Abstract
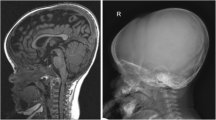
Achondroplasia (ACH) is the most common skeletal dysplasia and characterized by a disproportionate short stature, macrocephaly with frontal bossing, exaggerated lumbar lordosis, and trident hands. It is induced by activated mutations in the fibroblast growth factor receptor 3 (FGFR3) gene. In addition to short stature, patients with ACH have a high prevalence of medical complications, including upper airway obstructive apnea, increased mortality, foramen magnum stenosis, hydrocephalus, developmental delay, recurrent ear infections, genu varum, obesity, and spinal canal stenosis, throughout their whole life. Several investigational drugs that modulate abnormal FGFR3 signaling have recently emerged, vosoritide being the most developed. This review presents the different disease-specific complications of ACH occurring in neonates, infants, childhood, adolescent, and adults and reports the current multidisciplinary interventions for these various complications. Moreover, we propose treatment strategies for children with ACH from the perspective of quality of life in adulthood.




Similar content being viewed by others
References
Waller DK, Correa A, Vo TM, Wang Y, Hobbs C, Langlois PH, Pearson K, Romitti PA, Shaw GM, Hecht JT (2008) The population-based prevalence of achondroplasia and thanatophoric dysplasia in selected regions of the US. Am J Med Genet A 146A:2385–2389
Rousseau F, Bonaventure J, Legeai-Mallet L, Pelet A, Rozet JM, Maroteaux P, Le Merrer M, Munnich A (1994) Mutations in the gene encoding fibroblast growth factor receptor-3 in achondroplasia. Nature 371:252–254
Shiang R, Thompson LM, Zhu YZ, Church DM, Fielder TJ, Bocian M, Winokur ST, Wasmuth JJ (1994) Mutations in the transmembrane domain of FGFR3 cause the most common genetic form of dwarfism, achondroplasia. Cell 78:335–342
Coi A, Santoro M, Garne E, Pierini A, Addor MC, Alessandri JL, Bergman JE, Bianchi F, Boban L, Braz P, Cavero-Carbonell C (2019) Epidemiology of achondroplasia: a population-based study in Europe. Am J Med Genet A 179:1791–1798
Baujat G, Legeai-Mallet L, Finidori G, Cormier-Daire V, Le Merrer M (2008) Achondroplasia. Best Pract Res Clin Rheumatol 22:3–18
Savarirayan R, Tofts L, Irving M, Wilcox WR, Bacino CA et al (2021) Safe and persistent growth-promoting effects of vosoritide in children with achondroplasia: 2-year results from an open-label, phase 3 extension study. Genet Med. https://doi.org/10.1038/s41436-021-01287-7
Breinholt VM, Rasmussen CE, Mygind PH, Kjelgaard-Hansen M, Faltinger F, Berngard A, Zettler J, Hersel U (2019) TransCon CNP, a sustained-release C-type natriuretic peptide prodrug, a potentially safe and efficacious new therapeutic modality for the treatment of comorbidities associated with fibroblast growth factor receptor 3-related skeletal dysplasias. J Permacol Exp Ther 370:459–471
Goncalves D, Rignol G, Dellugat P, Hartmann G, Garcia SS, Stavenhagen J, Santarelli L, Gouze E, Czech C (2020) In vitro and in vivo characterization of Recifercept, a soluble fibroblast growth factor receptor 3, as treatment for achondroplasia. PLoS ONE 15:e0244368
Kimura T, Bosakova M, Nonaka Y, Hruba E, Yasuda K et al (2021) An RNA aptamer restores defective bone growth in FGFR3-related skeletal dysplasia in mice. Sci Transl Med 13:eaba4226
Kitoh H, Matsushita M, Michima K, Nagata T, Kamiya Y, Ueda K, Kuwatsuka Y, Morikawa H, Nakai Y, Ishiguro N (2020) Pharmacokinetics and safety after once and twice a day doses of meclizine hydrochloride administered to children with achondroplasia. PLoS ONE 15:20229639
Komla-Ebri D, Dambroise E, Kramer I, Benoist-Lasselin C, Kaci N, Le Gall C, Martin L, Busca P, Barbault F, Graus-Porta D, Munnich A, Kneissel M, Di Rocco F, Biosse-Duplan M, Legeai-Mallet L (2016) Tyrosine kinase inhibitor NVP-BGJ398 functionally improves FGFR3-related dwarfism in mouse model. J Clin Invest 126:1871–1884
