Summary
Background
To evaluate the efficacy and safety of intravitreal bevacizumab injections in patients with pigment epithelial detachments (PEDs) secondary to age-related macular degeneration (AMD).
Material and methods
In a retrospective interventional case series, 62 eyes of 61 patients were treated with 1.5 mg bevacizumab intravitreally. Baseline and follow-up visits included best-corrected visual acuity and optical coherence tomography (OCT) examinations. Follow-up visits were performed 1, 3, and 6 months after initial treatment. Morphological effects on PED were quantified by repetitively measuring the highest elevation on two perpendicular OCT cross-sections. If height of PED was increased by 50 microns, or intraretinal fluid appeared or increased, or visual acuity decreased more than 5 letters on the Early Treatment Diabetic Retinopathy Study (ETDRS) chart, patients were reinjected.
Results
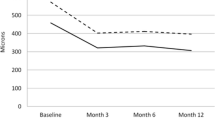
On OCT, PED decreased from 346 ± 148 µm at baseline to 241 ± 159 µm (p < 0.001) at 1 month, 227 ± 193 µm (p < 0.001) at 3 months, and 166 ± 170 µm (p < 0.001) at 6 months. Mean best corrected visual acuity (BCVA) increased from 49 ± 18 letters at baseline to 52 ± 21 letters (p = 0.062) at 1 month. However, 3 and 6 months after initial injection mean BCVA returned to baseline levels (3 months: 49 ± 19 letters, p = 0.518; 6 months: 49 ± 20 letters, p = 0.053). On average, patients received 2.5 injections during the observation period of 6 months. Except for one retinal pigment epithelial (RPE) tear no other ocular or systemic adverse events were noticed. Ocular inflammation was not found in any of the investigated patients.
Conclusions
The presented data demonstrate a therapeutic effect of intravitreal bevacizumab in patients with specific classes of pigment epithelial detachments secondary to AMD.
Zusammenfassung
Hintergrund
Untersuchung der Wirksamkeit und Sicherheit von intravitrealen Bevacizumab-Injektionen bei Patienten mit Pigmentepithelabhebungen (PED) bei altersabhängiger Makuladegeneration (AMD).
Material und Methoden
In einer retrospektiven, interventionelle Fallserie wurden 62 Augen von 61 Patienten mit 1,5 mg intravitreal appliziertem Bevacizumab behandelt. Bei der Ausgangsuntersuchung und den Follow-up-Untersuchungen wurde die bestkorrigierte Sehschärfe bestimmt und eine optische Kohärenztomographie durchgeführt. Follow-up-Untersuchungen wurden 1, 3 und 6 Monate nach der ersten Behandlung durchgeführt. Morphologische Effekte auf die PED wurden in der OCT durch wiederholtes Messen der höchsten Erhebung auf zwei im rechten Winkel zueinander aufgenommenen OCT-Schnittbildern quantifiziert. Bei den Patienten wurden erneute Injektionen durchgeführt, wenn die Höhe der PED um mehr als 50 Mikrometer zunahm oder intraretinale Flüssigkeit entstand oder sich vermehrte oder wenn die Sehschärfe mehr als 5 Buchstaben auf den ETDRS Tafeln abnahm.
Ergebnisse
In der OCT reduzierte sich die Höhe der PED von 346 ± 148 μm bei Studienbeginn auf 241 ± 159 μm (p < 0,001) nach 1 Monat, 227 ± 193 μm (p < 0,001) nach 3 Monaten und 166 ± 170 μm (p < 0,001) nach 6 Monaten. Die mittlere bestkorrigierte Sehschärfe (BCVA) erhöhte sich von 49 ± 18 Buchstaben bei Studienbeginn auf 52 ± 21 Buchstaben (p = 0,062) nach einem Monat. Nach 3 und 6 Monaten nach der ersten Injektion fiel die BCVA jedoch wieder auf das Ausgangsniveau ab (3 Monate: 49 ± 19 Buchstaben, p = 0,518; 6 Monate: 49 ± 20 Buchstaben, p = 0,053). Im Durchschnitt erhielten die Patienten 2,5 Injektionen während der Beobachtungszeit von 6 Monaten. Außer einem Riss des retinalen Pigmentepithels (RPE) wurden keine anderen okulären oder systemischen Nebenwirkungen festgestellt. Okuläre Entzündungen wurden bei keinem der untersuchten Patienten gefunden.
Schlussfolgerungen
Die vorgestellten Daten zeigen einen therapeutischen Effekt der intravitrealen Bevacizumab-Applikation bei Patienten mit spezifischen Klassen von Pigmentepithelabhebungen bei AMD.













