Summary
Purpose
To assess the efficacy of intravitreally injected tissue plasminogen activator (t-PA, Alteplase [Actilyse®]) to induce posterior vitreous detachment (PVD) in eyes with recent onset of retinal vein occlusion (RVO).
Methods
Retrospective patient chart analysis.
Results
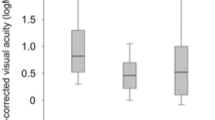
Nine eyes were included thereof 4 eyes (44%) with central (CRVO) and 5 eyes (56%) with branch RVO (BRVO). One week after injection none of the eyes treated showed PVD formation. After 12 months one patient (17%) developed partial PVD and two patients (33%) demonstrated complete PVD. All eyes developing (partial) PVD after one year suffered from BRVO. Mean best corrected visual acuity (BCVA) increased from 0.35 to 0.45 after one week (p = 0.401) and further to 1.0 after 12 months (p = 0.042). There was an overall significant gain in mean BCVA development after 12 months (p = 0.015). Mean central retinal thickness decreased from 572 to 485 µm after one week (p = 0.374) and further to 299 µm after 12 months (p = 0.345). There was an overall significant decrease in CRT development from injection until month 12 (p = 0.030).
Conclusion
Intravitreally injected Actilyse® might have the potential to induce PVD in eyes with recent onset of RVO and might favorably impact standard treatment regimens. A prospective and randomized clinical trial is needed to prove this hypothesis.
Zusammenfassung
Zielsetzung
Ziel der Studie war es, die Wirksamkeit einer intravitrealen Injektion des Gewebeplasminogenaktivators (t-PA, Alteplase [Actilyse®]) bezüglich der Induktion einer hinteren Glaskörperabhebung (HGA) in Augen mit kürzlich aufgetretenem retinalem Venenverschluss (RVV) zu untersuchen.
Material und Methoden
Retrospektive Analyse von Patientenakten.
Ergebnisse
In die Studie wurden 9 Augen eingeschlossen, davon 4 (44%) mit Zentralvenenverschluss (ZVV) und 5 (56%) mit Venenastverschluss (VAV). Eine Woche nach Injektion war in keinem der behandelten Augen die Entwicklung einer HGA zu beobachten. Nach 12 Monaten fand sich bei einem Patienten (17%) eine partielle HGA, bei 2 Patienten (33%) eine komplette HGA. In allen Augen mit (partieller) HGA nach einem Jahr bestand ein VAV. Der Mittelwert der bestkorrigierten Sehschärfe stieg von 0,35 auf 0,45 nach einer Woche (p = 0,401) und weiter auf 1,0 nach 12 Monaten (p = 0,042). Es fand sich eine insgesamt signifikante Zunahme des Mittelwerts der bestkorrigierten Sehschärfe nach 12 Monaten (p = 0,015). Die mittlere zentrale Netzhautdicke sank von 572 auf 485 µm nach einer Woche (p = 0,374) und weiter auf 299 µm nach 12 Monaten (p = 0,345). Es fand sich eine insgesamt signifikante Abnahme der zentralen Netzhautdicke von der Injektion bis 12 Monate danach (p = 0,030).
Schlussfolgerung
Die intravitreale Injektion von Actilyse® könnte in Augen mit kürzlich aufgetretenem RVV eine HGA induzieren und die standardmäßigen Behandlungsregime günstig beeinflussen. Eine prospektive und randomisierte klinische Studie ist erforderlich, um diese Hypothese zu belegen.



Similar content being viewed by others
References
Bertelmann T, Kičová N, Messerschmidt-Roth A, Irle S, Sekundo W, Mennel S. The vitreomacular interface in retinal vein occlusion. Acta Ophthalmol. 2011;89:e327–e31.
Bertelmann T, Bertelmann I, Szurman P, Mester U, Schmidt J, Sekundo W, Mennel S. vitreous body and retinal vein occlusion. Ophthalmologe. 2014 Dec;111(12):1178–82. doi:10.1007/s00347-014-3086-0.
