Abstract
Background
Speech disorders and freezing of gait (FOG) in Parkinson's disease (PD) may have some common pathological mechanisms. The purpose of this study was to compare the acoustic parameters of PD patients with dopamine-responsive FOG (PD-FOG) and without FOG (PD-nFOG) during "ON state" and explore the ability of "ON state" voice features in distinguishing PD-FOG from PD-nFOG.
Methods
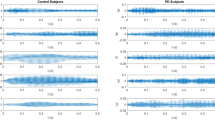
A total of 120 subjects, including 40 PD patients with dopamine-responsive FOG, 40 PD-nFOG, and 40 healthy controls (HCs) were recruited. All subjects underwent neuropsychological tests. Speech samples were recorded through the sustained vowel pronunciation tasks during the "ON state" and then analyzed by the Praat software. A set of 27 voice features was extracted from each sample for comparison. Support vector machine (SVM) was used to build mathematical models to classify PD-FOG and PD-nFOG.
Results
Compared with PD-nFOG, the jitter, the standard deviation of fundamental frequency (F0SD), the standard deviation of pulse period (pulse period SD) and the noise-homophonic-ratio (NHR) were increased, and the maximum phonation time (MPT) was decreased in PD-FOG. The above voice features were correlated with the freezing of gait questionnaire (FOGQ). The average accuracy, specificity, and sensitivity of SVM models based on 27 voice features for classifying PD-FOG and PD-nFOG were 73.57%, 75.71%, and 71.43%, respectively.
Conclusions
PD-FOG have more severe voice impairment than PD-nFOG during "ON state".


Similar content being viewed by others
References
Ali L, Zhu C, Zhang Z, Liu Y (2019) Automated detection of Parkinson’s disease based on multiple types of sustained phonations using linear discriminant analysis and genetically optimized neural network. IEEE J Transl Eng Health Med 7:2000410. https://doi.org/10.1109/jtehm.2019.2940900
Amboni M, Stocchi F, Abbruzzese G, Morgante L, Onofrj M, Ruggieri S, Tinazzi M, Zappia M, Attar M, Colombo D, Simoni L, Ori A, Barone P, Antonini A (2015) Prevalence and associated features of self-reported freezing of gait in Parkinson disease: the DEEP FOG study. Parkinsonism Relat Disord 21(6):644–649. https://doi.org/10.1016/j.parkreldis.2015.03.028
Bartels AL, Balash Y, Gurevich T, Schaafsma JD, Hausdorff JM, Giladi N (2003) Relationship between freezing of gait (FOG) and other features of Parkinson’s: FOG is not correlated with bradykinesia. J Clin Neurosci 10(5):584–588. https://doi.org/10.1016/s0967-5868(03)00192-9
Berg L (1984) Clinical dementia rating. Br J Psychiatry 145:339
Boersma P, D. W (2017) Praat: doing phonetics by computer.https://www.fon.hum.uva.nl/praat/
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatry Res 12(3):189–198. https://doi.org/10.1016/0022-3956(75)90026-6
Galaz Z, Mekyska J, Zvoncak V, Mucha J, Kiska T, Smekal Z, Eliasova I, Mrackova M, Kostalova M, Rektorova I, Faundez-Zanuy M, Alonso-Hernandez J, Gomez-Vilda P (2018) Changes in phonation and their relations with progress of Parkinson’s Disease. Appl Sci. https://doi.org/10.3390/app8122339
Gao C, Liu J, Tan Y, Chen S (2020) Freezing of gait in Parkinson’s disease: pathophysiology, risk factors and treatments. Transl Neurodegener 9:12. https://doi.org/10.1186/s40035-020-00191-5
Giladi N, Shabtai H, Simon ES, Biran S, Tal J, Korczyn AD (2000) Construction of freezing of gait questionnaire for patients with Parkinsonism. Parkinsonism Relat Disord 6(3):165–170. https://doi.org/10.1016/s1353-8020(99)00062-0
