Abstract
Introduction
A 2015 study showed a decreasing trend in the incidence of osteoporotic hip fractures in Niigata Prefecture, Japan, which had been increasing. This study aimed to investigate the incidence of osteoporotic hip fractures in 2020, determine the long-term change in the incidence of hip fractures from 1985 to 2020, and assess whether the decline in fracture incidence since 2010 has continued.
Materials and Methods
We obtained data from the registration forms submitted by hospitals and clinics of patients who lived in Niigata Prefecture and were diagnosed with osteoporotic hip fracture through a survey conducted from January 1, 2020 to December 31, 2020.
Results
In 2020, 3,369 hip fractures were recorded in Niigata Prefecture. Although the overall incidence of age-specific hip fractures decreased, it increased in patients aged ≥ 90 years, regardless of sex. The proportion of patients receiving anti-osteoporosis drugs prior to hip fracture increased from 7.6% in 2004 to 17.3% in 2020. Notably, surgical treatment should be performed as early as possible, and the preoperative waiting time was 2.9 days, which was mainly due to holidays.
Conclusion
The incidence of hip fractures in Niigata Prefecture has gradually increased over the past 35 years, with an increasing change observed in the very elderly recently in 2020. Although the treatment of osteoporotic hip fractures in Niigata Prefecture is adequate, improvements may include increasing the rate of adoption of osteoporosis treatment further and decreasing the number of days of preoperative waiting.
Similar content being viewed by others
Introduction
With the increase in life expectancy worldwide, fragility fractures, associated with osteoporosis in the aging population, are becoming more common, resulting in a reduced quality of life [1], severe morbidity, and increased mortality [2]. Hip fractures are considered one of the most damaging osteoporotic fractures in the elderly [3]. Assuming that age-specific fracture rates remain constant, the incidence of hip fractures is expected to continue to increase as the global elderly population increases [4, 5].
The elderly population is increasing annually in Japan. In 2020, there were 36.21 million elderly people aged ≥ 65 years, accounting for 28.8% of the total Japanese population [6]. The estimated incidence of osteoporotic hip fractures in Japan has increased every year from 1986 to 2017 [7,8,9,10], with 200,000 incidents reported annually, and is expected to continue to increase in the future. We have studied the incidence of osteoporotic hip fractures in Niigata Prefecture, Japan, approximately every 5 years since 1985. Based on the results of the Niigata Osteoporotic Hip Fracture Study, we previously reported that the incidence of proximal femoral fragility fractures in Niigata Prefecture, Japan, increased between 1985 and 2010 and decreased between 2010 and 2015 [3, 11,12,13,14,15]. We attribute this decrease to the widespread use of osteoporosis treatment [3].
This study aimed to investigate the incidence of hip fractures in Niigata Prefecture in 2020, clarify the long-term trend of hip fracture incidence from 1985 to 2020, and evaluate whether the decrease in fracture incidence since 2010 has continued. By investigating the characteristics of fractures and their treatment, we also assessed whether the recommended and appropriate prevention and treatment are being conducted in Niigata Prefecture.
Materials and methods
In accordance with all previous surveys, registration forms were sent to all orthopedic clinics and hospitals in Niigata Prefecture to be filled in with information on patients admitted for hip fracture [3, 11,12,13,14,15]. In recent years, extensive data, such as receipt data and disease name search systems data, have been used in many cases, but considering the content and scale of this survey, we decided to collect the data using survey forms, as in previous surveys [16]. In Japan, most citizens are covered by the National Health Insurance or Employees' Pension Insurance [17].
The data collected in this study were from all patients who lived in Niigata Prefecture and were diagnosed with osteoporotic hip fracture from January 1, 2020, to December 31, 2020. Osteoporotic fractures were defined as fractures caused by small external forces, such as falls from a height lower than the standing-up position. All fractures were classified as femoral neck or femoral trochanteric fractures. Fractures at the base of the femoral neck and subtrochanteric fractures were classified as trochanteric fractures. A total of 25 orthopedic clinics and 48 hospitals in Niigata city and Prefecture, respectively, participated in this study. In addition, access to the data from these hospitals and clinics was provided during the study period. Patients who did not receive orthopedic care; lived in other prefectures; were younger than 60 years; had fractures of the femoral diaphysis, pathological fractures, periprosthetic fractures, and fractures due to high-energy trauma; and refused to participate in the study or research were excluded. The enrollment forms were returned to the hospital after completion.
The study was designed in accordance with the Declaration of Helsinki, and was approved by the Ethics Review Board of Niigata University Graduate School of Medical and Dental Science (No. 2018–0341). As this was a retrospective study, the requirement to obtain informed consent was waived.
