Abstract
The relationship between bone tissue and bone marrow, which is responsible for hematopoiesis, is inseparable. Osteoblasts and osteocytes, which produce and consist of bone tissue, regulate the function of hematopoietic stem cells (HSC), the ancestors of all hematopoietic cells in the bone marrow. The peripheral nervous system finely regulates bone remodeling in bone tissue and modulates HSC function within the bone marrow, either directly or indirectly via modification of the HSC niche function. Peripheral nerve signals also play an important role in the development and progression of malignant tumors (including hematopoietic tumors) and normal tissues, and peripheral nerve control is emerging as a potential new therapeutic target. In this review, we summarize recent findings on the linkage among blood system, bone tissue, and peripheral nerves.



Similar content being viewed by others
References
Calvo W (1968) The innervation of the bone marrow in laboratory animals. Am J Anat 123:315–328. https://doi.org/10.1002/aja.1001230206
Pinho S, Frenette PS (2019) Haematopoietic stem cell activity and interactions with the niche. Nat Rev Mol Cell Biol 20:303–320. https://doi.org/10.1038/s41580-019-0103-9
Torres LS, Asada N, Weiss MJ, Trumpp A, Suda T, Scadden DT, Ito K (2022) Recent advances in “sickle and niche” research - Tribute to Dr. Paul S Frenette Stem Cell Reports 17:1509–1535. https://doi.org/10.1016/j.stemcr.2022.06.004
Nilsson SK, Johnston HM, Coverdale JA (2001) Spatial localization of transplanted hemopoietic stem cells: inferences for the localization of stem cell niches. Blood 97:2293–2299. https://doi.org/10.1182/blood.v97.8.2293
Calvi LM, Adams GB, Weibrecht KW, Weber JM, Olson DP, Knight MC, Martin RP, Schipani E, Divieti P, Bringhurst FR, Milner LA, Kronenberg HM, Scadden DT (2003) Osteoblastic cells regulate the haematopoietic stem cell niche. Nature 425:841–846. https://doi.org/10.1038/nature02040
Zhang J, Niu C, Ye L, Huang H, He X, Tong WG, Ross J, Haug J, Johnson T, Feng JQ, Harris S, Wiedemann LM, Mishina Y, Li L (2003) Identification of the haematopoietic stem cell niche and control of the niche size. Nature 425:836–841. https://doi.org/10.1038/nature02041
Lymperi S, Horwood N, Marley S, Gordon MY, Cope AP, Dazzi F (2008) Strontium can increase some osteoblasts without increasing hematopoietic stem cells. Blood 111:1173–1181. https://doi.org/10.1182/blood-2007-03-082800
Ma YD, Park C, Zhao H, Oduro KA Jr, Tu X, Long F, Allen PM, Teitelbaum SL, Choi K (2009) Defects in osteoblast function but no changes in long-term repopulating potential of hematopoietic stem cells in a mouse chronic inflammatory arthritis model. Blood 114:4402–4410. https://doi.org/10.1182/blood-2008-12-196311
Greenbaum A, Hsu YM, Day RB, Schuettpelz LG, Christopher MJ, Borgerding JN, Nagasawa T, Link DC (2013) CXCL12 in early mesenchymal progenitors is required for haematopoietic stem-cell maintenance. Nature 495:227–230. https://doi.org/10.1038/nature11926
Ding L, Saunders TL, Enikolopov G, Morrison SJ (2012) Endothelial and perivascular cells maintain haematopoietic stem cells. Nature 481:457–462. https://doi.org/10.1038/nature10783