Giladi N, McDermott MP, Fahn S, Przedborski S, Jankovic J, Stern M, Tanner C (2001) Freezing of gait in PD: prospective assessment in the DATATOP cohort. Neurology 56(12):1712–1721. https://doi.org/10.1212/wnl.56.12.1712
Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, Poewe W, Sampaio C, Stern MB, Dodel R, Dubois B, Holloway R, Jankovic J, Kulisevsky J, Lang AE, Lees A, Leurgans S, LeWitt PA, Nyenhuis D, Olanow CW, Rascol O, Schrag A, Teresi JA, van Hilten JJ, LaPelle N (2008) Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord 23(15):2129–2170. https://doi.org/10.1002/mds.22340
Hamilton M (1959) The assessment of anxiety states by rating. Br J Med Psychol 32(1):50–55. https://doi.org/10.1111/j.2044-8341.1959.tb00467.x
Hamilton M (1967) Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol 6(4):278–296. https://doi.org/10.1111/j.2044-8260.1967.tb00530.x
Hemmerling D, Wojcik-Pedziwiatr M (2020) Prediction and estimation of Parkinson’s disease severity based on voice signal. J Voice. https://doi.org/10.1016/j.jvoice.2020.06.004
Ho AK, Iansek R, Marigliani C, Bradshaw JL, Gates S (1999) Speech impairment in a large sample of patients with Parkinson’s disease. Behav Neurol 11(3):131–137
Hoehn MM, Yahr MD (1967) Parkinsonism: onset, progression and mortality. Neurology 17(5):427–442
Lam PK, Chan KM, Ho WK, Kwong E, Yiu EM, Wei WI (2006) Cross-cultural adaptation and validation of the Chinese Voice Handicap Index-10. Laryngoscope 116(7):1192–1198. https://doi.org/10.1097/01.mlg.0000224539.41003.93
Li YM, Zhang SJ, Zeng XP (2009) Research of multi-population agent genetic algorithm for feature selection. Expert Syst Appl 36(9):11570–11581. https://doi.org/10.1016/j.eswa.2009.03.032
Lord SR, Bindels H, Ketheeswaran M, Brodie MA, Lawrence AD, Close JCT, Whone AL, Ben-Shlomo Y, Henderson EJ (2020) Freezing of gait in people with Parkinson’s disease: nature, occurrence, and risk factors. J Parkinsons Dis 10(2):631–640. https://doi.org/10.3233/JPD-191813
Ma A, Lau KK, Thyagarajan D (2020) Voice changes in Parkinson’s disease: what are they telling us? J Clin Neurosci 72:1–7. https://doi.org/10.1016/j.jocn.2019.12.029
Martens KAE, Shine JM, Walton CC, Georgiades MJ, Gilat M, Hall JM, Muller AJ, Szeto JYY, Lewis SJG (2018) Evidence for subtypes of freezing of gait in Parkinson’s disease. Mov Disord 33(7):1174–1178. https://doi.org/10.1002/mds.27417
Mekyska J, Galaz Z, Kiska T, Zvoncak V, Mucha J, Smekal Z, Eliasova I, Kostalova M, Mrackova M, Fiedorova D, Faundez-Zanuy M, Sole-Casals J, Gomez-Vilda P, Rektorova I (2018) Quantitative analysis of relationship between hypokinetic dysarthria and the freezing of gait in Parkinson’s disease. Cognit Comput 10(6):1006–1018. https://doi.org/10.1007/s12559-018-9575-8
Midi I, Dogan M, Koseoglu M, Can G, Sehitoglu MA, Gunal DI (2008) Voice abnormalities and their relation with motor dysfunction in Parkinson’s disease. Acta Neurol Scand 117(1):26–34. https://doi.org/10.1111/j.1600-0404.2007.00965.x
Norel R, Agurto C, Heisig S, Rice JJ, Zhang H, Ostrand R, Wacnik PW, Ho BK, Ramos VL, Cecchi GA (2020) Speech-based characterization of dopamine replacement therapy in people with Parkinson’s disease. NPJ Parkinsons Dis 6:12. https://doi.org/10.1038/s41531-020-0113-5
Nutt JG, Bloem BR, Giladi N, Hallett M, Horak FB, Nieuwboer A (2011) Freezing of gait: moving forward on a mysterious clinical phenomenon. Lancet Neurol 10(8):734–744. https://doi.org/10.1016/s1474-4422(11)70143-0
Park HK, Yoo JY, Kwon M, Lee J-H, Lee SJ, Kim SR, Kim MJ, Lee MC, Lee SM, Chung SJ (2014) Gait freezing and speech disturbance in Parkinson’s disease. Neurol Sci 35(3):357–363. https://doi.org/10.1007/s10072-013-1519-1