Zucconi M, Weber G, Castronovo V, Ferini-Strambi L, Russo F, Chiumello G, Smirne S (1996) Sleep and upper airway obstruction in children with achondroplasia. J Pediatr 129:743–749
Trotter TL, Hall JG, American Academy of Pediatrics Committee on Genetics (2005) Health supervision for children with achondroplasia. Pediatrics 116:771–783
Tenconi R, Khirani S, Amaddeo A, Michot C, Baujat G, Couloigner V, De Sanctis L, James S, Zerah M, Cormier-Daire V, Fauroux B (2017) Sleep-disordered breathing and its management in children with achondroplasia. Am J Med Genet A 173:868–878
Hecht JT, Horton WA, Reid CS, Pyeritz RE, Chakraborty R (1989) Growth of the foramen magnum in achondroplasia. Am J Med Genet 32:528–535
Ednick M, Tinkle BT, Phromchairak J, Egelhoff J, Amin R, Simakajornboon N (2009) Sleep-related respiratory abnormalities and arousal pattern in achondroplasia during early infancy. J Pediatr 155:510–515
White KK, Bompadre V, Goldberg MJ, Bober MB, Campbell JW, Cho TJ, Hoover-Fong J, Mackenzie W, Parnell SE, Raggio C, Rapoport DM, Spencer SA, Savarirayan R (2016) Best practices in the evaluation and treatment of foramen magnum stenosis in achondroplasia during infancy. Am J Med Genet A 170A:42–51
Bagley CA, Pindrik JA, Bookland MJ, Camara-Quintana JQ, Carson BS (2006) Cervicomedullary decompression for foramen magnum stenosis in achondroplasia. J Neurosurg 104:166–172
King JA, Vachhrajani S, Drake JM, Rutka JT (2009) Neurosurgical implications of achondroplasia. J Neurosurg Pediatr 4:297–306
Todorov AB, Scott CI Jr, Warren AE, Leeper JD (1981) Developmental screening tests in achondroplastic children. Am J Med Genet 9:19–23
Ireland PJ, Donaghey S, McGill J, Zankl A, Ware RS, Pacey V, Ault J, Savarirayan R, Sillence D, Thompson E, Townshend S, Johnston LM (2012) Development in children with achondroplasia: a prospective clinical cohort study. Dev Med Child Neurol 54:532–537
Kopits SE (1988) Thoracolumbar kyphosis and lumbosacral hyperlordosis in achondroplastic children. Basic Life Sci 48:241–255
Pauli RM, Breed A, Horton VK, Glinski LP, Reiser CA (1997) Prevention of fixed, angular kyphosis in achondroplasia. J Pediatr Orthop 17:726–733
Margalit A, McKean G, Lawing C, Galey S, Ain MC (2018) Walking out of the curve: thoracolumbar kyphosis in achondroplasia. J Pediatr Orthop 38:491–497
Horton WA, Rotter JI, Rimoin DL, Scott CI, Hall JG (1978) Standard growth curves for achondroplasia. J Pediatr 93:435–438
Harada D, Namba N, Hanioka Y, Ueyama K, Sakamoto N, Nakano Y, Izui M, Nagamatsu Y, Kashiwagi H, Yamamuro M, Ishiura Y, Ogitani A, Seino Y (2017) Final adult height in long-term growth hormone-treated achondroplasia patients. Eur J Pediatr 176:873–879
Kitoh H, Mishima K, Matsushita M, Nishida Y, Ishiguro N (2014) Early and late fracture following extensive limb lengthening in patients with achondroplasia and hypochondroplasia. Bone Joint J 96-B:1269–1273
Collins WO, Choi SS (2007) Otolaryngologic manifestations of achondroplasia. Arch Otolaryngol Head Neck Surg 133:237–244
Hunter AG, Bankier A, Rogers JG, Sillence D, Scott CI (1998) Medical complications of achondroplasia: a multicentre patient review. J Med Genet 35:705–712
Inan M, Thacker M, Church C, Miller F, Mackenzie WG, Conklin D (2006) Dynamic lower extremity alignment in children with achondroplasia. J Pediatr Orthop 26:526–529
McClure PK, Kilinc E, Birch JG (2017) Growth modulation in achondroplasia. J Pediatr Orthop 37:e384–e387
Okura T, Matsushita M, Mishima K, Esaki R, Seki T, Ishiguro N, Kitoh H (2018) Activated FGFR3 prevents subchondral bone sclerosis during the development of osteoarthritis in transgenic mice with achondroplasia. J Orthop Res 36:300–308
Hoover-Fong J, McGready J, Schulze K, Alade AY, Scott CI (2017) A height-for-age growth reference for children with achondroplasia: expanded applications and comparison with original reference data. Am J Med Genet A 173:1226–1230