Hikichi T, Konno S, Trempe CL. Role of the vitreous in central retinal vein occlusion. Retina. 1995;15:29–33.
Takahashi MK, Hikichi T, Akiba J, Yoshida A, Trempe CL. Role of the vitreous and macular edema in branch retinal vein occlusion. Ophthalmic Surg Lasers. 1997;28:294–9.
Akiba J, Kado M, Kakehashi A, Trempe CL. Role of the vitreous in posterior segment neovascularization in central retinal vein occlusion. Ophthalmic Surg. 1991;22:498–502.
Kado M, Jalkh AE, Yoshida A, Takahashi M, Wazen N, Trempe CL, Schepens CL. Vitreous changes and macular edema in central retinal vein occlusion. Ophthalmic Surg. 1990;21:544–9.
Tachi N, Hashimoto Y, Ogino N. Vitrectomy for macular edema combined with retinal vein occlusion. Doc Ophthalmol. 1999;97:465–9.
Charbonnel J, Glacet-Bernard A, Korobelnik JF, Nyouma-Moune E, Pournaras CJ, Colin J, Coscas G, Soubrane G. Management of branch retinal vein occlusion with vitrectomy and arteriovenous adventitial sheathotomy, the possible role of surgical posterior vitreous detachment. Graefes Arch Clin Exp Ophthalmol. 2004;242:223–8.
Avunduk AM, Cetinkaya K, Kapicioğlu Z, Kaya C. The effect of posterior vitreous detachment on the prognosis of branch retinal vein occlusion. Acta Ophthalmol Scand. 1997;75:441–2.
Noma H, Funatsu H, Mimura T, Shimada K. Visual acuity and foveal thickness after vitrectomy for macular edema. Ophthalmologica. 2010;224:367–73.
Noma H, Funatsu H, Mimura T, Eguchi S, Shimada K. Visual acuity and foveal thickness after vitrectomy for macular edema associated with branch retinal vein occlusion: a case series. BMC Ophthalmol. 2010;10:11.
Stalmans P, Benz MS, Gandorfer A, Kampik A, Girach A, Pakola S, Haller JA, Group M. Enzymatic vitreolysis with ocriplasmin for vitreomacular traction and macular holes. N Engl J Med. 2012;367:606–15.
DOG, Retinologische Gesellschaft, BVA. Durchführung von intravitrealen Injektionen (IVI). Empfehlung der DOG, der Retinologischen Gesellschaft und des BVA. (Juli 2007).
Kičová N, Bertelmann T, Irle S, Sekundo W, Mennel S. Evaluation of a posterior vitreous detachment: a comparison of biomicroscopy, b‑scan ultrasonography and optical coherence tomography to surgical findings with chromodissection. Acta Ophthalmol. 2012;90:e264–e8.
Gandorfer A. Pharmacologic vitreolysis. Dev Ophthalmol. 2007;39:149–56.
Murakami T, Takagi H, Ohashi H, Kita M, Nishiwaki H, Miyamoto K, Watanabe D, Sakamoto A, Yamaike N, Yoshimura N. Role of posterior vitreous detachment induced by intravitreal tissue plasminogen activator in macular edema with central retinal vein occlusion. Retina. 2007;27:1031–7.
Murakami T, Takagi H, Kita M, Nishiwaki H, Miyamoto K, Ohashi H, Watanabe D, Yoshimura N. Intravitreal tissue plasminogen activator to treat macular edema associated with branch retinal vein occlusion. Am J Ophthalmol. 2006;142:318–20.
Glacet-Bernard A, Kuhn D, Vine AK, Oubraham H, Coscas G, Soubrane G. Treatment of recent onset central retinal vein occlusion with intravitreal tissue plasminogen activator: a pilot study. Br J Ophthalmol. 2000;84:609–13.