In November 2020, there were 2,198,210 persons in Niigata Prefecture; 1,066,494 were male, and 1,131,716 were female. The number of people aged ≥ 65 years was 721,618, with 312,009 male and 409,609 female patients, which accounted for 32.8% of the total population of Niigata Prefecture [18]. Table 1 shows the total population and the elderly population (≥ 65 years old) of Niigata Prefecture in each survey year.
In this study, we classified all patients with hip fractures according to their age at 5-year intervals, sex (male or female), and fracture type (neck or trochanteric). During this study period, patients with bilateral hip fractures who sustained two injuries simultaneously or separately were counted in duplicate. Twenty-three patients experienced bilateral hip fractures during the study period. We previously conducted studies on the incidence of fragility hip fractures that occurred in Niigata Prefecture in 1985, 1987, 1989, 1994, 1999, 2004, 2010, and 2015 [3, 11,12,13,14,15]. The incidence of hip fractures at 5-year age intervals in the 2020 study was calculated as the annual number of fractures per 100,000 people. All the data obtained in previous studies were compared with that obtained in 2020, except for a study conducted in 1987, to standardize the figures for every 5 years. For each survey year, the standardized incidence rates were adjusted to the proportion of the Japanese population aged ≥ 60 years in 1985.
In accordance with previous studies [19], statistical tests for overall change were performed by comparing the incidence rates for each study year using the Mantel–Haenszel extended Chi-square test [20] and joinpoint trend analysis was used to evaluate long-term trends over time [21, 22]. First, we evaluated age-specific change during the study period. The age-adjusted hip fracture change was shown by combining all age-specific results of the Mantel test. Statistical significance was set at p < 0.05. These statistical analyses were performed using Microsoft Excel 2013 (Microsoft Corp., Redmond, WA, USA).
Patients were also surveyed regarding the place where the fracture occurred (indoor or outdoor), presence or absence of pre-injury osteoporosis treatment interventions, treatment method (conservative therapy, surgical treatment; osteosynthesis, hemiarthroplasty/total hip arthroplasty, other), and preoperative waiting time. A comparison of the results of the 2015 survey was assessed using the Chi-square test to determine whether the place of injury was indoor or outdoor. If the preoperative waiting time was > 48 h, reasons for the delay were selected from (1) holiday, (2) convenience of the operating room and anesthesiology department, (3) convenience of the orthopedic department, (4) medical comorbidity, and (5) several days had already passed at the time of consultation. Multiple answers were allowed.
Results
The details of all the fractures are shown in Table 2. In Niigata Prefecture in 2020, the total number of hip fractures was 3,369 (661 males, mean age: 82.7 years; 2,708 females, mean age: 86.4 years), with a male-to-female ratio of 1:4.1 (Table 2). In patients aged ≥ 60 years, the incidence of hip fracture per 100,000 individuals was 388 per year. The percentages of total hip fractures in patients aged ≥ 65 years, ≥ 85 years, and ≥ 90 years were 98.0, 63.1, and 36.9% respectively (Table 3). The 2015 survey showed that the percentages of patients aged ≥ 65 years, ≥ 85 years, and ≥ 90 years were 98.0, 56.6, and 29.1%, with a notable decrease in fractures in people aged ≥ 85 years and ≥ 90 years compared to the current study.
A survey of indoor and outdoor incidence locations was also conducted in 2015, and a Chi-square test showed that indoor incidences were significantly higher and outdoor incidences were significantly lower in 2020 (χ2(1) = 5.879, p < 0.05) (Table 2). A total of 3,110 patients underwent surgery, and 259 underwent conservative treatment. The average preoperative waiting time was 2.9 days, and 49.6% of the patients underwent surgery within 48 h. The reasons for waiting periods of ≥ 48 h were as follows: 40.4% were due to “holidays,” 23.0% were due to “convenience of the operating room and anesthesiology department,” 20.1% were due to “several days had already passed at the time of consultation,” 12.8% were due to “medical comorbidities,” and 7.6% were due to “convenience of the orthopedic department.” Delays in surgeries due to COVID-19-related issues, such as "awaiting PCR test results for COVID-19" and "isolation measures due to fever," accounted for 1.9% (Table 4).
The percentage of patients taking anti-osteoporotic medications prior to hip fracture was 7.6% in 2004, 10.2% in 2010, and 14.9% in 2015, compared to 17.3% in 2020. Anti-osteoporotic medications included bisphosphonates, selective estrogen receptor modulators, vitamin D, teriparatide, denosumab (anti-RANKL antibody), and calcium preparations, which were used in 199, 69, 399, 25, 15, and 33 patients, respectively.
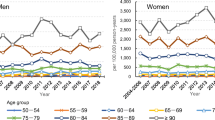
We investigated long-term change of the incidence of hip fractures in Niigata Prefecture from 1985 to 2020. Figs. 1, 2 show the incidence of hip fractures according to age and sex during the survey.