Cao H, Cao B, Heazlewood CK, Domingues M, Sun X, Debele E, McGregor NE, Sims NA, Heazlewood SY, Nilsson SK (2019) Osteopontin is an important regulative component of the fetal bone marrow hematopoietic stem cell niche. Cells. https://doi.org/10.3390/cells8090985
Nilsson SK, Johnston HM, Whitty GA, Williams B, Webb RJ, Denhardt DT, Bertoncello I, Bendall LJ, Simmons PJ, Haylock DN (2005) Osteopontin, a key component of the hematopoietic stem cell niche and regulator of primitive hematopoietic progenitor cells. Blood 106:1232–1239. https://doi.org/10.1182/blood-2004-11-4422
Ding L, Morrison SJ (2013) Haematopoietic stem cells and early lymphoid progenitors occupy distinct bone marrow niches. Nature 495:231–235. https://doi.org/10.1038/nature11885
Yu VW, Saez B, Cook C, Lotinun S, Pardo-Saganta A, Wang YH, Lymperi S, Ferraro F, Raaijmakers MH, Wu JY, Zhou L, Rajagopal J, Kronenberg HM, Baron R, Scadden DT (2015) Specific bone cells produce DLL4 to generate thymus-seeding progenitors from bone marrow. J Exp Med 212:759–774. https://doi.org/10.1084/jem.20141843
Mizoguchi T, Pinho S, Ahmed J, Kunisaki Y, Hanoun M, Mendelson A, Ono N, Kronenberg HM, Frenette PS (2014) Osterix marks distinct waves of primitive and definitive stromal progenitors during bone marrow development. Dev Cell 29:340–349. https://doi.org/10.1016/j.devcel.2014.03.013
Yu VW, Lymperi S, Oki T, Jones A, Swiatek P, Vasic R, Ferraro F, Scadden DT (2016) Distinctive Mesenchymal-Parenchymal Cell Pairings Govern B Cell Differentiation in the Bone Marrow. Stem Cell Reports 7:220–235. https://doi.org/10.1016/j.stemcr.2016.06.009
Rankin EB, Wu C, Khatri R, Wilson TL, Andersen R, Araldi E, Rankin AL, Yuan J, Kuo CJ, Schipani E, Giaccia AJ (2012) The HIF signaling pathway in osteoblasts directly modulates erythropoiesis through the production of EPO. Cell 149:63–74. https://doi.org/10.1016/j.cell.2012.01.051
Bonewald LF, Johnson ML (2008) Osteocytes, mechanosensing and Wnt signaling. Bone 42:606–615. https://doi.org/10.1016/j.bone.2007.12.224
Sato M, Asada N, Kawano Y, Wakahashi K, Minagawa K, Kawano H, Sada A, Ikeda K, Matsui T, Katayama Y (2013) Osteocytes regulate primary lymphoid organs and fat metabolism. Cell Metab 18:749–758. https://doi.org/10.1016/j.cmet.2013.09.014
Bonnet D, Dick JE (1997) Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nat Med 3:730–737. https://doi.org/10.1038/nm0797-730
Lapidot T, Sirard C, Vormoor J, Murdoch B, Hoang T, Caceres-Cortes J, Minden M, Paterson B, Caligiuri MA, Dick JE (1994) A cell initiating human acute myeloid leukaemia after transplantation into SCID mice. Nature 367:645–648. https://doi.org/10.1038/367645a0
Ishikawa F, Yoshida S, Saito Y, Hijikata A, Kitamura H et al (2007) Chemotherapy-resistant human AML stem cells home to and engraft within the bone-marrow endosteal region. Nat Biotechnol 25:1315–1321. https://doi.org/10.1038/nbt1350
Kode A, Manavalan JS, Mosialou I, Bhagat G, Rathinam CV, Luo N, Khiabanian H, Lee A, Murty VV, Friedman R, Brum A, Park D, Galili N, Mukherjee S, Teruya-Feldstein J, Raza A, Rabadan R, Berman E, Kousteni S (2014) Leukaemogenesis induced by an activating beta-catenin mutation in osteoblasts. Nature 506:240–244. https://doi.org/10.1038/nature12883
