Abstract
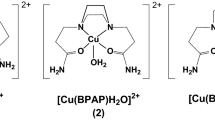
In the present study, cytotoxic effects of cisplatin, the most usually used chemotherapeutic agent, were compared with new designed platinum(IV) ([PtCl4(en)] (en = ethylenediamine) and [PtCl4(dach)]) (dach = (±)-trans-1,2-diaminocyclohexane) and platinum(II) complexes ([{trans-Pt(NH3)2Cl}2(μ-pyrazine)](ClO4)2 (Pt1), [{trans-Pt(NH3)2Cl}2(μ-4,4′-bipyridyl)](ClO4)2DMF(Pt2),[{trans-Pt(NH3)2Cl}2(μ-1,2-bis(4pyridyl)ethane)](ClO4)2 (Pt3)), in vitro and in vivo against human and murine lung cancer cells, to determine anti-tumor potential of newly synthesized platinum-based drugs in the therapy of lung cancer. Results obtained by MTT [3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide], Lactate dehydrogenase and Annexin V/Propidium Iodide assays showed that, among all tested complexes, [PtCl4(en)] had the highest cytotoxicity against human and murine lung carcinoma cells in vitro. [PtCl4(en)] showed significantly higher cytotoxicity then cisplatin in all tested concentrations, mainly by inducing apoptosis in lung cancer cells. [PtCl4(en)] was well tolerated in vivo. Clinical signs of [PtCl4(en)]-induced toxicity, such as changes in food, water consumption or body weight, nephrotoxicity or hepatotoxicity was not observed in [PtCl4(en)]-treated mice. [PtCl4(en)] managed to increase presence of CD45+ leukocytes, including F4/80+ macrophages, CD11c+ dendritic cells, CD4+ helper and CD8+ cytotoxic T cells (CTLs) in the lungs, cytotoxic NK, NKT and CTLs in the spleens of tumor bearing mice, resulting with reduction of metastatic lesions in the lungs, indicating its potential to stimulate anti-tumor immune response in vivo. Due to its anti-tumor cytotoxicity, biocompatibility, and potential for stimulation of anti-tumor immune response, [PtCl4(en)] may be a good candidate for further testing in the field of medicinal chemistry.





Similar content being viewed by others
References
Abu-Surrah AS, Kettunen M (2006) Platinum group antitumor chemistry: design and development of new anticancer drugs complementary to cisplatin. Curr Med Chem 13:1337–1357
Kozubík A, Vaculová A, Soucek K, Vondrácek J, Turánek J, Hofmanová J (2008) Novel anticancer platinum(IV) complexes with adamantylamine: their efficiency and innovative chemotherapy strategies modifying lipid metabolism. Met Based Drugs 2008:417897
Florea AM, Büsselberg D (2011) Cisplatin as an anti-tumor drug: cellular mechanisms of activity, drug resistance and induced side effects. Cancers (Basel) 3:1351–1371
Galluzzi L, Senovilla L, Vitale I, Michels J, Martins I, Kepp O, Castedo M, Kroemer G (2012) Molecular mechanisms of cisplatin resistance. Oncogene 31:1869–1883
Boulikas T (2007) Molecular mechanisms of cisplatin and its liposomally encapsulated form, Lipoplatin™. Lipoplatin™ as a chemotherapy and antiangiogenesis drug. Cancer Therapy 5:351–376
Bugarčić ŽD, Bogojeski J, Petrović B, Hochreuther S, van Eldik R (2012) Mechanistic studies on the reactions of platinum(II) complexes with nitrogen- and sulfur-donor biomolecules. Dalton Trans 41:12329–12345
Fanelli M, Formica M, Fusi V, Giorgi L, Micheloni M, Paoli P (2016) New trends in platinum and palladium complexes as antineoplastic agents. Coord Chem Rev 310:41–79