Similar content being viewed by others
References
Poliner LS, Olk RJ, Burgess D, Gordon ME. Natural history of retinal pigment epithelial detachments in age-related macular degeneration. Ophthalmology. 1986;93(5):543–51.
Meredith TA, Braley RE, Aaberg TM. Natural history of serous detachments of the retinal pigment epithelium. Am J Ophthalmol. 1979;88(4):643–51.
Elman MJ, Fine SL, Murphy RP, et al. The natural history of serous retinal pigment epithelium detachment in patients with age-related macular degeneration. Ophthalmology. 1986;93(2):224–30.
Verhoeff FH, Grossman HP. The pathogenesis of disciform degeneration of the macula. Trans Am Ophthalmol Soc. 1937;35:262–94.
Murphy RP, Yeo JH, Green WR, Patz A. Dehiscences of the pigment epithelium. Trans Am Ophthalmol Soc. 1985;83:63–81.
Green WR, McDonnell PJ, Yeo JH. Pathologic features of senile macular degeneration. Retina. 1985(2005);25(5 Suppl):615–27.
Pauleikhoff D, Harper CA, Marshall J, Bird AC. Aging changes in Bruch’s membrane. A histochemical and morphologic study. Ophthalmology. 1990;97(2):171–8.
Bird AC, Marshall J. Retinal pigment epithelial detachments in the elderly. Trans Ophthalmol Soc U K. 1986;105(Pt 6):674–82.
Gass JD. Serous retinal pigment epithelial detachment with a notch: a sign of occult choroidal neovascularization. Retina. 1984(2003);23(6 Suppl):205–20.
The Moorfields Macular Study Group. Retinal pigment epithelial detachments in the elderly. A controlled trial of argon laser photocoagulation. Br J Ophthalmol. 1982;66(1):1–16.
Pece A, Isola V, Vadala M, Calori G. Photodynamic therapy with verteporfin for choroidal neovascularization associated with retinal pigment epithelial detachment in age-related macular degeneration. Retina. 2007;27(3):342–8.
Axer-Siegel R, Ehrlich R, Avisar I, et al. Combined photodynamic therapy and intravitreal triamcinolone acetonide injection for neovascular age-related macular degeneration with pigment epithelium detachment. Ophthalmic Surg Lasers Imaging. 2006;37(6):455–61.
Lommatzsch AP, Heimes B, Gutfleisch M, et al. Treatment of vascularized serous pigment epithelium detachment in AMD—observations after changing the intravitreal agent due to lack of response. Klin Monbl Augenheilkd. 2008;225(10):874–9.
Ruppenstein M, Ach T, Hoh A, Dithmar S. Effect of intravitreal bevacizumab on pigment epithelial detachment in occult choroidal neovascularization. Ophthalmologe. 2010;107(9):827–30.
Lommatzsch A, Heimes B, Gutfleisch M, et al. Serous pigment epithelial detachment in age-related macular degeneration: comparison of different treatments. Eye (Lond). 2009;23(12):2163–8.
Ach T, Hoeh AE, Ruppenstein M, et al. Intravitreal bevacizumab in vascular pigment epithelium detachment as a result of subfoveal occult choroidal neovascularization in age-related macular degeneration. Retina. 2010;30(9):1420–5.
Ritter M, Bolz M, Sacu S, et al. Effect of intravitreal ranibizumab in avascular pigment epithelial detachment. Eye (Lond). 2010;24(6):962–8.
Arias L. Treatment of retinal pigment epithelial detachment with antiangiogenic therapy. Clin Ophthalmol. 2010;4:369–74.
Ladas ID, Kotsolis AI, Papakostas TD, et al. Intravitreal bevacizumab combined with photodynamic therapy for the treatment of occult choroidal neovascularization associated with serous pigment epithelium detachment in age-related macular degeneration. Retina. 2007;27(7):891–6.
Shima C, Gomi F, Sawa M, et al. One-year results of combined photodynamic therapy and intravitreal bevacizumab injection for retinal pigment epithelial detachment secondary to age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2009;247(7):899–906.
el Matri L, Chebil A, Kort F, et al. Intravitreal injection of triamcinolone combined with bevacizumab for choroidal neovascularization associated with large retinal pigment epithelial detachment in age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2010;248(6):779–84.
Hajouli N, Hirsh A, Quintyn JC. Triple therapy for the treatment of choroidal neovascularization with pigment epithelium detachment in age-related macular degeneration. J Fr Ophtalmol. 2010;33(7):487–92.
