Summary
Background
Acute inflammatory disorders of the orbit can cause not only blindness but also intracranial complications that directly threaten the patient’s life. Accurate and timely diagnosis of the type of orbital lesion is necessary for determining the treatment tactics.
Methods
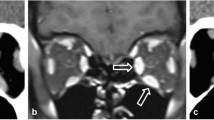
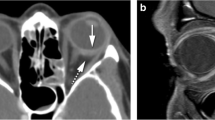
The clinical and tomographical data of 57 patients with acute inflammatory disorders of the orbit were analyzed prospectively (2008–2017) along with the data of 37 patients analyzed retrospectively (1999–2007). Morphometric and functional parameters of the patients’ orbits on the healthy side were used as a control group (94 orbits). All patients underwent visometry, biomicroscopy, ophthalmoscopy, measuring the width of the palpebral fissure in the central part, and exophthalmometry, measuring the lateral displacement of the eyeball. All patients underwent computed tomography examination. The scanning was performed in axial, coronary, and orbitomeatal projections with a step size of 1 mm.
Results
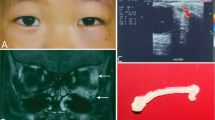
Osteoperiostitis and subperiostal abscess were characterized by moderate pathological changes of the eyelids and orbital soft tissues and normal visual functions. Retrobulbar infiltrate and edema of orbital cellular tissue were characterized by pathological changes of the eyelids and orbital soft tissues and a decrease in visual acuity in 42.9% of cases of edema of the orbital tissue.. Orbital abscess and phlegmon of the orbit were characterized by heavily expressed pathological changes of the eyelids and orbital soft tissues and a marked decrease in visual acuity in all patients with phlegmon of the orbital.
Conclusion
Clarification of the type of orbital inflammatory disease via the clinical and tomographic criteria determined in this study led to a decrease in the number of unjustified transcutaneous orbitotomy procedures.
Zusammenfassung
Hintergrund
Akute entzündliche Erkrankungen der Orbita können nicht nur Blindheit verursachen, sondern auch intrakranielle Komplikationen, die für den Patienten unmittelbar lebensbedrohlich sind. Eine genaue und zügige Diagnose der Art einer Orbitaläsion ist notwendig, um die Behandlungsstrategie festzulegen.
Methoden
Prospektiv wurden die klinischen und tomographischen Daten von 57 Patienten mit akuter entzündlicher Erkrankung der Orbita ausgewertet (2008–2017), damit einher ging die retrospektive Analyse der Daten von 37 Patienten (1999–2007). Morphometrische und funktionelle Parameter der Orbitae der Patienten auf der gesunden Seite dienten als Kontrollgruppe (94 Orbitae). Bei allen Patienten wurde eine Visometrie, Biomikroskopie, Ophthalmoskopie, Messung der Lidspaltenweite im zentralen Bereich, Exophthalmometrie und Messung der lateralen Abweichung des Augapfels durchgeführt. Auch erfolgte bei sämtlichen Patienten eine computertomographische Untersuchung. Die Aufnahmen wurden in axialer, koronarer und orbitomeataler Projektion mit einer Schichtdicke von 1 mm durchgeführt.
Ergebnisse
Osteoperiostitis und subperiostaler Abszess waren durch mittelgradige pathologische Veränderungen der Augenlider und Orbitaweichgewebe bei normalen Sehleistungen gekennzeichnet. Ein retrobulbäres Infiltrat und Ödem der orbitalen Zellgewebe zeichneten sich durch pathologische Veränderungen der Augenlider und der Orbitalweichgewebe sowie in 42,9% der Fälle mit Ödem des Orbitagewebes durch eine Abnahme der Sehschärfe aus. Charakteristisch für einen Orbitaabszess und eine Orbitaphlegmone waren schwergradige pathologische Veränderungen der Augenlider und der Orbitaweichgewebe sowie eine deutliche Abnahme der Sehschärfe bei allen Patienten mit Orbitaphlegmone.
Schlussfolgerung
Die Abklärung der Art einer entzündlichen Erkrankung der Orbita anhand der klinischen und tomographischen Kriterien, die in der vorliegenden Studie ermittelt wurden, führte zu einer Abnahme der Anzahl ungerechtfertigter transkutaner Orbitotomieoperationen.






Similar content being viewed by others
References
Uy H, Tuan P. Preseptal and orbital cellulitis in a developing country. Orbit. 2007;26:33–7.
Das J, Choudhury B, Medhi J. Orbital abscess and hemi-occlusion of the central retinal vein in a child. Orbit. 2007;26:295–7.
Luemsamran P, Pornpanich K, Vangveeravong S, et al. Orbital cellulitis and endophthalmitis in pseudomonas septicemia. Orbit. 2008;27:455–7.
Lip P, Moutsou M, Hero M. A postoperative complication far worse than endophthalmitis: the coexistence of orbital cellulitis. Br J Ophthalmol. 2001;85:625–33.