Bowers M, Zhang B, Ho Y, Agarwal P, Chen CC, Bhatia R (2015) Osteoblast ablation reduces normal long-term hematopoietic stem cell self-renewal but accelerates leukemia development. Blood 125:2678–2688. https://doi.org/10.1182/blood-2014-06-582924
Mach DB, Rogers SD, Sabino MC, Luger NM, Schwei MJ, Pomonis JD, Keyser CP, Clohisy DR, Adams DJ, O’Leary P, Mantyh PW (2002) Origins of skeletal pain: sensory and sympathetic innervation of the mouse femur. Neuroscience 113:155–166. https://doi.org/10.1016/s0306-4522(02)00165-3
Abeynayake N, Arthur A, Gronthos S (2021) Crosstalk between skeletal and neural tissues is critical for skeletal health. Bone 142:115645
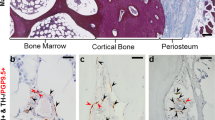
Fujita S, Morikawa T, Tamaki S, Sezaki M, Takizawa H, Okamoto S, Kataoka K, Takubo K (2022) Quantitative analysis of sympathetic and nociceptive innervation across bone marrow regions in mice. Exp Hematol. https://doi.org/10.1016/j.exphem.2022.07.297
Lorenz MR, Brazill JM, Beeve AT, Shen I, Scheller EL (2021) A neuroskeletal atlas: spatial mapping and contextualization of axon subtypes innervating the long bones of C3H and B6 mice. J Bone Miner Res 36:1012–1025. https://doi.org/10.1002/jbmr.4273
Castaneda-Corral G, Jimenez-Andrade JM, Bloom AP, Taylor RN, Mantyh WG, Kaczmarska MJ, Ghilardi JR, Mantyh PW (2011) The majority of myelinated and unmyelinated sensory nerve fibers that innervate bone express the tropomyosin receptor kinase A. Neuroscience 178:196–207. https://doi.org/10.1016/j.neuroscience.2011.01.039
Grills BL, Schuijers JA, Ward AR (1997) Topical application of nerve growth factor improves fracture healing in rats. J Orthop Res 15:235–242. https://doi.org/10.1002/jor.1100150212
Wang L, Zhou S, Liu B, Lei D, Zhao Y, Lu C, Tan A (2006) Locally applied nerve growth factor enhances bone consolidation in a rabbit model of mandibular distraction osteogenesis. J Orthop Res 24:2238–2245. https://doi.org/10.1002/jor.20269
Schinke T, Liese S, Priemel M, Haberland M, Schilling AF, Catala-Lehnen P, Blicharski D, Rueger JM, Gagel RF, Emeson RB, Amling M (2004) Decreased bone formation and osteopenia in mice lacking alpha-calcitonin gene-related peptide. J Bone Miner Res 19:2049–2056. https://doi.org/10.1359/JBMR.040915
Mrak E, Guidobono F, Moro G, Fraschini G, Rubinacci A, Villa I (2010) Calcitonin gene-related peptide (CGRP) inhibits apoptosis in human osteoblasts by beta-catenin stabilization. J Cell Physiol 225:701–708. https://doi.org/10.1002/jcp.22266
Wang L, Shi X, Zhao R, Halloran BP, Clark DJ, Jacobs CR, Kingery WS (2010) Calcitonin-gene-related peptide stimulates stromal cell osteogenic differentiation and inhibits RANKL induced NF-kappaB activation, osteoclastogenesis and bone resorption. Bone 46:1369–1379. https://doi.org/10.1016/j.bone.2009.11.029
Mori T, Ogata T, Okumura H, Shibata T, Nakamura Y, Kataoka K (1999) Substance P regulates the function of rabbit cultured osteoclast; increase of intracellular free calcium concentration and enhancement of bone resorption. Biochem Biophys Res Commun 262:418–422. https://doi.org/10.1006/bbrc.1999.1220
