Abstract
Introduction
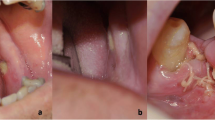
Antiresorptive-related osteonecrosis of the jaw (ARONJ) is a rare but serious adverse event associated with bone-modifying agents (BMAs) and affects patients in the terminal stages of cancer. Molecular targeting drugs (MTDs), anti-vascular endothelial growth factor receptor (VEGFR), and anti-epidermal growth factor receptor (EGFR) drugs are essential in various cancer treatments, although MTDs are risk factors for ARONJ. However, the mechanism through which MTDs affect treatment prognosis of ARONJ remains unclear. Therefore, we investigated the potential inhibitory factors for healing in the conservative therapy of ARONJ with a focus on MTDs.
Materials and methods
Sixty patients who were administered BMAs for the treatment of malignancies and who underwent conservative treatment for ARONJ were assessed. The healing rate of ARONJ for each risk factor was retrospectively evaluated.
Results
Among the 60 patients, 27 were male and 33 were female. The median age was 67 years, and the median follow-up period was 292 (range 91–1758) days. The healing rate was lower in those treated with both zoledronic acid (Za) and denosumab (Dmab) than in those treated with Za or Dmab alone (0% vs. 28.8%, p = 0.03). Regarding the administration of MTDs, the treatment rate with anti-VEGFR drugs was 7.1% (p = 0.04), anti-EGFR drugs was 12.5% (p = 0.18), and without MTDs was 36.8%.
Conclusion
In the conservative treatment of ARONJ, the administration of several BMAs and anti-VEGFR drugs was the factor contributing to the inhibition of healing.
Similar content being viewed by others
References
Gnant M, Pfeiler G, Dubsky PC, Hubalek M, Greil R et al (2015) Adjuvant denosumab in breast cancer (ABCSG-18): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet 386:433–443
Smith MR, Egerdie B, Hernandez Toriz N, Feldman R, Tammela TL, Saad F, Heracek J, Szwedowski M, Ke C, Kupic A, Leder BZ, Goessl C, Denosumab HPCSG (2009) Denosumab in men receiving androgen-deprivation therapy for prostate cancer. N Engl J Med 361:745–755
Marx RE, Cillo JE Jr, Ulloa JJ (2007) Oral bisphosphonate-induced osteonecrosis: risk factors, prediction of risk using serum CTX testing, prevention, and treatment. J Oral Maxillofac Surg 65:2397–2410
Yarom N, Shapiro CL, Peterson DE, Van Poznak CH, Bohlke K, Ruggiero SL, Migliorati CA, Khan A, Morrison A, Anderson H, Murphy BA, Alston-Johnson D, Mendes RA, Beadle BM, Jensen SB, Saunders DP (2019) Medication-related osteonecrosis of the jaw: MASCC/ISOO/ASCO clinical practice guideline. J Clin Oncol 37:2270–2290
Saad F, Brown JE, Van Poznak C, Ibrahim T, Stemmer SM, Stopeck AT, Diel IJ, Takahashi S, Shore N, Henry DH, Barrios CH, Facon T, Senecal F, Fizazi K, Zhou L, Daniels A, Carriere P, Dansey R (2012) Incidence, risk factors, and outcomes of osteonecrosis of the jaw: integrated analysis from three blinded active-controlled phase III trials in cancer patients with bone metastases. Ann Oncol 23:1341–1347
Hayashida S, Yanamoto S, Fujita S, Hasegawa T, Komori T, Kojima Y, Miyamoto H, Shibuya Y, Ueda N, Kirita T, Nakahara H, Shinohara M, Kondo E, Kurita H, Umeda M (2020) Drug holiday clinical relevance verification for antiresorptive agents in medication-related osteonecrosis cases of the jaw. J Bone Miner Metab 38:126–134
Ikeda T, Kuraguchi J, Kogashiwa Y, Yokoi H, Satomi T, Kohno N (2015) Successful treatment of bisphosphonate-related osteonecrosis of the jaw (BRONJ) patients with sitafloxacin: new strategies for the treatment of BRONJ. Bone 73:217–222
El-Rabbany M, Lam DK, Shah PS, Azarpazhooh A (2019) Surgical management of medication-related osteonecrosis of the jaw is associated with improved disease resolution: a retrospective cohort study. J Oral Maxillofac Surg 77:1816–1822
Sitohy B, Nagy JA, Dvorak HF (2012) Anti-VEGF/VEGFR therapy for cancer: reassessing the target. Cancer Res 72:1909–1914
Vokes EE, Chu E (2006) Anti-EGFR therapies: clinical experience in colorectal, lung, and head and neck cancers. Oncology 20:15–25