Long-term changes in the age-specific incidence of hip fractures in men from 1985 to 2020. In most age groups, the incidence of hip fractures peaked between 2004 and 2010 and then began to decrease. The incidence of hip fractures in the very elderly (≥ 85 years) peaked in 2004 and began to decrease but then increased slightly in 2020
Long-term changes in the age-specific incidence of hip fractures in women from 1985 to 2020. Except for those aged 60–64 years, the incidence of hip fractures peaked in 2010. In most age groups, there was a decreasing trend after the peak, but those aged ≥ 90 years showed an increasing trend in 2020
The age-specific incidence of hip fractures in males increased since 1985, peaked between 2004 and 2010 in most age groups, and then began to decline. The incidence of hip fractures in the very elderly (≥ 85 years) peaked in 2004 and began to decrease but increased slightly in 2020. In the very elderly, the degree of increase in the fracture rate was greater in those aged ≥ 90 years than in those aged 85–89 years; those who showed an increasing change in 2020 were aged 75–79 years, 85–89 years, and ≥ 90 years.
The age-specific incidence of hip fractures in females and males increased from 1985 to 2010 and declined after 2010. In 2010, the peak year, the incidence of hip fracture for all age groups was the highest, except for those aged 60–64 years. In most age groups, there was a decreasing trend after the peak, but those aged ≥ 90 years showed a slightly increasing in 2020. Patients aged 65–69 years and ≥ 90 years showed an increasing in 2020.
We adjusted the changes during the study period of the age- and sex-specific incidence rates for each investigative year using the Japanese population composition of 1985 (Fig. 3). For females, the incidence rate increased every year, except 1999, before 2010, but was highest in 2010 and then significantly lower in 2015 and 2020 in comparison (p < 0.001). In males, as in females, the incidence increased in all years except 1994, but was highest in 2010 and then significantly lower in 2015 and 2020 in comparison (p < 0.001); however, there was no significant difference between the incidence in 2020 and in 1994 (p = 0.633).
Trends in the incidence of hip fractures by sex using the population structure of Japan in 1985. Comparing the figures alone, it appears that the incidence rate for both males and females gradually increased since the start of the survey until 2010 and has gradually trended downward since then; however, future progress needs to be monitored to determine an actual decrease over time
When the long-term trend, age-specific trend, and sex-specific trend were evaluated using joinpoint trends, it was clear that the incidence rate of women 80–84 and women 90 and older peaked in 2010, men 80–84 peaked in 1999, and men 85–89 peaked in 2004, showing a decrease over time. However, the overall change over time did not indicate that 2010 was a major peak. Therefore, although this analysis indicated that a few age groups displayed a declining trend after peaking in 2010, 2010 could not be considered the peak year when measuring the overall trend.
Discussion
In this survey, compared to 2015, the number of fractures increased slightly, but the fracture rate did not change significantly. Since 1985, in Niigata Prefecture, the fracture rate for males and females was on an increasing until 2010, after which it began to decline; however, in this survey, the rate remained unchanged.
In the 1990s, Cooper et al. [4] and Cauley et al. [5] estimated that between 4.5 and 6.26 million hip fractures would occur worldwide by 2050 but that the proportion in North America and Europe would decrease to approximately a quarter, and half would be in Asia. Between 1995 and 2010, several studies reported a reduction in the incidence of hip fractures in the US and Europe [23,24,25,26,27,28]. Previous studies have attributed the decrease in the incidence of hip fractures to fall-preventive measures for older adults, lifestyle changes, screening by bone density test, osteoporotic therapy, an improved nutritional status, and a decreased use of psychiatric drugs to reduce fall risk [20, 23,24,25,26,27]. On the other hand, in the US, it has been reported that the degree of decrease in the fracture rate has slowed since 2013 [28]. Some reports in Asia have shown an increase [29], while others have shown a plateau to a decreasing trend [30, 31]. In Japan, the number and incidence of new hip fractures are steadily increasing [7, 9, 32]. According to a study by Sakuma et al. [33] in Sado Island, Niigata Prefecture, the incidence of hip fractures increased from 2004 to 2006 but did not change significantly from 2006 to 2010. Hagino et al. also reported that the incidence of hip fractures in Tottori Prefecture increased until 2018 for males, whereas it did not increase after 2010 for females [34]. While some reports, such as these, show that the incidence of hip fractures did not increase, most reports indicate that the incidence of hip fractures continues to increase [7, 35, 36]. The incidence of hip fractures in Niigata Prefecture increased for both males and females from 1985 to 2010. The age- and sex-specific incidence rates showed that the incidence of hip fractures in 2020 decreased in all age groups except 75–79, 85–89, and ≥ 90 years for males and 65–69 and ≥ 90 years for females; however, it cannot be said that the trend has yet turned downward, and future trends should be observed in the next Niigata Prefecture Osteoporotic Hip Fracture Study. In this study, since the incidence rate was calculated by adjusting for the population in 1985, it is considered that the increase in the elderly population is not expected to affect the trend in the incidence of hip fracture.