Wang L, Zhao R, Shi X, Wei T, Halloran BP, Clark DJ, Jacobs CR, Kingery WS (2009) Substance P stimulates bone marrow stromal cell osteogenic activity, osteoclast differentiation, and resorption activity in vitro. Bone 45:309–320. https://doi.org/10.1016/j.bone.2009.04.203
Niedermair T, Schirner S, Seebroker R, Straub RH, Grassel S (2018) Substance modulates bone remodeling properties of murine osteoblasts and osteoclasts. Sci Rep 8:9199. https://doi.org/10.1038/s41598-018-27432-y
Luo Y, Raible D, Raper JA (1993) Collapsin: a protein in brain that induces the collapse and paralysis of neuronal growth cones. Cell 75:217–227. https://doi.org/10.1016/0092-8674(93)80064-l
Behar O, Golden JA, Mashimo H, Schoen FJ, Fishman MC (1996) Semaphorin III is needed for normal patterning and growth of nerves, bones and heart. Nature 383:525–528. https://doi.org/10.1038/383525a0
Hayashi M, Nakashima T, Taniguchi M, Kodama T, Kumanogoh A, Takayanagi H (2012) Osteoprotection by semaphorin 3A. Nature 485:69–74. https://doi.org/10.1038/nature11000
Hayashi M, Nakashima T, Yoshimura N, Okamoto K, Tanaka S, Takayanagi H (2019) Autoregulation of osteocyte sema3a orchestrates estrogen action and counteracts bone aging. Cell Metab 29:627–637
Fukuda T, Takeda S, Xu R, Ochi H, Sunamura S et al (2013) Sema3A regulates bone-mass accrual through sensory innervations. Nature 497:490–493. https://doi.org/10.1038/nature12115
Bajayo A, Bar A, Denes A, Bachar M, Kram V, Attar-Namdar M, Zallone A, Kovacs KJ, Yirmiya R, Bab I (2012) Skeletal parasympathetic innervation communicates central IL-1 signals regulating bone mass accrual. Proc Natl Acad Sci U S A 109:15455–15460. https://doi.org/10.1073/pnas.1206061109
Chartier SR, Mitchell SAT, Majuta LA, Mantyh PW (2018) The changing sensory and sympathetic innervation of the young, adult and aging mouse femur. Neuroscience 387:178–190. https://doi.org/10.1016/j.neuroscience.2018.01.047
Takeda S, Elefteriou F, Levasseur R, Liu X, Zhao L, Parker KL, Armstrong D, Ducy P, Karsenty G (2002) Leptin regulates bone formation via the sympathetic nervous system. Cell 111:305–317. https://doi.org/10.1016/s0092-8674(02)01049-8
Elefteriou F, Ahn JD, Takeda S, Starbuck M, Yang X, Liu X, Kondo H, Richards WG, Bannon TW, Noda M, Clement K, Vaisse C, Karsenty G (2005) Leptin regulation of bone resorption by the sympathetic nervous system and CART. Nature 434:514–520. https://doi.org/10.1038/nature03398
Kajimura D, Hinoi E, Ferron M, Kode A, Riley KJ, Zhou B, Guo XE, Karsenty G (2011) Genetic determination of the cellular basis of the sympathetic regulation of bone mass accrual. J Exp Med 208:841–851. https://doi.org/10.1084/jem.20102608
Sato T, Abe T, Chida D, Nakamoto N, Hori N, Kokabu S, Sakata Y, Tomaru Y, Iwata T, Usui M, Aiko K, Yoda T (2010) Functional role of acetylcholine and the expression of cholinergic receptors and components in osteoblasts. FEBS Lett 584:817–824. https://doi.org/10.1016/j.febslet.2010.01.001