Lee HW, Choi HJ, Ha SJ, Lee KT, Kwon YG (2013) Recruitment of monocytes/macrophages in different tumor microenvironments. Biochim Biophys Acta 1835:170–179
Yang ZF, Poon RT, Luo Y, Cheung CK, Ho DW, Lo CM, Fan ST (2004) Up-regulation of vascular endothelial growth factor (VEGF) in small-for-size liver grafts enhances macrophage activities through VEGF receptor 2-dependent pathway. J Immunol 173:2507–2515
Pastore S, Mascia F, Mariani V, Girolomoni G (2008) The epidermal growth factor receptor system in skin repair and inflammation. J Invest Dermatol 128:1365–1374
Repertinger SK, Campagnaro E, Fuhrman J, El-Abaseri T, Yuspa SH, Hansen LA (2004) EGFR enhances early healing after cutaneous incisional wounding. J Invest Dermatol 123:982–989
van Cann T, Loyson T, Verbiest A, Clement PM, Bechter O et al (2018) Incidence of medication-related osteonecrosis of the jaw in patients treated with both bone resorption inhibitors and vascular endothelial growth factor receptor tyrosine kinase inhibitors. Support Care Cancer 26:869–878
Beuselinck B, Wolter P, Karadimou A, Elaidi R, Dumez H, Rogiers A, Van Cann T, Willems L, Body JJ, Berkers J, Van Poppel H, Lerut E, Debruyne P, Paridaens R, Schoffski P (2012) Concomitant oral tyrosine kinase inhibitors and bisphosphonates in advanced renal cell carcinoma with bone metastases. Br J Cancer 107:1665–1671
Nifosi AF, Zuccarello M, Nifosi L, Hervas Saus V, Nifosi G (2019) Osteonecrosis of the jaw in the era of targeted therapy and immunotherapy in oncology. J Korean Assoc Oral Maxillofac Surg 45:3–8
Shibahara T (2019) Antiresorptive agent-related osteonecrosis of the jaw (ARONJ): a twist of fate in the bone. Tohoku J Exp Med 247:75–86
Japanese Allied Committee on Osteonecrosis of the Jaw, Yoneda T, Hagino H, Sugimoto T, Ohta H, Takahashi S, Soen S, Taguchi A, Nagata T, Urade M, Shibahara T, Toyosawa S (2017) Antiresorptive agent-related osteonecrosis of the jaw: Position Paper 2017 of the Japanese Allied Committee on Osteonecrosis of the Jaw. J Bone Miner Metab 35:6–19
Soundia A, Hadaya D, Esfandi N, Gkouveris I, Christensen R, Dry SM, Bezouglaia O, Pirih F, Nikitakis N, Aghaloo T, Tetradis S (2018) Zoledronate impairs socket healing after extraction of teeth with experimental periodontitis. J Dent Res 97:312–320
Scappaticci FA, Fehrenbacher L, Cartwright T, Hainsworth JD, Heim W, Berlin J, Kabbinavar F, Novotny W, Sarkar S, Hurwitz H (2005) Surgical wound healing complications in metastatic colorectal cancer patients treated with bevacizumab. J Surg Oncol 91:173–180
Allegra CJ, Yothers G, O’Connell MJ, Sharif S, Colangelo LH, Lopa SH, Petrelli NJ, Goldberg RM, Atkins JN, Seay TE, Fehrenbacher L, O’Reilly S, Chu L, Azar CA, Wolmark N (2009) Initial safety report of NSABP C-08: a randomized phase III study of modified FOLFOX6 with or without bevacizumab for the adjuvant treatment of patients with stage II or III colon cancer. J Clin Oncol 27:3385–3390
Golshan M, Garber JE, Gelman R, Tung N, Smith BL, Troyan S, Greenberg CC, Winer EP, Ryan P (2011) Does neoadjuvant bevacizumab increase surgical complications in breast surgery? Ann Surg Oncol 18:733–737
Jonasch E, Wood CG, Matin SF, Tu SM, Pagliaro LC, Corn PG, Aparicio A, Tamboli P, Millikan RE, Wang X, Araujo JC, Arap W, Tannir N (2009) Phase II presurgical feasibility study of bevacizumab in untreated patients with metastatic renal cell carcinoma. J Clin Oncol 27:4076–4081
Clark AJ, Butowski NA, Chang SM, Prados MD, Clarke J, Polley MY, Sughrue ME, McDermott MW, Parsa AT, Berger MS, Aghi MK (2011) Impact of bevacizumab chemotherapy on craniotomy wound healing. J Neurosurg 114:1609–1616
Fornaro L, Caparello C, Vivaldi C, Rotella V, Musettini G, Falcone A, Baldini E, Masi G (2014) Bevacizumab in the pre-operative treatment of locally advanced rectal cancer: a systematic review. World J Gastroenterol 20:6081–6091
Sharma K, Marcus JR (2013) Bevacizumab and wound-healing complications: mechanisms of action, clinical evidence, and management recommendations for the plastic surgeon. Ann Plast Surg 71:434–440