Frimpong-Boateng A, Varde MA, Rufer F, et al. Intravitreal administration of triamcinolone and bevacizumab for pigment epithelial detachment in conjunction with AMD. Ophthalmologe. 2008;105(7):661–8.
Subramanyam A, Phatak S, Chudgar D. Large retinal pigment epithelium rip following serial intravitreal injection of avastin in a large fibrovascular pigment epithelial detachment. Indian J Ophthalmol. 2007;55(6):483–6.
Chan CK, Lin SG. Retinal pigment epithelial tear after ranibizumab therapy for subfoveal fibrovascular pigment epithelial detachment. Eur J Ophthalmol. 2007;17(4):674–6.
Chen E, Kaiser RS, Vander JF. Intravitreal bevacizumab for refractory pigment epithelial detachment with occult choroidal neovascularization in age-related macular degeneration. Retina. 2007;27(4):445–50.
Chan CK, Abraham P, Meyer CH, et al. Optical coherence tomography-measured pigment epithelial detachment height as a predictor for retinal pigment epithelial tears associated with intravitreal bevacizumab injections. Retina. 2009;30(2):203–11.
Casswell AG, Kohen D, Bird AC. Retinal pigment epithelial detachments in the elderly: classification and outcome. Br J Ophthalmol. 1985;69(6):397–403.
Pauleikhoff D, Loffert D, Spital G, et al. Pigment epithelial detachment in the elderly. Clinical differentiation, natural course and pathogenetic implications. Graefes Arch Clin Exp Ophthalmol. 2002;240(7):533–8.
Schuman JS, Fujimoto JG, Puliafito CA. Optical coherence tomography of ocular diseases. Slack Incorporated; 2004/5.
Eter N, Bindewald A, Roth F, Holz FG. OCT in age-related macular degeneration. Findings, usage in clinical routine, and assessment of treatment outcome. Ophthalmologe. 2004;101(8):794–803.
Bressler NM, Bressler SB, Fine SL. Age-related macular degeneration. Surv Ophthalmol. 1988;32(6):375–413.
Gass JDM. Stereoscopic atlas of macular disease: diagnosis and management. St. Louis:Mosby; 1997.
Gass JD. Retinal pigment epithelial rip during krypton red laser photocoagulation. Am J Ophthalmol. 1984;98(6):700–6.
Barbazetto I, Burdan A, Bressler NM, et al. Photodynamic therapy of subfoveal choroidal neovascularization with verteporfin: fluorescein angiographic guidelines for evaluation and treatment–TAP and VIP report No. 2. Arch Ophthalmol. 2003;121(9):1253–68.
Schaal KB, Engler C, Schutt F, et al. Intravitreal anti-VEGF therapy with bevacizumab for neovascular AMD. Ophthalmologe. 2008;105(6):538–43.
Kaiser PK, Blodi BA, Shapiro H, Acharya NR. Angiographic and optical coherence tomographic results of the MARINA study of ranibizumab in neovascular age-related macular degeneration. Ophthalmology. 2007;114(10):1868–75.
Rosenfeld PJ, Rich RM, Lalwani GA. Ranibizumab: phase III clinical trial results. Ophthalmol Clin North Am. 2006;19(3):361–72.
Lazic R, Gabric N. Intravitreally administered bevacizumab (Avastin) in minimally classic and occult choroidal neovascularization secondary to age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2007;245(1):68–73.
Brown DM, Regillo CD. Anti-VEGF agents in the treatment of neovascular age-related macular degeneration: applying clinical trial results to the treatment of everyday patients. Am J Ophthalmol. 2007;144(4):627–37.
Cohen SY, Korobelnik JF, Tadayoni R, et al. [Monitoring anti-VEGF drugs for treatment of exudative AMD]. J Fr Ophtalmol. 2007;30(4):330–4.
Helb HM, Issa PC, Fleckenstein M, et al. Clinical evaluation of simultaneous confocal scanning laser ophthalmoscopy imaging combined with high-resolution, spectral-domain optical coherence tomography. Acta Ophthalmol. 2010;88(8):842–9.
Meyer CH, Helb HM, Eter N. [Monitoring of AMD patients on anti-vascular endothelial growth factor (VEGF) treatment. Practical notes on functional and anatomical examination parameters from drug approval studies, specialist information and case series]. Ophthalmologe. 2008;105(2):125–38,140–22.
Avery RL, Pieramici DJ, Rabena MD, et al. Intravitreal bevacizumab (Avastin) for neovascular age-related macular degeneration. Ophthalmology. 2006;113(3):363–72.e365.