Using the population structure of Japan from 1985 to 2020, we reported the incidence rates by sex and age for each survey year (Fig. 3). For both sexes, there was a temporary decrease in the incidence of hip fractures in 1999 and a gradual increase until 2010, after which the incidence seemed to begin to decrease. In males, no significant differences were observed between 1999 and 2020. Several studies have reported that a deficiency of calcium and other nutrients in childhood and adolescence increases osteoporosis in adulthood and affects the incidence of hip fracture [37, 38]. According to Sakuma et al., vitamin D deficiency and hip fractures are closely related [39, 40]. Morita et al. reported a high proportion of frail, elderly people who were alive in the 1940s [14]. As currently older adults (≥ 85 years) grew up in the 1940s during and after World War II and experienced nutritional deficiencies during that period, it is likely that the proportion of frail older adults is high as Morita et al. [14] suggested, and thus the fracture rate may have increased in that age group. This is consistent with the results of this and our previous studies [3, 11,12,13,14,15].
This study additionally confirmed that the number of patients treated with osteoporosis drugs, prior to hip fracture, increased by 7.1% between 2010 and 2020 and by 2.4% between 2015 and 2020. These results may suggest that, as well as an increase in the osteoporosis treatment rate among fracture patients in Niigata Prefecture, there may have been an increase in the proportion of the general population without fractures taking osteoporosis medication, which may have led to a decrease in hip fractures, which had been gradually rising between 1999 and 2010. Orimo et al. [9] stated that the number of hip fractures has increased, although the incidence may have decreased in some age groups in both sexes. They reported that the use of a wide variety of osteoporosis drugs, especially bisphosphonates, to treat osteoporosis and prevent hip fractures may have contributed to the decreased incidence rate. A long-term decrease in the incidence of hip fractures has been reported in North American and European populations [23,24,25,26,27,28]. This decrease is mainly due to the increased use of osteoporosis drugs, especially bisphosphonates. They also reported that the rate of decline is slowing in the US, which may be due to a decrease in the rate of osteoporosis screening and bisphosphonate use [28]. In Japan, the number of patients with osteoporosis is approximately 13 million, but only 20–25% of all patients are treated with osteoporosis drugs. In Niigata Prefecture, the number of patients receiving osteoporosis drug treatment prior to hip fractures is gradually increasing, reaching 17.3% in the 2020 survey. However, only 199 of the 3,369 patients (approximately 6%) were taking bisphosphonates. Based on these results, focus should be emphasized on osteoporosis treatment, and the rate of taking osteoporosis medications should be increased. Fracture liaison services (FLSs) have become widespread to prevent secondary fractures in North American and European countries, however, there were only six such institutions in Niigata Prefecture. FLS may help reduce costs and provide quality care, resulting in a lower risk of subsequent fractures [41]. Similarly, the Osteoporosis Society of Japan established an osteoporosis liaison service in 2012 that recommends osteoporosis medications for patients at a high risk of fracture to reduce the risk and incidence of hip fracture. Soon, the incidence of hip fractures in Japan may decrease through these efforts [9].
In 2020, 2,623 fractures occurred indoors, and 562 occurred outdoors. In the 2015 survey, 2349 fractures occurred indoors, and 591 occurred outdoors. In 2020, there were significantly more indoor fractures and fewer outdoor fractures than those in 2015. The global COVID-19 pandemic occurred in 2020, which may have affected the results. Regarding orthopedic injuries during the pandemic, the decrease in outdoor fractures, including those related to traffic accidents and sports, and the proportion of indoor-onset fractures increased, which could be due to lockdown and travel restrictions [42, 43]. Similar changes to those reported in this study were observed, and the location of Niigata Prefecture-onset fragility fractures in 2020, during the global COVID-19 pandemic, may have been affected by the declaration of emergency and curfews issued throughout Japan.
Regarding the timing of treatment, the American Academy of Orthopedic Surgeons guidelines [44] recommend surgery within 48 h, and the Guidelines by the Japanese Orthopedic Association [45] recommend surgery as soon as possible. Hagino et al. reported that the mean preoperative hospital stay in Japan was 4.8 days in 2009, 4.5 days in 2014 [46], and 4.1 days in 2018 [47]. Sasabuchi [48] et al. reported that 22.5% of patients underwent surgery within 2 days. In this study, the average preoperative waiting time was 2.9 days, and 49.6% of the patients underwent surgery within the waiting period of 48 h. Compared to the overall report for Japan, this is shorter than the average preoperative hospital stay; although many patients underwent surgery within 48 h, wait time still needs to be shortened.