Sato T, Abe T, Nakamoto N, Tomaru Y, Koshikiya N, Nojima J, Kokabu S, Sakata Y, Kobayashi A, Yoda T (2008) Nicotine induces cell proliferation in association with cyclin D1 up-regulation and inhibits cell differentiation in association with p53 regulation in a murine pre-osteoblastic cell line. Biochem Biophys Res Commun 377:126–130. https://doi.org/10.1016/j.bbrc.2008.09.114
Mandl P, Hayer S, Karonitsch T, Scholze P, Gyori D, Sykoutri D, Bluml S, Mocsai A, Poor G, Huck S, Smolen JS, Redlich K (2016) Nicotinic acetylcholine receptors modulate osteoclastogenesis. Arthritis Res Ther 18:63. https://doi.org/10.1186/s13075-016-0961-x
Mito K, Sato Y, Kobayashi T, Miyamoto K, Nitta E, Iwama A, Matsumoto M, Nakamura M, Sato K, Miyamoto T (2017) The nicotinic acetylcholine receptor alpha7 subunit is an essential negative regulator of bone mass. Sci Rep 7:45597. https://doi.org/10.1038/srep45597
Somm E, Guerardel A, Maouche K, Toulotte A, Veyrat-Durebex C, Rohner-Jeanrenaud F, Maskos U, Huppi PS, Schwitzgebel VM (2014) Concomitant alpha7 and beta2 nicotinic AChR subunit deficiency leads to impaired energy homeostasis and increased physical activity in mice. Mol Genet Metab 112:64–72. https://doi.org/10.1016/j.ymgme.2014.03.003
Shi Y, Oury F, Yadav VK, Wess J, Liu XS, Guo XE, Murshed M, Karsenty G (2010) Signaling through the M(3) muscarinic receptor favors bone mass accrual by decreasing sympathetic activity. Cell Metab 11:231–238. https://doi.org/10.1016/j.cmet.2010.01.005
Pareyson D, Marchesi C (2009) Diagnosis, natural history, and management of Charcot-Marie-Tooth disease. Lancet Neurol 8:654–667. https://doi.org/10.1016/S1474-4422(09)70110-3
Pouwels S, de Boer A, Leufkens HG, Weber WE, Cooper C, de Vries F (2014) Risk of fracture in patients with charcot-marie-tooth disease. Muscle Nerve 50:919–924. https://doi.org/10.1002/mus.24240
Abdala R, Levi L, Longobardi V, Zanchetta MB (2020) Severe bone microarchitecture deterioration in a family with hereditary neuropathy: evidence of the key role of the mechanostat. Osteoporos Int 31:2477–2480. https://doi.org/10.1007/s00198-020-05674-9
Schwartzlow C, Kazamel M (2019) Hereditary sensory and autonomic neuropathies: adding more to the classification. Curr Neurol Neurosci Rep 19:52. https://doi.org/10.1007/s11910-019-0974-3
Maayan C, Bar-On E, Foldes AJ, Gesundheit B, Pollak RD (2002) Bone mineral density and metabolism in familial dysautonomia. Osteoporos Int 13:429–433. https://doi.org/10.1007/s001980200050
Maayan C, Becker Y, Gesundheit B, Girgis SI (2001) Calcitonin gene related peptide in familial dysautonomia. Neuropeptides 35:189–195. https://doi.org/10.1054/npep.2001.0863
Katayama Y, Battista M, Kao WM, Hidalgo A, Peired AJ, Thomas SA, Frenette PS (2006) Signals from the sympathetic nervous system regulate hematopoietic stem cell egress from bone marrow. Cell 124:407–421. https://doi.org/10.1016/j.cell.2005.10.041
Kawamori Y, Katayama Y, Asada N, Minagawa K, Sato M, Okamura A, Shimoyama M, Nakagawa K, Okano T, Tanimoto M, Kato S, Matsui T (2010) Role for vitamin D receptor in the neuronal control of the hematopoietic stem cell niche. Blood 116:5528–5535. https://doi.org/10.1182/blood-2010-04-279216