Smretschnig E, Krebs I, Moussa S, et al. Cirrus OCT versus Spectralis OCT: differences in segmentation in fibrovascular pigment epithelial detachment. Graefes Arch Clin Exp Ophthalmol. 2010;248(12):1693–8.
Mylonas G, Ahlers C, Malamos P, et al. Comparison of retinal thickness measurements and segmentation performance of four different spectral and time domain OCT devices in neovascular age-related macular degeneration. Br J Ophthalmol. 2009;93(11):1453–60.
Levy J, Shneck M, Rosen S, et al. Intravitreal bevacizumab (avastin) for subfoveal neovascular age-related macular degeneration. Int Ophthalmol. 2009;29(5):349–57.
Melamud A, Stinnett S, Fekrat S. Treatment of neovascular age-related macular degeneration with intravitreal bevacizumab: efficacy of three consecutive monthly injections. Am J Ophthalmol. 2008;146(1):91–5.
Emerson MV, Lauer AK, Flaxel CJ, et al. Intravitreal bevacizumab (Avastin) treatment of neovascular age-related macular degeneration. Retina. 2007;27(4):439–44.
Keane PA, Liakopoulos S, Ongchin SC, et al. Quantitative subanalysis of optical coherence tomography after treatment with ranibizumab for neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci. 2008;49(7):3115–20.
Moutray T, Alarbi M, Mahon G, et al. Relationships between clinical measures of visual function, fluorescein angiographic and optical coherence tomography features in patients with subfoveal choroidal neovascularization. Br J Ophthalmol. 2008;92(3):361–4.
Ting TD, M Oh, Cox TA, et al. Decreased visual acuity associated with cystoid macular edema in neovascular age-related macular degeneration. Arch Ophthalmol. 2002;120(6):731–7.
Eter N, Spaide RF. Comparison of fluorescein angiography and optical coherence tomography for patients with choroidal neovascularization after photodynamic therapy. Retina. 2005;25(6):691–6.
Brown DM, Kaiser PK, Michels M, et al. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med. 355(14):1432–44.
Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1419–31.
Meyer CH, Mennel S, Schmidt JC, Kroll P. Acute retinal pigment epithelial tear following intravitreal bevacizumab (Avastin) injection for occult choroidal neovascularization secondary to age related macular degeneration. Br J Ophthalmol. 2006;90(9):1207–8.
Pece A, Introini U, Bottoni F, Brancato R. Acute retinal pigment epithelial tear after photodynamic therapy. Retina. 2001;21(6):661–5.
Michels S, Aue A, Simader C, et al. Retinal pigment epithelium tears following verteporfin therapy combined with intravitreal triamcinolone. Am J Ophthalmol. 2006;141(2):396–8.
Yeo JH, Marcus S, Murphy RP. Retinal pigment epithelial tears. Patterns and prognosis. Ophthalmology. 1988;95(1):8–13.
Dhalla MS, Blinder KJ, Tewari A, et al. Retinal pigment epithelial tear following intravitreal pegaptanib sodium. Am J Ophthalmol. 2006;141(4):752–4.
Rosenfeld PJ, Heier JS, Hantsbarger G, Shams N. Tolerability and efficacy of multiple escalating doses of ranibizumab (Lucentis) for neovascular age-related macular degeneration. Ophthalmology. 2006;113(4):623.e1.
Hoskin A, Bird AC, Sehmi K. Tears of detached retinal pigment epithelium. Br J Ophthalmol. 1981;65(6):417–22.
Ronan SM, Yoganathan P, Chien FY, et al. Retinal pigment epithelium tears after intravitreal injection of bevacizumab (avastin) for neovascular age-related macular degeneration. Retina. 2007;27(5):535–40.
Weinberger AW, Thiel M, Mohammadi B, et al. Retinal pigment epithelium tears after intravitreal bevacizumab in pigment epithelium detachment. Am J Ophthalmol. 2007;144(2):294–6.
Kook D, Wolf A, Neubauer AS, et al. Retinal pigment epithelial tears after intravitreal injection of bevacizumab for AMD. Frequency and progress. Ophthalmologe. 2008;105(2):158–64.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hamelmann, V., Helb, HM., Meyer, C. et al. Intravitreal bevacizumab for pigment epithelial detachments in age-related macular degeneration. Spektrum Augenheilkd. 27, 184–195 (2013). https://doi.org/10.1007/s00717-013-0177-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00717-013-0177-2
Keywords
- Age-related macular degeneration
- AMD
- Avastin
- Bevacizumab
- Fluorescein angiography
- OCT
- Optical coherence tomography
- PED
- Pigment epithelial detachment