Hagino et al. [46] reported that the most common reason for a delay in surgery was difficulty securing operating rooms (50.2%), followed by complications (24.5%), securing an anesthesiologist (24.2%), use of anticoagulants (22.4%), and securing a surgeon (19.2%). The most common reason in this study was ‘holiday break’. Measures, such as securing surgical scheduling and anesthesiology, encouraging prompt consultation, and controlling medical comorbidities, may allow many patients to be operated on within 48 h in the future. Imai et al. [49] reported that a multidisciplinary approach, such as FLS, significantly reduced the time from injury to surgery from 2.42 days to 1.83 days for patients with proximal femur fractures. Early interventions by internists, through multidisciplinary approaches, may lead to the faster approval and scheduling of surgery and a reduction in medical complications.
A limitation of this study is that the younger age groups (< 59 years) were excluded. According to Morita et al. [14], in a 1999 study, the number of young patients who had hip fractures under the age of 49 was approximately 2% of the total, which was not very high. On the other hand, one of the strengths of this study is that almost all patients with hip fractures were seen by orthopedic surgeons in Niigata Prefecture, although some of the hip fracture patients were seen by other medical institutions that do not have orthopedic departments. Dohmae et al. [12] suggested that patients with new hip fractures and who visited medical institutions other than orthopedic surgery were approximately 2% of all patients with hip fractures in Niigata Prefecture. The number of neglected patients in this survey was estimated to be small because the same methodology was used in the 1989 survey. Regarding the rate of adoption of osteoporosis treatment, the actual overall rate of adoption of osteoporosis treatment was not calculated because we are investigating whether the patients had interventions before the fracture.
In conclusion, there was no significant change in the incidence of hip fractures in Niigata Prefecture in 2020 compared with that in 2015 for both males and females. In terms of the age-specific incidence, fractures among the “very elderly”, aged > 85 years resulted in an increasing change in both males and females, while those aged < 85 years showed a decreasing change. However, when assessing the trends overall, we observed that the incidence rate did not peak in 2010 and therefore, future studies should clarify this aspect. Moreover, it is necessary to improve the treatment of osteoporotic hip fractures by increasing the rate of adoption of osteoporosis treatment further and decreasing the number of days of the preoperative waiting time.
References
Amarilla-Donoso FJ, López-Espuela F, Roncero-Martín R, Leal-Hernandez O, Puerto-Parejo LM, Aliaga-Vera I, Toribio-Felipe R, Lavado-García JM (2020) Quality of life in elderly people after a hip fracture: a prospective study. Health Qual Life Outcomes 18:71. https://doi.org/10.1186/s12955-020-01314-2
Panula J, Pihlajamäki H, Mattila VM, Jaatinen P, Vahlberg T, Aarnio P, Kivelä SL (2011) Mortality and cause of death in hip fracture patients aged 65 or older: a population-based study. BMC Musculoskelet Disord 12:105. https://doi.org/10.1186/1471-2474-12-105
Imai N, Endo N, Shobugawa Y, Ibuchi S, Suzuki H, Miyasaka D, Sakuma M (2018) A decrease in the number and incidence of osteoporotic hip fractures among elderly individuals in Niigata, Japan, from 2010 to 2015. J Bone Miner Metab 36:573–579. https://doi.org/10.1007/s00774-017-0863-2
Cooper C, Campion G, Melton LJ 3rd (1992) Hip fractures in the elderly: a world-wide projection. Osteoporos Int 2:285–289. https://doi.org/10.1007/BF01623184
Cauley JA, Chalhoub D, Kassem AM, Gel-H F (2014) Geographic and ethnic disparities in osteoporotic fractures. Nat Rev Endocrinol 10:338–351. https://doi.org/10.1038/nrendo.2014.51
Statistics Bureau (2020) Ministry of Internal Affairs and communications. https://www.stat.go.jp/data/jinsui/pdf/202011.pdf. Government of Japan. Accessed 1 Nov 2021