Carter K, Lee A, Tang R, et al. Neuro-ophthalmologic complications of sinus surgery. Neuroophthalmology. 1998;19(2):75–82.
Muhtaseb M, Marjanovic B, Waddilove L, et al. Cavernous sinus thrombosis secondary to MRSA septicaemia. Neuroophthalmology. 2004;28(5):245–50.
Goawalla A, Mansell N, Pearson A. Septic cavernous sinus thrombosis with bilateral secondary orbital infection. Orbit. 2007;26:113–6.
Harstein M, Steinvurzel M, Cohen C. Intracranial abscess as a complication of subperiostal abscess of the orbit. Ophthalmol Plast Reconstr Surg. 2001;17(6):398–403.
Murphy C, Livingstone I, Foot B, et al. Orbital cellulitis in Scotland: current incidence, aetiology, management and outcomes. Br J Ophthalmol. 2014;98:1575–8.
Chaudhry I, Shamsi F, Elzaridi E, et al. Outcome of treated orbital cellulitis in a tertiary eye care center in the Middle East. Ophthalmology. 2007;114:345–54.
Dissel J, de Keizer J. Bacterial infections of the orbit. Orbit. 1998;17(4):227–35.
Briscoe D, Cruz A. A new classification of orbital cellulitis. Book of Abstracts 10th Congress of International Ocular Inflammation Society Prague; 30.05.–02.06.. 2009. p. 51.
Harris G. Subperiosteal abscess of the orbit. Arch Ophthalmol. 1983;101:751–7.
Stubinger S, Leiggener C, Sader R, et al. Intraorbital abscess. J Am Dent Assoc. 2005;136(7):921–5.
Group C, Ong C, Chew N, Syrimi M, et al. Streptococcal subperiosteal abscess of the orbit. Orbit. 2009;28:160–1.
Shibasakii H, Hayasakaiy S, Setogawa T, et al. Ophthalmic complications in patients with paranasal sinusitis. Orbit. 1992;11(1):1–5.
Blake F, Siegert I, Wed I, et al. The acute orbit: etiology, diagnosis, and therapy. J Oral Maxillofac Surg. 2006;64(1):87–93.
Pereira F, Cruz A, Teresinha A, et al. Computed tomographic patterns of orbital cellulitis due to sinusitis. Arq Bras Oftalmol. 2006;69(4):513–8.
Harris G. Subperiosteal abscess of the orbit: computed tomography and the clinical course. Ophthal Plast Reconstr Surg. 1996;12:1–8.
Wang C, Chen D. Diagnostic significance of CT in the orbital inflammatory lesions. Zhonghua Yan Ke Za Zhi. 1996;5:366–8.
Leib M, Cooper W, Mai P, et al. Volume determination of the orbit with high resolution CT scans and quantitative digital image analysis. Orbit. 1982;1(3):149.
Garcia G, Harris G. Criteria for nonsurgical management of subperiosteal abscess of the orbit: analysis of outcomes 1988–1998. Ophthalmology. 2000;107(8):1454–8.
Harris G. Subperiosteal abscess of the orbit: age as a factor in the bacteriology and response to treatment. Ophthalmology. 1994;101:585–95.
Harris G. Subperiosteal abscess of the orbit: older children and adults require aggressive treatment. Ophthal Plast Reconstr Surg. 2001;17:395–7.
Hatano A, Shiva A. Surgical treatment of subperiostal abscess of the orbit. Nippon Libiinkoko Gakkai Kaiho. 2006;109(5):447–54.
Pakdaman MN, Sepahdari AR, Elkhamary SM. Orbital inflammatory disease: pictorial review and differential diagnosis. World J Radiol. 2014;6(4):106–15.
Mary K. Jacob Idiopathic orbital inflammatory disease. Oman J Ophthalmol. 2012;5(2):124–5.
Weber AL, Romo LV, Sabates NR. Pseudotumor of the orbit. Clinical, pathologic, and radiologic evaluation. Radiol Clin North Am. 1999;37(1):151–68.
Rumelt S, Rubin P. Potential sources for orbital cellulitis. Int Ophthalmol Clin. 1996;36(3):207–21.
Dhariwal D, Kittur M, Farrier J, et al. Post-traumatic orbital cellulitis. Br J Oral Maxillofac Surg. 2003;41:21–8.
Maheshwari R, Maheshwari S, Shah T. Acute dacryocystitis causing orbital cellulitis and abscess. Orbit. 2009;28:196–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
D. Zubkova, P. Bezditko, O. Zavoloka, Y. Ilyina, and O. Zubkov declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zubkova, D., Bezditko, P., Zavoloka, O. et al. Clinical and tomographic features of acute inflammatory disorders of the orbit. Spektrum Augenheilkd. 34, 10–17 (2020). https://doi.org/10.1007/s00717-019-0426-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00717-019-0426-0