Abstract
Introduction
Primary hyperparathyroidism (PHPT), a third common endocrine disorder, varies from asymptomatic disease, mostly seen in the West where routine biochemical screening is practiced, to the classical symptomatic disease mostly seen in the Eastern countries. We aimed to compare the demographic, clinical, biochemical measurements in patients with asymptomatic and symptomatic PHPT from the Indian PHPT registry.
Material and methods
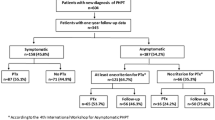
Data of PHPT patients from the last 25 years (1995–2019) were analyzed for demographic, clinical presentation and biochemical measurements, and compared these characteristics between asymptomatic and symptomatic PHPT patients.
Results
Of the 554 patients, 54 (10%) patients had asymptomatic PHPT. There was a sharp rise in the proportion of asymptomatic PHPT patients of 3% in the first decade to 13% in the second decade of the century (p = 0.003). Patients with asymptomatic PHPT were significantly older (50 vs. 42 years; p < 0.0001) and had higher mean body mass index (27.8 vs. 23.5 kg/m2; p < 0.0001) compared to the symptomatic PHPT group. In addition, asymptomatic PHPT patients had significantly lower median plasma iPTH (180 vs. 370 pg/mL; p < 0.0001), serum alkaline phosphatase (119 vs. 172 IU/L; p < 0.0001), and parathyroid adenoma weight (1.0 vs. 2.62 g; p = 0.006) compared to the symptomatic PHPT group.
Conclusion
Although symptomatic PHPT is still most prevalent (> 90%) in India with higher indices of the disease and tumor weights, there is a progressive rise in the prevalence of asymptomatic PHPT patients in the last decade. Improvements in calcium and vitamin D nutrition might account for this change as in the Western series.

Similar content being viewed by others
References
Fraser WD (2009) Hyperparathyroidism. Lancet 374:145–158
Wermers RA, Khosla S, Atkinson EJ, Achenbach SJ, Oberg AL, Grant CS et al (2006) Incidence of primary hyperparathyroidism in Rochester, Minnesota, 1993–2001: an update on the changing epidemiology of the disease. J Bone Miner Res 21:171–177
Bilezikian JP, Rubin M, Silverberg SJ (2006) Asymptomatic primary hyperparathyroidism. Arq Bras Endocrinol Metabol 50:647–656
Bandeira F, Cusano NE, Silva BC, Cassibba S, Almeida CB, Machado VC et al (2014) Bone disease in primary hyperparathyroidism. Arq Bras Endocrinol Metabol 58:553–561
Shah VN, Bhadada S, Bhansali A, Behera A, Mittal B (2014) Changes in clinical and biochemical presentations of primary hyperparathyroidism in India over a period of 20 years. Indian J Med Res 139:694–699
Gopal RA, Acharya SV, Bandgar T, Menon PS, Dalvi AN, Shah NS (2010) Clinical profile of primary hyperparathyroidism from western India: a single center experience. J Postgrad Med 56:79–84
Bhadada SK, Arya AK, Mukhopadhyay S, Khadgawat R, Sukumar S, Lodha S et al (2018) Primary hyperparathyroidism: insights from the Indian PHPT registry. J Bone Miner Metab 36:238–245
Hu S, Cai X, Mewani V, Wong B, Trooskin S, Wang X (2016) Impact of ethnic background on clinical characteristics and cardiovascular risk factors among patients with primary hyperparathyroidism. Endocr Pract 22:323–327
Shah VN, Bhadada SK, Bhansali A, Behera A, Mittal BR, Bhavin V (2012) Influence of age and gender on presentation of symptomatic primary hyperparathyroidism. J Postgrad Med 58:107–111
Jacob JJ, John M, Thomas N, Chacko A, Cherian R, Selvan B et al (2006) Does hyperparathyroidism cause pancreatitis? A South Indian experience and a review of published work. ANZ J Surg 76:740–744