Hagino H, Furukawa K, Fujiwara S, Okano T, Katagiri H, Yamamoto K, Teshima R (2009) Recent trends in the incidence and lifetime risk of hip fracture in Tottori, Japan. Osteoporos Int 20:543–548. https://doi.org/10.1007/s00198-008-0685-0
Hagino H, Sakamoto K, Harada A, Nakamura T, Mutoh Y, Mori S, Endo N, Nakano T, Itoi E, Kita K, Yamamoto N, Aoyagi K, Yamazaki K (2010) Nationwide one-decade survey of hip fractures in Japan. J Orthop Sci 15:737–745. https://doi.org/10.1007/s00776-010-1543-4
Orimo H, Yaegashi Y, Hosoi T, Fukushima Y, Onoda T, Hashimoto T, Sakata K (2016) Hip fracture incidence in Japan: estimates of new patients in 2012 and 25-year trends. Osteoporos Int 27:1777–1784. https://doi.org/10.1007/s00198-015-3464-8
Takusari E, Sakata K, Hashimoto T, Fukushima Y, Nakamura T, Orimo H (2021) Trends in hip fracture incidence in Japan: estimates based on nationwide hip fracture surveys from 1992 to 2017. JBMR Plus. 5:10428. https://doi.org/10.1002/jbm4.10428
Kawashima T (1989) Epidemiology of the femoral neck fracture in 1985, Niigata Prefecture, Japan. J Bone Miner Metab 7:46–54. https://doi.org/10.1007/BF02911534
Dohmae Y, Takahashi HE, Kawashima T (1991) Epidemiology of femoral neck fracture in 1989, Niigata Prefecture, Japan. A comparison with the incidence in 1985 and 1987. J Bone Miner Metab 9:94–98. https://doi.org/10.1007/BF02375927
Iga T, Dohmae Y, Endo N, Takahashi HE (1999) Increase in the incidence of cervical and trochanteric fractures of the proximal femur in Niigata Prefecture, Japan. J Bone Miner Metab 17:224–231. https://doi.org/10.1007/s007740050089
Morita Y, Endo N, Iga T, Tokunaga K, Ohkawa Y (2002) The incidence of cervical and trochanteric fractures of the proximal femur in 1999 in Niigata Prefecture, Japan. J Bone Miner Metab 20:311–318. https://doi.org/10.1007/s007740200045
Miyasaka D, Endo N, Endo E, Sakuma M, Yamamoto N, Tanabe N, Imai N, Suda K (2016) Incidence of hip fracture in Niigata, Japan in 2004 and 2010 and the long-term trends from 1985 to 2010. J Bone Miner Metab 34:92–98. https://doi.org/10.1007/s00774-015-0648-4
Nozaki A, Imai N, Suzuki H, Endo N (2020) Differences in accuracy of patient collection between survey forms and disease retrieval systems. Arch Niigata Soc Orthop Surg 36:57–60
Ministry of Health, Labour and Welfare, Japan (2021) National health insurance. https://www.mhlw.go.jp/bunya/iryouhoken/iryouhoken01/dl/01_eng.pdf. Accessed 1 Nov 2021
General Affairs Division, Niigata Prefecture Government (2020) Niigata Prefecture population estimates. https://www.pref.niigata.lg.jp/site/tokei/jinkou20201001.html. Accessed 1 Nov 2021
Sneyd MJ, Cox B (2013) A comparison of trends in melanoma mortality in New Zealand and Australia: the two countries with the highest melanoma incidence and mortality in the world. BMC Cancer 13:372. https://doi.org/10.1186/1471-2407-13-372
Mantel N (1963) Chi-square tests with one degree of freedom; extensions of the Mantel-Haenszel procedure. J Am Stat Assoc 58:690–700. https://doi.org/10.1080/01621459.1963.10500879
Kim HJ, Fay MP, Feuer EJ, Midthune DN (2000) Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 19:335–351. https://doi.org/10.1002/(sici)1097-0258(20000215)19:3%3c335::aid-sim336%3e3.0.co;2-z
National Cancer Institute, Division of Cancer Control & Population Sciences (2020) Joinpoint trend analysis software. Accessed 24 Aug 2022
Mazzucchelli Esteban R, Pérez-Fernández E, Crespí-Villarías N, García-Vadillo A, Rodriguez-Caravaca G, Gil de Miguel A, Carmona L (2017) Trends in osteoporotic hip fracture epidemiology over a 17-year period in a Spanish population: Alcorcón 1999–2015. Arch Osteoporos 12:84. https://doi.org/10.1007/s11657-017-0376-6
Tarantino U, Piscitelli P, Feola M, Neglia C, Rao C, Gimigliano F, Iolascon G (2018) Decreasing trend of hip fractures incidence in Italy between 2007 and 2014: epidemiological changes due to population aging. Arch Osteoporos 13:23. https://doi.org/10.1007/s11657-018-0423-y
Unim B, Minelli G, Da Cas R, Manno V, Trotta F, Palmieri L, Galluzzo L, Maggi S, Onder G (2021) Trends in hip and distal femoral fracture rates in Italy from 2007 to 2017. Bone 142:115752. https://doi.org/10.1016/j.bone.2020.115752