Rubino S, Pibiri I, Costantino C, Buscemi S, Girasolo MA, Attanzio A, Tesoriere L (2016) Synthesis of platinum complexes with 2-(5-perfluoroalkyl-1,2,4-oxadiazol-3yl)-pyridine and 2-(3-perfluoroalkyl-1-methyl-1,2,4-triazole-5yl)-pyridine ligands and their in vitro antitumor activity. J Inorg Biochem 155:92–100
Gay M, Montaña ÁM, Batalla C, Mesas JM, Alegre MT (2015) Design, synthesis and SAR studies of novel 1,2-bis(aminomethyl)cyclohexane platinum(II) complexes with cytotoxic activity. Studies of interaction with DNA of iodinated seven-membered 1,4-diaminoplatinocycles. J Inorg Biochem 142:15–27
Galanski M, Jakupec MA, Keppler BK (2005) Update of the preclinical situation of anticancer platinum complexes: novel design strategies and innovative analytical approaches. Curr Med Chem 12:2075–2094
Arsenijevic M, Milovanovic M, Volarevic V, Canovic D, Arsenijevic N, Soldatovic T, Jovanovic S, Bugarcic ZD (2012) Cytotoxic properties of platinum(IV) and dinuclear platinum(II) complexes and their ligand substitution reactions with guanosine-5′-monophosphate. Trans Met Chem. 37:481–488
Sequist LV, Waltman BA, Dias-Santagata D et al (2011) Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med 3:75ra26
Siegel R, Ward E, Brawley O et al (2011) Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin 61:212–236
Didkowska J, Wojciechowska U, Mańczuk M, Łobaszewski J (2016) Lung cancer epidemiology: contemporary and future challenges worldwide. Ann Transl Med 4:150
Khokhar AR, Xu Q, Al-Baker S (1993) X-ray crystal structure of tetrachloro(trans-d, l-1,2-diaminocyclohexane)platinum(IV) complex: a potential anticancer agent. J Inorg Biochem 52:51–58
Jovanović S, Petrović B, Bugarčić ŽD (2010) UV–Vis, HPLC, and 1H-NMR studies of the substitution reactions of some Pt(IV) complexes with 5′-GMP and l-histidine. J Coord Chem 63:2419–2430
Soldatović T, Jovanović S, Bugarčić ŽD, van Eldik R (2012) Substitution behaviour of novel dinuclear Pt(II) complexes with bio-relevant nucleophiles. Dalton Trans 41:876–884
Bertram JS, Janik P (1980) Establishment of a cloned line of Lewis lung carcinoma cells adapted to cell culture. Cancer Lett 11:63–73
Gerlier D, Thomasset N (1986) Use of MTT colorimetric assay to measure cell activation. J Immunol Methods 94:57–63
Mosmann T (1983) Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods 65:55–63
Shounan Y, Feng X, O’Connell PJ (1998) Apoptosis detection by annexin V binding: a novel method for the quantitation of cell-mediated cytotoxicity. J Immunol Methods 217:61–70
Tsai MS, Chang CC, Kuo ML, Wu YT (2011) Vascular endothelial growth factor-A and changes in a tumor-bearing mouse model with Lewis lung cancer. Oncol Lett 2:1143–1147
Tsai MS, Kuo ML, Chang CC, Wu YT (2013) The effects of exercise training on levels of vascular endothelial growth factor in tumor-bearing mice. Cancer Biomark 13:307–313
Okada T, Kurabayashi A, Akimitsu N, Furihata M (2017) Expression of cadherin-17 promotes metastasis in a highly bone marrow metastatic murine breast cancer model. Biomed Res Int 2017:8494286
Amaral EP, Ribeiro SC, Lanes VR, Almeida FM, de Andrade MR, Bomfim CC, Salles EM, Bortoluci KR, Coutinho-Silva R, Hirata MH, Alvarez JM, Lasunskaia EB, D’Império-Lima MR (2014) Pulmonary infection with hypervirulent Mycobacteria reveals a crucial role for the P2X7 receptor in aggressive forms of tuberculosis. PLoS Pathog 10:e1004188
Volarevic V, Milovanovic M, Ljujic B, Pejnovic N, Arsenijevic N, Nilsson U, Leffler H, Lukic ML (2012) Galectin-3 deficiency prevents concanavalin A-induced hepatitis in mice. Hepatology 55:1954–1964