Kapur MM, Agarwal MS, Gupta A, Misra MC, Ahuja MM (1985) Clinical and biochemical features of primary hyperparathyroidism. Indian J Med Res 81:607–612
Jha S, Jayaraman M, Jha A, Jha R, Modi KD, Kelwadee JV (2016) Primary hyperparathyroidism: a changing scenario in India. Indian J Endocrinol Metab 20:80–83
Sathe PA, Madiwale CV, Kandalkar BM, Bandgar TR, Shah NS, Menon PS (2009) Primary hyperparathyroidism: a clinicopathological experience. Indian J Pathol Microbiol 52:313–320
Pradeep PV, Jayashree B, Mishra A, Mishra SK (2011) Systematic review of primary hyperparathyroidism in India: the past, present, and the future trends. Int J Endocrinol 2011:921814
Arya AK, Bhadada SK, Mukherjee S, Singh P, Rana SS, Dahiya D et al (2018) Frequency and predictors of pancreatitis in symptomatic primary hyperparathyroidism. Indian J Med Res 148:721–727
Mukherjee S, Bhadada SK, Arya AK, Singh P, Sood A, Dahiya D et al (2018) Primary hyperparathyroidism in the young: comparison with adult primary hyperparathyroidism. Endocr Pract 24:1051–1056
Singh P, Vadi SK, Saikia UN, Sood A, Dahiya D, Arya AK et al (2019) Minimally invasive parathyroid carcinoma—a missing entity between parathyroid adenoma and carcinoma: scintigraphic and histological features. Clin Endocrinol (Oxf) 91:842–850
Zhao L, Liu JM, He XY, Zhao HY, Sun LH, Tao B et al (2013) The changing clinical patterns of primary hyperparathyroidism in Chinese patients: data from 2000 to 2010 in a single clinical center. J Clin Endocrinol Metab 98:721–728
Sun B, Guo B, Wu B, Kang J, Deng X, Zhang Z et al (2018) Characteristics, management, and outcome of primary hyperparathyroidism at a single clinical center from 2005 to 2016. Osteoporos Int 29:635–642
Mithal A, Kaur P, Singh VP, Sarin D, Rao DS (2015) Asymptomatic primary hyperparathyroidism exists in North India: retrospective data from 2 tertiary care centers. Endocr Pract 21:581–585
Rao DS, Honasoge M, Divine GW, Phillips ER, Lee MW, Ansari MR et al (2000) Effect of vitamin D nutrition on parathyroid adenoma weight: pathogenetic and clinical implications. J Clin Endocrinol Metab 85:1054–1058
Rao DS, Agarwal G, Talpos GB, Phillips ER, Bandeira F, Mishra SK et al (2002) Role of vitamin D and calcium nutrition in disease expression and parathyroid tumor growth in primary hyperparathyroidism: a global perspective. J Bone Miner Res 17(Suppl 2):N75–N80
Harinarayan CV, Gupta N, Kochupillai N (1995) Vitamin D status in primary hyperparathyroidism in India. Clin Endocrinol (Oxf) 43:351–358
Parfitt AM, Rao DS, Kleerekoper M (1988) Screening for primary hyperparathyroidism. Ann Intern Med 108:151–152
Silverberg SJ, Bilezikian JP (2006) The diagnosis and management of asymptomatic primary hyperparathyroidism. Nat Clin Pract Endocrinol Metab 2:494–503
Bilezikian JP, Khan AA, Potts JT Jr (2009) Third International Workshop on the Management of Asymptomatic Primary H. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the third international workshop. J Clin Endocrinol Metab 94:335–339
Khan AA, Hanley DA, Rizzoli R, Bollerslev J, Young JE, Rejnmark L et al (2017) Primary hyperparathyroidism: review and recommendations on evaluation, diagnosis, and management. A Canadian and international consensus. Osteoporos Int 28:1–19
Bandeira F, Griz L, Caldas G, Bandeira C, Freese E (2006) From mild to severe primary hyperparathyroidism: the Brazilian experience. Arq Bras Endocrinol Metabol 50:657–663