Ahn JW, Shalabi D, Correa-Selm LM, Dasgeb B, Nikbakht N, Cha J (2019) Impaired wound healing secondary to bevacizumab. Int Wound J 16:1009–1012
Singer AJ, Clark RA (1999) Cutaneous wound healing. N Engl J Med 341:738–746
Stavri GT, Zachary IC, Baskerville PA, Martin JF, Erusalimsky JD (1995) Basic fibroblast growth factor upregulates the expression of vascular endothelial growth factor in vascular smooth muscle cells. Synergistic interaction with hypoxia. Circulation 92:11–14
Honnegowda TM, Kumar P, Udupa EGP, Kumar S, Kumar U, Rao P (2015) Role of angiogenesis and angiogenic factors in acute and chronic wound healing. Plast Aesthet Res 2:243–249
Birkenhauer E, Neethirajan S (2015) A double-edged sword: the role of VEGF in wound repair and chemoattraction of opportunist pathogens. Int J Mol Sci 16:7159–7172
Akita Y, Kuroshima S, Nakajima K, Hayano H, Kanai R, Sasaki M, Sawase T (2018) Effect of anti-angiogenesis induced by chemotherapeutic monotherapy, chemotherapeutic/bisphosphonate combination therapy and anti-VEGFA mAb therapy on tooth extraction socket healing in mice. J Bone Miner Metab 36:547–559
Guo Z, Cui W, Que L, Li C, Tang X, Liu J (2020) Pharmacogenetics of medication-related osteonecrosis of the jaw: a systematic review and meta-analysis. Int J Oral Maxillofac Surg 49:298–309
Yang Q, McHugh KP, Patntirapong S, Gu X, Wunderlich L, Hauschka PV (2008) VEGF enhancement of osteoclast survival and bone resorption involves VEGF receptor-2 signaling and beta3-integrin. Matrix Biol 27:589–599
Aldridge SE, Lennard TW, Williams JR, Birch MA (2005) Vascular endothelial growth factor receptors in osteoclast differentiation and function. Biochem Biophys Res Commun 335:793–798
Yi T, Lee HL, Cha JH, Ko SI, Kim HJ, Shin HI, Woo KM, Ryoo HM, Kim GS, Baek JH (2008) Epidermal growth factor receptor regulates osteoclast differentiation and survival through cross-talking with RANK signaling. J Cell Physiol 217:409–422
Maeda H, Ito N, Yokoyama M, Kamiya M, Kameyama Y (1995) Immunohistochemical study of EGFR expression in the excisional wound of hamster tongue. Jpn J Stomatol 44:317–321
Higuchi T, Soga Y, Muro M, Kajizono M, Kitamura Y, Sendo T, Sasaki A (2018) Replacing zoledronic acid with denosumab is a risk factor for developing osteonecrosis of the jaw. Oral Surg Oral Med Oral Pathol Oral Radiol 125:547–551
Voss PJ, Steybe D, Poxleitner P, Schmelzeisen R, Munzenmayer C, Fuellgraf H, Stricker A, Semper-Hogg W (2018) Osteonecrosis of the jaw in patients transitioning from bisphosphonates to denosumab treatment for osteoporosis. Odontology 106:469–480
Owosho AA, Blanchard A, Levi L, Kadempour A, Rosenberg H, Yom SK, Farooki A, Fornier M, Huryn JM, Estilo CL (2016) Osteonecrosis of the jaw in patients treated with denosumab for metastatic tumors to the bone: a series of thirteen patients. J Craniomaxillofac Surg 44:265–270
Acknowledgements
We thank Editage (www.editage.jp) for their English language editing service.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Each author contributed to this study. Study concept: CK, KT, and HH Study design: CK and HH Data acquisition: CK, ME, TK, Y.K., and YW Quality control: TS and TK Data analysis and interpretation: CK, YK, and YW Statistical analysis: CK and TK Manuscript preparation and editing: CK and HH Manuscript review: HH and TK
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest.
Ethics approval
Ethical approval was obtained from the institutional review board of Fukushima Medical University Hospital (No. General 2020-010), and the study conformed to the tenets of the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Kanno, C., Kaneko, T., Endo, M. et al. Anti-VEGFR therapy is one of the healing inhibitors of antiresorptive-related osteonecrosis of the jaw. J Bone Miner Metab 39, 423–429 (2021). https://doi.org/10.1007/s00774-020-01170-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-020-01170-6