Bertelmann T, Mennel S, Sekundo W, Strodthoff S, Witteborn MC, Stief T, Nguyen N, Koss MJ. Intravitreal functional plasminogen is elevated in central retinal vein occlusion. Ophthalmic Res. 2013;50:151–9.
Bertelmann T, Stief T, Bölöni R, Schulze S, Wenner Y, Sekundo W, Mennel S. Fibrinolysis in normal vitreous liquid. Blood Coagul Fibrinolysis. 2014 Apr;25(3):217–20. doi:10.1097/MBC.0000000000000022.
Bertelmann T, Sekundo W, Strodthoff S, Witteborn MC, Stief T, Irle S, Nguyen N, Koss MJ, Mennel S. Intravitreal functional plasminogen in eyes with branch retinal vein occlusion. Ophthalmic Res. 2014;52:74–80.
Bertelmann T, Stief T, Sekundo W, Witteborn M, Strodthoff S, Mennel S, Nguyen N, Koss M. intravitreal fibrinolysis and retinal vein occlusion. Ophthalmologe. 2015; 112(2):155–61. doi:10.1007/s00347-014-3107-z.
Gutman FA, Zegarra H. Macular edema secondary to occlusion of the retinal veins. Surv Ophthalmol. 1984;28(Suppl):462–70.
Ghazi NG, Noureddine B, Haddad RS, Jurdi FA, Bashshur ZF. Intravitreal tissue plasminogen activator in the management of central retinal vein occlusion. Retina. 2003;23:780–4.
Tagami M, Kusuhara S, Imai H, Honda S, Tsukahara Y, Negi A. Impact of intravitreal injection of tissue plasminogen activator on full-field electroretinogram in patients with macular oedema secondary to retinal vein occlusion. Ophthalmologica. 2011;226:81–6.
Yamamoto T, Kamei M, Kunavisarut P, Suzuki M, Tano Y. Increased retinal toxicity of intravitreal tissue plasminogen activator in a central retinal vein occlusion model. Graefes Arch Clin Exp Ophthalmol. 2008;246:509–14.
Murakami T, Tsujikawa A, Ohta M, Miyamoto K, Kita M, Watanabe D, Takagi H, Yoshimura N. Photoreceptor status after resolved macular edema in branch retinal vein occlusion treated with tissue plasminogen activator. Am J Ophthalmol. 2007;143:171–3.
Rowley SA, Vijayasekaran S, Yu PK, McAllister IL, Yu DY. Retinal toxicity of intravitreal tenecteplase in the rabbit. Br J Ophthalmol. 2004;88:573–8.
Chen SN, Yang TC, Ho CL, Kuo YH, Yip Y, Chao AN. Retinal toxicity of intravitreal tissue plasminogen activator: case report and literature review. Ophthalmology. 2003;110:704–8.
Jaffe GJ, Green GD, McKay BS, Hartz A, Williams GA. Intravitreal clearance of tissue plasminogen activator in the rabbit. Arch Ophthalmol. 1988;106:969–72.
Weber-Krause B, Eckardt C. incidence of posterior vitreous detachment in the elderly. Ophthalmologe. 1997;94:619–23.
Geck U, Pustolla N, Baraki H, Atili A, Feltgen N, Hoerauf H. Posterior vitreous detachment following intravitreal drug injection. Graefes Arch Clin Exp Ophthalmol. 2013;251:1691–5.
Elman MJ, Raden RZ, Carrigan A. Intravitreal injection of tissue plasminogen activator for central retinal vein occlusion. Trans Am Ophthalmol Soc. 2001;99:219–21, discussion 222–213.
Lahey JM, Fong DS, Kearney J. Intravitreal tissue plasminogen activator for acute central retinal vein occlusion. Ophthalmic Surg Lasers. 1999;30:427–34.
Figueroa MS, Ruiz Moreno JM. bravo and cruise: Ranibizumab for the treatment of macular edema secondary to retinal vein occlusion. Arch Soc Esp Oftalmol. 2012;87(Suppl 1):46–53.