Wang S, Zhang X, Ju Y, Zhao B, Yan X, Hu J, Shi L, Yang L, Ma Z, Chen L, Liu Y, Duan Z, Chen X, Meng S (2013) MicroRNA-146a feedback suppresses T cell immune function by targeting Stat1 in patients with chronic hepatitis B. J Immunol 191:293–301
Cubo L, Hambley TW, Sanz Miguel PJ, Carnero A, Navarro-Ranninger C, Quiroga AG (2011) The preparation and characterization of trans-platinum(IV) complexes with unusually high cytotoxicity. Dalton Trans 40:344–347
Cohen SM, Lippard SJ (2001) Cisplatin: from DNA damage to cancer chemotherapy. Prog Nucleic Acid Res Mol Biol 67:93–130
Wheate NJ, Walker S, Craig GE, Oun R (2010) The status of platinum anticancer drugs in the clinic and in clinical trials. Dalton Trans 39:8113–8127
Yao X, Panichpisal K, Kurtzman N, Nugent K (2007) Cisplatin nephrotoxicity: a review. Am J Med Sci 334:115–124
Heffeter P, Jungwirth U, Jakupec M, Hartinger C, Galanski M, Elbling L, Micksche M, Keppler B, Berger W (2008) Resistance against novel anticancer metal compounds: differences and similarities. Drug Resist Updat 11:1–16
Kelland L (2007) The resurgence of platinum-based cancer chemotherapy. Nat Rev Cancer 7:573–584
Jakupec MA, Galanski M, Arion VB, Hartinger CG, Keppler BK (2008) Antitumour metal compounds: more than theme and variations. Dalton Trans 2:183–189
Di Nicola M, Lemoli RM (2000) Dendritic cells: specialized antigen presenting cells. Haematologica 85:202–207
Terhune J, Berk E, Czerniecki BJ (2013) Dendritic cell-induced Th1 and Th17 cell differentiation for cancer therapy. Vaccines (Basel) 1:527–549
Fricke I, Gabrilovich DI (2006) Dendritic cells and tumor microenvironment: a dangerous liaison. Immunol Invest 35:459–483
Liao YP, Schaue D, McBride WH (2007) Modification of the tumor microenvironment to enhance immunity. Front Biosci 12:3576–3600
Kiraz Y, Baran Y, Nalbant A (2016) T cells in tumor microenvironment. Tumour Biol 37:39–45
Kouchi Y, Maeda Y, Ohuchida A, Ohsawa M (1996) Immunotoxic effect of low dose cisplatin in mice. J Toxicol Sci 21:227–233
Hassan MI, Ahmed MI, Kassim SK, Rashad A, Khalifa A (1999) Cis-platinum-induced immunosuppression: relationship to melatonin in human peripheral blood mononuclear cells. Clin Biochem 32:621–626
Kennedy R, Celis E (2008) Multiple roles for CD4+ T cells in anti-tumor immune responses. Immunol Rev 222:129–144
Andersen MH, Schrama D, Thor Straten P, Becker JC (2006) Cytotoxic T cells. J Invest Dermatol 126:32–41
Brutkiewicz RR, Sriram V (2002) Natural killer T (NKT) cells and their role in antitumor immunity. Crit Rev Oncol Hematol 41:287–298
Muntasell A, Ochoa MC, Cordeiro L, Berraondo P, López-Díaz de Cerio A, Cabo M, López-Botet M, Melero I (2017) Targeting NK-cell checkpoints for cancer immunotherapy. Curr Opin Immunol 45:73–81
Acknowledgements
This work was supported by grants from the Ministry of Education, Science and Technological Development, Republic of Serbia (Projects ON175069, ON175103 and 172011).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Arsenijevic, M., Milovanovic, M., Jovanovic, S. et al. In vitro and in vivo anti-tumor effects of selected platinum(IV) and dinuclear platinum(II) complexes against lung cancer cells. J Biol Inorg Chem 22, 807–817 (2017). https://doi.org/10.1007/s00775-017-1459-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00775-017-1459-y