Podsiadlo D, Richardson S (1991) The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39(2):142–148. https://doi.org/10.1111/j.1532-5415.1991.tb01616.x
Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, Obeso J, Marek K, Litvan I, Lang AE, Halliday G, Goetz CG, Gasser T, Dubois B, Chan P, Bloem BR, Adler CH, Deuschl G (2015) MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 30(12):1591–1601. https://doi.org/10.1002/mds.26424
Ricciardi L, Ebreo M, Graziosi A, Barbuto M, Sorbera C, Morgante L, Morgante F (2016) Speech and gait in Parkinson’s disease: when rhythm matters. Parkinsonism Relat Disord 32:42–47. https://doi.org/10.1016/j.parkreldis.2016.08.013
Rusz J, Tykalova T, Ramig LO, Tripoliti E (2020) Guidelines for speech recording and acoustic analyses in dysarthrias of movement disorders. Mov Disord. https://doi.org/10.1002/mds.28465
Rusz J, Tykalova T, Novotny M, Zogala D, Ruzicka E, Dusek P (2021a) Automated speech analysis in early untreated Parkinson’s disease: relation to gender and dopaminergic transporter imaging. Eur J Neurol. https://doi.org/10.1111/ene.15099
Rusz J, Tykalova T, Novotny M, Zogala D, Sonka K, Ruzicka E, Dusek P (2021b) Defining speech subtypes in De Novo Parkinson disease: response to long-term levodopa therapy. Neurology 97(21):e2124–e2135. https://doi.org/10.1212/WNL.0000000000012878
Sakar BE, Isenkul ME, Sakar CO, Sertbas A, Gurgen F, Delil S, Apaydin H, Kursun O (2013) Collection and analysis of a Parkinson speech dataset with multiple types of sound recordings. IEEE J Biomed Health Inform 17(4):828–834. https://doi.org/10.1109/jbhi.2013.2245674
Skodda S, Visser W, Schlegel U (2010) Short- and long-term dopaminergic effects on dysarthria in early Parkinson’s disease. J Neural Transm (vienna) 117(2):197–205. https://doi.org/10.1007/s00702-009-0351-5
Skodda S, Grönheit W, Schlegel U (2012) Impairment of vowel articulation as a possible marker of disease progression in Parkinson’s disease. PLoS ONE 7(2):e32132. https://doi.org/10.1371/journal.pone.0032132
Teixeira JP, Oliveira C, Lopes C (2013) Vocal acoustic analysis – Jitter, Shimmer and HNR Parameters. Procedia Technol 9:1112–1122. https://doi.org/10.1016/j.protcy.2013.12.124
Tykalova T, Rusz J, Svihlik J, Bancone S, Spezia A, Pellecchia MT (2020) Speech disorder and vocal tremor in postural instability/gait difficulty and tremor dominant subtypes of Parkinson’s disease. J Neural Transm (vienna) 127(9):1295–1304. https://doi.org/10.1007/s00702-020-02229-4
Acknowledgements
We would like to thank all the PD patients and healthy controls who participated in our research.
Funding
This research was supported by the National Natural Science Foundation of China (Nos. 81871002, 81471334, 81100981), the National Key Clinical Specialties Construction Program of China and Joint project of Chongqing Health Commission and Science and Technology Bureau (2021ZY024302).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Data availability
Anonymized data presented in this study will be shared on request to the corresponding author.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Co-first authors: Xiaoya Zou, Fengying Quan, Zhaoying Dong.
Rights and permissions
About this article
Cite this article
Yu, Q., Zou, X., Quan, F. et al. Parkinson's disease patients with freezing of gait have more severe voice impairment than non-freezers during “ON state”. J Neural Transm 129, 277–286 (2022). https://doi.org/10.1007/s00702-021-02458-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-021-02458-1