Kannus P, Niemi S, Parkkari J, Sievänen H (2018) Continuously declining incidence of hip fracture in Finland: analysis of nationwide database in 1970–2016. Arch Gerontol Geriatr 77:64–67. https://doi.org/10.1016/j.archger.2018.04.008
Dimai HP, Reichardt B, Zitt E, Concin H, Malle O, Fahrleitner-Pammer A, Svedbom A, Brozek W (2022) Thirty years of hip fracture incidence in Austria: is the worst over? Osteoporos Int 33:97–104. https://doi.org/10.1007/s00198-021-06086-z
Lewiecki EM, Wright NC, Curtis JR, Siris E, Gagel RF, Saag KG, Singer AJ, Steven PM, Adler RA (2018) Hip fracture trends in the United States, 2002 to 2015. Osteoporos Int 29:717–722. https://doi.org/10.1007/s00198-017-4345-0
Kim BS, Lim JY, Ha YC (2020) Recent epidemiology of hip fractures in South Korea. Hip Pelvis 32:119–124. https://doi.org/10.5371/hp.2020.32.3.119
Zhang C, Feng J, Wang S, Gao P, Xu L, Zhu J, Jia J, Liu L, Liu G, Wang J, Zhan S, Song C (2020) Incidence of and trends in hip fracture among adults in urban China: a nationwide retrospective cohort study. PLOS Med 17:1003180. https://doi.org/10.1371/journal.pmed.1003180
Yong EL, Ganesan G, Kramer MS, Logan S, Lau TC, Cauley JA, Tan KB (2019) Hip fractures in Singapore: ethnic differences and temporal trends in the new millennium. Osteoporos Int 30:879–886. https://doi.org/10.1007/s00198-019-04839-5
Orimo H, Yaegashi Y, Onoda T, Fukushima Y, Hosoi T, Sakata K (2009) Hip fracture incidence in Japan: estimates of new patients in 2007 and 20-year trends. Arch Osteoporos 4:71–77. https://doi.org/10.1007/s11657-009-0031-y
Sakuma M, Endo N, Oinuma T, Miyasaka D, Oguma Y, Imao K, Koga H, Tanabe N (2014) Incidence of osteoporotic fractures in Sado, Japan in 2010. J Bone Miner Metab 32:200–205. https://doi.org/10.1007/s00774-013-0486-1
Hagino H, Osaki M, Okuda R, Enokida S, Nagashima H (2020) Recent trends in the incidence of hip fracture in Tottori Prefecture, Japan: changes over 32 years. Arch Osteoporos 15:152. https://doi.org/10.1007/s11657-020-00823-3
Koseki H, Sunagawa S, Noguchi C, Yonekura A, Matsumura U, Watanabe K, Nishiyama Y, Osaki M (2021) Incidence of and risk factors for hip fracture in Nagasaki, Japan from 2005 to 2014. Arch Osteoporos 16:111. https://doi.org/10.1007/s11657-021-00978-7
Arakaki H, Owan I, Kudoh H, Horizono H, Arakaki K, Ikema Y, Shinjo H, Hayashi K, Kanaya F (2011) Epidemiology of hip fractures in Okinawa, Japan. J Bone Miner Metab 29:309–314. https://doi.org/10.1007/s00774-010-0218-8
Reid IR, Chin K, Evans MC, Jones JG (1994) Relation between increase in length of hip axis in older women between 1950s and 1990s and increase in age specific rates of hip fracture. BMJ 309:508–509. https://doi.org/10.1136/bmj.309.6953.508
Baker SS, Cochran WJ, Flores CA, Georgieff MK, Jacobson MS, Jaksic T, Krebs NF, A Academy of Pediatrics Committee on Nutrition (1999) American academy of pediatrics. committee on nutrition. calcium requirements of infants, children, and adolescents. Pediatrics 104:1152–1157. https://doi.org/10.1542/peds.104.5.1152
Sakuma M, Endo N, Hagino H, Harada A, Matsui Y, Nakano T, Nakamura K (2011) Serum 25-hydroxyvitamin D status in hip and spine-fracture patients in Japan. J Orthop Sci 16:418–423. https://doi.org/10.1007/s00776-011-0089-4
Sakuma M, Endo N, Oinuma T, Hayami T, Endo E, Yazawa T, Watanabe K, Watanabe S (2006) Vitamin D and intact PTH status in patients with hip fracture. Osteoporos Int 17:1608–1614. https://doi.org/10.1007/s00198-006-0167-1
Curtis JR, Silverman SL (2013) Commentary: the five Ws of a Fracture Liaison Service: why, who, what, where, and how? In osteoporosis, we reap what we sow. Curr Osteoporos Rep 11:365–368. https://doi.org/10.1007/s11914-013-0177-9
Poggetti A, Del Chiaro A, Nucci AM, Suardi C, Pfanner S (2021) How hand and wrist trauma has changed during covid-19 emergency in Italy: incidence and distribution of acute injuries. What to learn? J Clin Orthop Trauma 12:22–26. https://doi.org/10.1016/j.jcot.2020.08.008
Lim MA, Mulyadi Ridia KG, Pranata R (2021) Epidemiological pattern of orthopaedic fracture during the COVID-19 pandemic: a systematic review and meta-analysis. J Clin Orthop Trauma 16:16–23. https://doi.org/10.1016/j.jcot.2020.12.028