Merker A, Neumeyer L, Hertel NT, Grigelioniene G, Mäkitie O, Mohnike K, Hagenäs L (2018) Growth in achondroplasia: development of height, weight, head circumference, and body mass index in a European cohort. Am J Med Genet A 176:1723–1734
Tofts L, Das S, Collins F, Burton KLO (2017) Growth charts for Australian children with achondroplasia. Am J Med Genet A 173:2189–2200
Tachibana K, Suwa S, Nishiyama S, Matsuda I (1997) Analysis of height of children with achondroplasia based on a national survey. Shounikarinsyou 8:1363–1369 (in Japanese)
Del Pino M, Ramos Mejía R, Fano V (2018) Leg length, sitting height, and body proportions references for achondroplasia: new tools for monitoring growth. Am J Med Genet A 176:896–906
Merker A, Neumeyer L, Hertel NT, Grigelioniene G, Mohnike K, Hagenäs L (2018) Development of body proportions in achondroplasia: sitting height, leg length, arm span, and foot length. Am J Med Genet A 176:1819–1829
Hunter AGW, Hecht JT, Scott CI (1996) Standard weight for height curves in achondroplasia. Am J Med Genet 62:255–261
Hoover-Fong JE, McGready J, Schulze KJ, Barnes H, Scott CI (2007) Weight for age chars for children with achondroplasia. Am J Med Genet A 143A:2227–2235
Wynn J, King TM, Gambello MJ, Waller DK, Hecht JT (2007) Mortality in achondroplasia study: a 42-year follow-up. Am J Med Genet A 143A:2502–2511
Kitoh H, Kitakoji T, Kurita K, Katoh M, Takamine Y (2002) Deformities of the elbow in achondroplasia. J Bone Joint Surg Br 84:680–683
Mahomed NN, Spellmann M, Goldberg MJ (1998) Functional health status of adults with achondroplasia. Am J Med Genet 78:30–35
Ain MC, Abdullah MA, Ting BL, Skolasky RL, Carlisle ES, Schkrohowsky JG, Rigamonti D (2010) Progression of low back and lower extremity pain in a cohort of patients with achondroplasia. J Neurosurg Spine 13:335–340
Vleggeert-Lankamp C, Peul W (2012) Surgical decompression of thoracic spinal stenosis in achondroplasia: indication and outcome. J Neurosurg Spine 17:164–172
Suzuki K, Kanamori M, Nobukiyo M (2008) Ossification of the thoracic ligamentum flavum in an achondroplastic patient: a case report. J Orthop Surg (Hong Kong) 16:392–395
Cabrera-Aldana EE, De la Garza RR, Zuluaga Gómez A, Rosales-Olivares LM, Reyes-Sánchez A (2016) Multiple thoracic ossification of the ligamentum flavum in a Hispanic woman with achondroplasia. Spine J 16:e749–e750
Gokcen HB, Ozturk C (2019) Ossification of the ligamentum flavum at the thoracic and lumbar region in an achondroplastic patient. World Neurosurg 126:461–465
Kachonkittisak K, Kunakornsawat S, Pluemvitayaporn T, Piyaskulkaew C, Pruttikul P, Kittithamvongs P (2019) Congenital spinal canal stenosis with ossification of the ligamentum flavum in an achondroplastic patient: a case report and literature review. Asian J Neurosurg 14:1231–1235
Matsushita M, Kitoh H, Mishima K, Yamashita S, Haga N, Fujiwara S, Ozono K, Kubota T, Kitaoka T, Ishiguro N (2019) Physical, mental, and social problems of adolescent and adult patients with achondroplasia. Calcif Tissue Int 104:364–372
Dhiman N, Albaghdadi A, Zogg CK, Sharma M, Hoover-Fong JE, Ain MC, Haider AH (2017) Factors associated with health-related quality of life (HRQOL) in adults with short stature skeletal dysplasias. Qual Life Res 26:1337–1348
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
This work was supported by the Health Labor Sciences Research Grants, the Ministry of Health, Labor and Welfare, Japan (Grant number, 19FC1006).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Kitoh, H., Matsushita, M., Mishima, K. et al. Disease-specific complications and multidisciplinary interventions in achondroplasia. J Bone Miner Metab 40, 189–195 (2022). https://doi.org/10.1007/s00774-021-01298-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-021-01298-z