Mallikarjuna VJ, Mathew V, Ayyar V, Bantwal G, Ganesh V, George B et al (2018) Five-year retrospective study on primary hyperparathyroidism in South India: emerging roles of minimally invasive parathyroidectomy and preoperative localization with methionine positron emission tomography-computed tomography scan. Indian J Endocrinol Metab 22:355–361
Ogo A, Sakaki Y, Saito R, Sakamoto R, Matoba Y (2014) A pilot study to examine the management of asymptomatic hyperparathyroidism in Japanese patients in accordance with the guidelines for asymptomatic PHPT proposed at the Third International Workshop in 2008. Intern Med 53:1749–1754
Prasarttong-Osoth P, Wathanaoran P, Imruetaicharoenchoke W, Rojananin S (2012) Primary hyperparathyroidism: 11-year experience in a single institute in Thailand. Int J Endocrinol 2012:952426
Kobayashi T, Sugimoto T, Chihara K (1997) Clinical and biochemical presentation of primary hyperparathyroidism in Kansai district of Japan. Endocr J 44:595–601
Makay O, Ozcinar B, Simsek T, Arici C, Gungor B, Ozbas S et al (2017) Regional clinical and biochemical differences among patients with primary hyperparathyroidism. Balkan Med J 34:28–34
Siddiqui MI, Pasha HA, Asad R, Talati JJ (2019) Changing paradigms in the surgical management of hyperparathyroidism at a tertiary care hospital in a developing country. J Pak Med Assoc 69:1360–1364
Tay YK, Khoo J, Chandran M (2016) Surgery or no surgery: What works best for the kidneys in primary hyperparathyroidism? A study in a multi-ethnic Asian population. Indian J Endocrinol Metab 20:55–61
Saponaro F, Cetani F, Repaci A, Pagotto U, Cipriani C, Pepe J et al (2018) Clinical presentation and management of patients with primary hyperparathyroidism in Italy. J Endocrinol Investig 41:1339–1348
Aresta C, Passeri E, Corbetta S (2019) Symptomatic hypercalcemia in patients with primary hyperparathyroidism is associated with severity of disease, polypharmacy, and comorbidity. Int J Endocrinol 2019:7617254
Silverberg SJ, Walker MD, Bilezikian JP (2013) Asymptomatic primary hyperparathyroidism. J Clin Densitom 16:14–21
Walker MD, Cong E, Lee JA, Kepley A, Zhang C, McMahon DJ et al (2015) Vitamin D in primary hyperparathyroidism: effects on clinical, biochemical, and densitometric presentation. J Clin Endocrinol Metab 100:3443–3451
Rao DS, Phillips ER, Divine GW, Talpos GB (2004) Randomized controlled clinical trial of surgery versus no surgery in patients with mild asymptomatic primary hyperparathyroidism. J Clin Endocrinol Metab 89:5415–5422
Locchi F, Tommasi M, Brandi ML, Tonelli F, Meldolesi U (1997) A controversial problem: is there a relationship between parathyroid hormone level and parathyroid size in primary hyperparathyroidism? Int J Biol Mark 12:106–111
Acknowledgements
No fund was received for conducting the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest.
Ethical approval
The study was approved by the Institutional Ethics committee, Postgraduate Institute of Medical Education and Research, Chandigarh India (INT/IEC/2016/2254 dated 27-09-2016). Informed written consent was obtained from all study participants. The study was carried out in accordance with the approved institutional and international research ethics guidelines.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Arya, A.K., Kumari, P., Bhadada, S.K. et al. Progressive rise in the prevalence of asymptomatic primary hyperparathyroidism in India: Data from PHPT registry. J Bone Miner Metab 39, 253–259 (2021). https://doi.org/10.1007/s00774-020-01142-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-020-01142-w