Ogura Y, Roider J, Korobelnik JF, Holz FG, Simader C, Schmidt-Erfurth U, Vitti R, Berliner AJ, Hiemeyer F, Stemper B, Zeitz O, Sandbrink R, Group GS. Intravitreal aflibercept for macular edema secondary to central retinal vein occlusion: 18-month results of the phase 3 galileo study. Am J Ophthalmol. 2014;158:1032–1038.e1032.
Haller JA, Bandello F, Belfort R, Blumenkranz MS, Gillies M, Heier J, Loewenstein A, Yoon YH, Jacques ML, Jiao J, Li XY, Whitcup SM, Group OGS. Randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology. 2010;117:1134–1146.e1133.
Haller JA, Bandello F, Belfort R, Blumenkranz MS, Gillies M, Heier J, Loewenstein A, Yoon YH, Jiao J, Li XY, Whitcup SM, Li J, Group OGS. Dexamethasone intravitreal implant in patients with macular edema related to branch or central retinal vein occlusion twelve-month study results. Ophthalmology. 2011;118:2453–60.
Aiello LP, Avery RL, Arrigg PG, Keyt BA, Jampel HD, Shah ST, Pasquale LR, Thieme H, Iwamoto MA, Park JE. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med. 1994;331:1480–7.
McAllister IL, Vijayasekaran S, Yu DY. Intravitreal tenecteplase (metalyse) for acute management of retinal vein occlusions. Invest Ophthalmol Vis Sci. 2013;54:4910–8.
Kamei M, Misono K, Lewis H. A study of the ability of tissue plasminogen activator to diffuse into the subretinal space after intravitreal injection in rabbits. Am J Ophthalmol. 1999;128:739–46.
Mahmoud TH, Peng YW, Proia AD, Davidson M, Deramo VA, Fekrat S. Recombinant tissue plasminogen activator injected into the vitreous cavity may penetrate the retinal veins of a porcine model of vascular occlusion. Br J Ophthalmol. 2006;90:911–5.
Üney G, Ünlü N, Acar MA, Hazirolan D, Altiparmak UE, Yalniz-Akkaya Z, Örnek F. Role of posterior vitreous detachment on outcome of anti-vascular endothelial growth factor treatment in age-related macular degeneration. Retina. 2014;34:32–7.
de Smet MD, Gad Elkareem AM, Zwinderman AH. The vitreous, the retinal interface in ocular health and disease. Ophthalmologica. 2013;230:165–78.
Lee SS, Ghosn C, Yu Z, Zacharias LC, Kao H, Lanni C, Abdelfattah N, Kuppermann B, Csaky KG, D’Argenio DZ, Burke JA, Hughes PM, Robinson MR. Vitreous vegf clearance is increased after vitrectomy. Invest Ophthalmol Vis Sci. 2010;51:2135–8.
Gandorfer A, Putz E, Welge-Lüssen U, Grüterich M, Ulbig M, Kampik A. Ultrastructure of the vitreoretinal interface following plasmin assisted vitrectomy. Br J Ophthalmol. 2001;85:6–10.
Funatsu H, Yamashita H, Ikeda T, Mimura T, Eguchi S, Hori S. Vitreous levels of interleukin-6 and vascular endothelial growth factor are related to diabetic macular edema. Ophthalmology. 2003;110:1690–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
T. Bertelmann, S. Strodthoff, W. Sekundo and S. Mennel declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Bertelmann, T., Strodthoff, S., Sekundo, W. et al. Intravitreal Actilyse® injection to induce posterior vitreous detachment in eyes with recent onset of retinal vein occlusion. Spektrum Augenheilkd. 32, 39–45 (2018). https://doi.org/10.1007/s00717-017-0351-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00717-017-0351-z
Keywords
- Ocriplasmin
- Alteplase
- Vitreomacular traction (VMT)
- Vitreomacular adhesion (VMA)
- Optical coherence tomography (OCT)