Brox WT, Roberts KC, Taksali S, Wright DG, Wixted JJ et al (2015) The American Academy of Orthopaedic Surgeons evidence-based guideline on management of hip fractures in the elderly. J Bone Joint Surg Am 97:1196–1199. https://doi.org/10.2106/JBJS.O.00229
Watanabe Y, Matsushita T (2007) Management of hip fracture in older people: a clinical guideline in Japan 2005. Nihon Rinsho 65:43–49
Hagino H, Endo N, Harada A, Iwamoto J, Mashiba T, Mori S, Ohtori S, Sakai A, Takada J, Yamamoto T (2017) Survey of hip fractures in Japan: recent trends in prevalence and treatment. J Orthop Sci 22:909–914. https://doi.org/10.1016/j.jos.2017.06.003
Hagino H (2021) Epidemiology of proximal femur fractures and current status of early surgery. J Jpn Orthop Assoc 95:S362
Sasabuchi Y, Matsui H, Lefor AK, Fushimi K, Yasunaga H (2018) Timing of surgery for hip fractures in the elderly: a retrospective cohort study. Injury 49:1848–1854. https://doi.org/10.1016/j.injury.2018.07.026
Imai N, Endo N, Suda K, Suzuki H (2021) Multidisciplinary approach to reduce postoperative complications and improve the activity of patients with hip fracture a 24-month follow-up survey. Acta Med Okayama 75:595–600. https://doi.org/10.18926/AMO/62772
Acknowledgements
We would like to thank all the hospitals in the Niigata Prefecture and all the doctors and staff who contributed to this study. Without their cooperation, this study would not have been possible. We are especially grateful to the following (in alphabetical order): Agano City Hospital, Aoki Orthopedic Clinic, Aozora Niitsu Orthopedic Clinic, Hasegawa Orthopedic Clinic, Hokari Clinic, Honma Orthopedic Clinic, Ishizaka Orthopedic Clinic, Isizaki Clinic, Okawa Clinic, Itoigawa General Hospital, Joetsu Community Medical Center, Joetsu General Hospital, Kaetsu Hospital, Kameda Daiichi Hospital, Kashiwazaki General hospital and Medical Center, Katsumi Orthopedic Clinics, Kido Hospital, Kuwana Hospital, Kimura Orthopedic Clinic, Kinto Orthopedic Clinic, Kobayashi Orthopedic Clinic, Kon Orthopedic Clinic, Maniwa Orthopedic Clinic, Matsui Orthopedic Clinic, Midori Hospital, Minamiuonuma City Hospital, Mitsuke City Hospital, Murakami General Hospital, Nagaoka Central General Hospital, Nagaoka Nishi Hospital, Nagaoka Red Cross Hospital, Nagata Clinic, Nakajo Chuo Hospital, Nekoyama Miyao Hospital, Niigata Bandai Hospital, Niigata Central Hospital, Niigata-City Hospital, Niigata Medical Center, Niigata Minami Hospital, Niigata National Hospital, Niigata Prefectural Cancer Center Hospital, Niigata Prefectural Central Hospital, Niigata Prefectural Kamo Hospital, Niigata Prefectural Saiseikai Sanjo Hospital, Niigata Prefectural Shibata Hospital, Niigata Prefectural Tokamachi Hospital, Niigata Prefectural Tsubame Rosai Hospital, Niigata Prefectural Yoshida Hospital, Niigata Rehabilitation Hospital, Niigata Rinko Hospital, Niigata Rosai Hospital, Niitsu Medical Center Hospital, Nishikan Medical Center Hospital, Nishiniigata Chuo Hospital, Nishiniigata Orthopedics, Ojiya General Hospital, Ono Orthopedic Clinic, Okawa Clinic, Oya Orthopedic Clinic, Sado General Hospital, Saiseikai Niigata Hospital, Sanjo General Hospital, Tachikawa general Hospital, Tominaga Kusano Hospital, Toyosaka Hospital, Takahashi Orthopedic Clinic, Takahashi Orthopedic Clinic, Takahashi Orthopedics, Takahashi Orthopedics, Uonuma City Koide Hospital, Uonuma Kikan Hospital, Wakatsuki Orthopedic Clinic, and Yukiyoshi Clinic for their help with the collection of data. We also would like to express our gratitude to Ms. Takai for her devoted assistance.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The material preparation, data collection, and analysis were performed by YS, NI, and AN. The first draft of the manuscript was written by AN, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Nozaki, A., Imai, N., Shobugawa, Y. et al. Increased incidence among the very elderly in the 2020 Niigata Prefecture Osteoporotic Hip Fracture Study. J Bone Miner Metab 41, 533–541 (2023). https://doi.org/10.1007/s00774-023-01421-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-023-01421-2