Asada N, Katayama Y, Sato M, Minagawa K, Wakahashi K, Kawano H, Kawano Y, Sada A, Ikeda K, Matsui T, Tanimoto M (2013) Matrix-embedded osteocytes regulate mobilization of hematopoietic stem/progenitor cells. Cell Stem Cell 12:737–747. https://doi.org/10.1016/j.stem.2013.05.001
Lucas D, Bruns I, Battista M, Mendez-Ferrer S, Magnon C, Kunisaki Y, Frenette PS (2012) Norepinephrine reuptake inhibition promotes mobilization in mice: potential impact to rescue low stem cell yields. Blood 119:3962–3965. https://doi.org/10.1182/blood-2011-07-367102
Kawano Y, Fukui C, Shinohara M, Wakahashi K, Ishii S, Suzuki T, Sato M, Asada N, Kawano H, Minagawa K, Sada A, Furuyashiki T, Uematsu S, Akira S, Uede T, Narumiya S, Matsui T, Katayama Y (2017) G-CSF-induced sympathetic tone provokes fever and primes antimobilizing functions of neutrophils via PGE2. Blood 129:587–597. https://doi.org/10.1182/blood-2016-07-725754
Yamazaki S, Ema H, Karlsson G, Yamaguchi T, Miyoshi H, Shioda S, Taketo MM, Karlsson S, Iwama A, Nakauchi H (2011) Nonmyelinating Schwann cells maintain hematopoietic stem cell hibernation in the bone marrow niche. Cell 147:1146–1158. https://doi.org/10.1016/j.cell.2011.09.053
Liu Y, Chen Q, Jeong HW, Han D, Fabian J, Drexler HCA, Stehling M, Scholer HR, Adams RH (2021) Dopamine signaling regulates hematopoietic stem and progenitor cell function. Blood 138:2051–2065. https://doi.org/10.1182/blood.2020010419
Mendez-Ferrer S, Lucas D, Battista M, Frenette PS (2008) Haematopoietic stem cell release is regulated by circadian oscillations. Nature 452:442–447. https://doi.org/10.1038/nature06685
Mendez-Ferrer S, Michurina TV, Ferraro F, Mazloom AR, Macarthur BD, Lira SA, Scadden DT, Ma’ayan A, Enikolopov GN, Frenette PS (2010) Mesenchymal and haematopoietic stem cells form a unique bone marrow niche. Nature 466:829–834. https://doi.org/10.1038/nature09262
Lucas D, Scheiermann C, Chow A, Kunisaki Y, Bruns I, Barrick C, Tessarollo L, Frenette PS (2013) Chemotherapy-induced bone marrow nerve injury impairs hematopoietic regeneration. Nat Med 19:695–703. https://doi.org/10.1038/nm.3155
Geiger H, de Haan G, Florian MC (2013) The ageing haematopoietic stem cell compartment. Nat Rev Immunol 13:376–389. https://doi.org/10.1038/nri3433
Maryanovich M, Zahalka AH, Pierce H, Pinho S, Nakahara F, Asada N, Wei Q, Wang X, Ciero P, Xu J, Leftin A, Frenette PS (2018) Adrenergic nerve degeneration in bone marrow drives aging of the hematopoietic stem cell niche. Nat Med 24:782–791. https://doi.org/10.1038/s41591-018-0030-x
Ho YH, Del Toro R, Rivera-Torres J, Rak J, Korn C et al (2019) Remodeling of bone marrow hematopoietic stem cell niches promotes myeloid cell expansion during premature or physiological aging. Cell Stem Cell 25:407–418
Li H, Qu J, Zhu H, Wang J, He H, Xie X, Wu R, Lu Q (2021) CGRP regulates the age-related switch between osteoblast and adipocyte differentiation. Front Cell Dev Biol. 9:675503
Pierce H, Zhang D, Magnon C, Lucas D, Christin JR, Huggins M, Schwartz GJ, Frenette PS (2017) Cholinergic signals from the CNS regulate G-CSF-mediated hsc mobilization from bone marrow via a glucocorticoid signaling relay. Cell Stem Cell 20:648–658
