Abstract
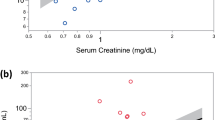
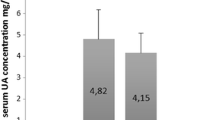
Thirty-three inpatients (22 females, 11 males, aged 79.4 ± 9.5 years) were investigated in this prospective cohort study to study the prevalence of polyneuropathy (PNP) and dementia in geriatric inpatients. Clinical and electrodiagnostic investigations, routine laboratory, including thyroid parameters, folic acid, vitamin B12, homocysteine, neopterin, fibrinogen and glycosylated hemoglobin were measured in serum, the mini-mental state examination and computed tomographic scanning were performed in each patient. PNP was found clinically and electrodiagnostically in 96% of patients. Age was the most precipitating factor for PNP, and was significantly correlated to electrodiagnostic changes in the nerves investigated in both, upper and lower extremities, while clinical symptoms were confined only to the feet. Correlation was seen between homocysteine and the amplitude of the sural nerve (surAmpl) (rs = −0.406, p = 0.029) as well as the sural nerve conduction velocity (surNCV) (rs = −0.389, p = 0.037), and between neopterin and the grade of denervation (rs = 0.445, p = 0.014) in our patients. Neopterin and fibrinogen did not correlate significantly, but there was a trend to higher fibrinogen concentrations in patients with higher neopterin levels (rs = 0.344, p = 0.062). A trend of a correlation was seen between higher homocysteine concentrations and the number of changes in electrodiagnostic measurements (rs = 0.354, p = 0.055). Twenty-one of the 33 patients (64%) were demented, 9 (27%) presented clinically as mild cognitive impairment, 3 (9%) were not demented. Vascular risk factors were found in 83%: hypertension in 58%, hypercholesterinemia in 39%, cardiac disease in 36%, diabetes mellitus (DM) in 21%, peripheral arterial disease (PAD) in 9%. A significant correlation was found between homocysteine and folic acid concentrations (rs = −0.401, p = 0.028). Falls were reported in 48% of cases, indicating PNP as a risk factor in this group of patients. In conclusion, PNP was found very common with a high coincidence with dementia and a female preponderance, suggesting an influence on daily life (falls) in our subjects studied. PNP correlated significantly with markers for vascular disease as well as immune activation (homocysteine and neopterin) similar to earlier findings in patients with neurodegenerative disorders, suggesting common therapeutic options in patients with PNP and dementia.


Similar content being viewed by others
References
Bisschops RH, van der Graaf Y, Mali WP et al (2004) Elevated levels of plasma homocysteine are associated with neurotoxicity. Atherosclerosis 174:87–92
Colbert LH, Visser M, Simonsick EM et al (2004) Physical activity, exercise, and inflammatory markers in older adults: finding from the health, aging and body composition study. J Am Geriatr Soc 52:1098–1104
Fratiglioni L, De Rochi D, Aguero-Torres H (1999) Worldwide prevalence and incidence of dementia. Drugs Aging 15:365–375
Grahmann F, Winterholler M, Neundörfer B (1991) Cryptogenic polyneuropathies: an outpatient follow up study. Acta Neurol Scand 84:221–225
Ha H, Lee JH, Kim HM et al (2006) Alpha lipoic acid inhibits bone resorption by suppressing prostaglandin E2 synthesis. J Immunol 176:111–117
Hattori N, Misu K, Koike H et al (2001) Age of onset influences clinical features of chronic inflammatory demyelinating polyneuropathy. J Neurol Sci 184:57–63
Leblhuber F, Reisecker F, Boem-Jurkovic H et al (1988) Diagnostic value of different electrophysiological tests in cervical disc prolapse. Neurology 38:1879–1881
Leblhuber F, Reisecker F, Willeit J et al (1991) Clinical and electrophysiological findings, nerve biopsy and blood group markers in a family with hereditary neuropathy with liability to pressure palsies. Acta Neurol Scand 83:166–171
Leblhuber F, Walli J, Demel U et al (1999) Increased serum neopterin concentrations in patients with Alzheimer’s disease. Clin Chem Lab Med 37:429–431
Leblhuber F, Walli J, Artner-Dvorzak E et al (2000) Hyperhomocysteinemia in dementia. J Neural Transm 107:1469–1474
Licastro F, Pedrini S, Capuron L et al (2000) Increased plasma levels of interleukin-1, interleukin-6, and alpha-1-antichymotrypsin in patients with Alzheimer’s disease: peripheral inflammation or signals from the brain? J Neuroimmunol 103:97–102
Lipton SA, Kim WK, Choi YB et al (1997) Neurotoxicity associated with dual actions of homocysteine at the N-methyl-d-aspartase receptor. Proc Natl Acad Sci USA 94:5923–5928
Lüdemann P, Dzewas R, Sösös P et al (2001) Axonal polyneuropathy in obstructive sleep apnoea. J Neurol Neurosurg Psychiatry 70:685–687
Ludin HP (1980) Electromyography in practice. Stuttgart, Thieme
Malik RA (2003) Current and future strategies for the management of diabetic neuropathy. Treat Endocrinol 2:398–400
Mc Leod JG, Tuck RR, Pollard JD et al (1984) Chronic polyneuropathy of undetermined cause. J Neurol Neurosurg Psychiatry 47:222–226
Moreland JD, Richardson JA, Goldsmith CH et al (2004) Muscle weakness and falls in older adults: a systemic review and meta-analysis. J Am Geriatr Soc 52:1121–1129
Schröcksnadel K, Leblhuber F, Frick B et al (2004) Association of hyperhomocysteinemia in Alzheimer disease with elevated neopterin levels. Alzheimer Dis Assoc Disord 18:129–133
Teunissen LL, Franssen H, Wocke JHJ et al (2002) Is vascular disease a risk factor in the development of axonal polyneuropathy? J Neurol Neurosurg Psychiatry 72:590–595
The Memantine Study Group (2005) Memantine in the treatment of diabetics with peripheral neuropathy: a placebo controlled phase IIb trial. Physiol Res 54:87–95
Verghese J, Bieri PL, Gellido C et al (2001) Peripheral neuropathy in young-old and old-old patients. Muscle Nerve 24:1476–1481
Verghese J, Lipton RB, Hall CB et al (2002) Abnormality of gait as a predictor of non Alzheimer’s dementia. N Engl J Med 347:1761–1768
Vranken AFJE, Fransen H, Wokke JH et al (2002) Chronic idiopathic axonal polyneuropathy and successful aging of the peripheral nervous system in elderly people. Arch Neurol 59(4):533–540
Weiss N (2005) Mechanisms of increased vascular oxidant stress in hyperhomocysteinemia and its impact on endothelial function. Curr Drug Metab 6:27–36
Wilson CJ, Finch CE, Cohen HJ (2002) Cytokines and cognition—the case for a head to toe inflammatory paradigm. J Am Geriatr Soc 50:2041–2056
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leblhuber, F., Schroecksnadel, K., Beran-Praher, M. et al. Polyneuropathy and dementia in old age: common inflammatory and vascular parameters. J Neural Transm 118, 721–725 (2011). https://doi.org/10.1007/s00702-011-0579-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-011-0579-8