Garcia-Garcia A, Korn C, Garcia-Fernandez M, Domingues O, Villadiego J, Martin-Perez D, Isern J, Bejarano-Garcia JA, Zimmer J, Perez-Simon JA, Toledo-Aral JJ, Michel T, Airaksinen MS, Mendez-Ferrer S (2019) Dual cholinergic signals regulate daily migration of hematopoietic stem cells and leukocytes. Blood 133:224–236. https://doi.org/10.1182/blood-2018-08-867648
Fielding C, Garcia-Garcia A, Korn C, Gadomski S, Fang Z, Reguera JL, Perez-Simon JA, Gottgens B, Mendez-Ferrer S (2022) Cholinergic signals preserve haematopoietic stem cell quiescence during regenerative haematopoiesis. Nat Commun 13:543. https://doi.org/10.1038/s41467-022-28175-1
Hill EL, Elde R (1991) Distribution of CGRP, VIP, D beta H, SP, and NPY-immunoreactive nerves in the periosteum of the rat. Cell Tissue Res 264:469–480. https://doi.org/10.1007/BF00319037
Gao X, Zhang D, Xu C, Li H, Caron KM, Frenette PS (2021) Nociceptive nerves regulate haematopoietic stem cell mobilization. Nature 589:591–596. https://doi.org/10.1038/s41586-020-03057-y
Zahalka AH, Arnal-Estape A, Maryanovich M, Nakahara F, Cruz CD, Finley LWS, Frenette PS (2017) Adrenergic nerves activate an angio-metabolic switch in prostate cancer. Science 358:321–326. https://doi.org/10.1126/science.aah5072
Hanoun M, Zhang D, Mizoguchi T, Pinho S, Pierce H, Kunisaki Y, Lacombe J, Armstrong SA, Duhrsen U, Frenette PS (2014) Acute myelogenous leukemia-induced sympathetic neuropathy promotes malignancy in an altered hematopoietic stem cell niche. Cell Stem Cell 15:365–375. https://doi.org/10.1016/j.stem.2014.06.020
Arranz L, Sanchez-Aguilera A, Martin-Perez D, Isern J, Langa X, Tzankov A, Lundberg P, Muntion S, Tzeng YS, Lai DM, Schwaller J, Skoda RC, Mendez-Ferrer S (2014) Neuropathy of haematopoietic stem cell niche is essential for myeloproliferative neoplasms. Nature 512:78–81. https://doi.org/10.1038/nature13383
Baryawno N, Przybylski D, Kowalczyk MS, Kfoury Y, Severe N, Gustafsson K, Kokkaliaris KD, Mercier F, Tabaka M, Hofree M, Dionne D, Papazian A, Lee D, Ashenberg O, Subramanian A, Vaishnav ED, Rozenblatt-Rosen O, Regev A, Scadden DT (2019) A cellular taxonomy of the bone marrow stroma in homeostasis and leukemia. Cell 177:1915–1932
Tikhonova AN, Dolgalev I, Hu H, Sivaraj KK, Hoxha E et al (2019) The bone marrow microenvironment at single-cell resolution. Nature 569:222–228. https://doi.org/10.1038/s41586-019-1104-8
Baccin C, Al-Sabah J, Velten L, Helbling PM, Grunschlager F, Hernandez-Malmierca P, Nombela-Arrieta C, Steinmetz LM, Trumpp A, Haas S (2020) Combined single-cell and spatial transcriptomics reveal the molecular, cellular and spatial bone marrow niche organization. Nat Cell Biol 22:38–48. https://doi.org/10.1038/s41556-019-0439-6
Funding
This work was supported in part by AMED (Grant Number JP22gm1510001 to N.A. and Y.K.).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Asada, N., Katayama, Y. A mysterious triangle of blood, bones, and nerves. J Bone Miner Metab 41, 404–414 (2023). https://doi.org/10.1007/s00774-023-01402-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-023-01402-5