Abstract
Background
To investigate the incidence and risk factors of coronal vertical vertebral body fracture (CV-VBF) during lateral lumbar interbody fusion (LLIF) for degenerative lumbar disease.
Methods
Clinical data, including age, sex, body mass index, and bone mineral density, were reviewed. Radiological assessments, such as facet joint arthrosis, intervertebral disc motion, index disc height, and cage profiles, were conducted. Posterior instrumentation was performed using either a single or staged procedure after LLIF. Demographic and surgical data were compared between patients with and without VBF.
Results
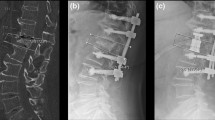
Out of 273 patients (552 levels), 7 (2.6%) experienced CV-VBF. Among the 552 levels, VBF occured in 7 levels (1.3%). All VBF cases developed intraoperatively during LLIF, with no instances caused by cage subsidence during the follow-up period. Sagittal motion in segments adjacent to VBF was smaller than in others (4.6° ± 2.6° versus 6.5° ± 3.9°, P = 0.031). The average grade of facet arthrosis was 2.5 ± 0.7, indicating severe facet arthrosis. All fractures developed due to oblique placement of a trial or cage into the index disc space, leading to a nutcracker effect. These factors were not related to bone quality.
Conclusions
CV-VBF after LLIF occurred in 2.6% of patients, accounting for 1.3% of all LLIF levels. A potential risk factor for VBF involves the nutcracker-impinging effect due to the oblique placement of a cage. Thorough preoperative evaluations and surgical procedures are needed to avoid VBF when considering LLIF in patients with less mobile spine.



Similar content being viewed by others
Data availability
The corresponding author is having the available data.
Code availability
Not applicable.
References
Abe K, Orita S, Mannoji C, Motegi H, Aramomi M, Ishikawa T, Kotani T, Akazawa T, Morinaga T, Fujiyoshi T, Hasue F, Yamagata M, Hashimoto M, Yamauchi T, Eguchi Y, Suzuki M, Hanaoka E, Inage K, Sato J, Fujimoto K, Shiga Y, Kanamoto H, Yamauchi K, Nakamura J, Suzuki T, Hynes RA, Aoki Y, Takahashi K, Ohtori S (2017) Perioperative Complications in 155 Patients Who Underwent Oblique Lateral Interbody Fusion Surgery: Perspectives and Indications From a Retrospective, Multicenter Survey. Spine 42:55–62 (Phila Pa 1976)
Ahmadian A, Verma S, Mundis GM Jr, Oskouian RJ Jr, Smith DA, Uribe JS (2013) Minimally invasive lateral retroperitoneal transpsoas interbody fusion for L4–5 spondylolisthesis: clinical outcomes. J Neurosurg Spine 19:314–320
Belkoff SM, Maroney M, Fenton DC, Mathis JM (1999) An in vitro biomechanical evaluation of bone cements used in percutaneous vertebroplasty. Bone 25:23s–26s
Brier-Jones JE, Palmer DK, Ĭnceoğlu S, Cheng WK (2011) Vertebral body fractures after transpsoas interbody fusion procedures. Spine J 11:1068–1072
Chang SY, Kang DH, Cho SK (2023) Innovative developments in lumbar interbody cage materials and design: A comprehensive narrative review. Asian Spine J. https://doi.org/10.31616/asj.2023.0407
Cummock MD, Vanni S, Levi AD, Yu Y, Wang MY (2011) An analysis of postoperative thigh symptoms after minimally invasive transpsoas lumbar interbody fusion. J Neurosurg Spine 15:11–18
Dua K, Kepler CK, Huang RC, Marchenko A (2010) Vertebral body fracture after anterolateral instrumentation and interbody fusion in two osteoporotic patients. Spine J 10:e11-15
Flamme CH, von der Heide N, Heymann C, Hurschler C (2006) Primary stability of anterior lumbar stabilization: interdependence of implant type and endplate retention or removal. Eur Spine J 15:807–818
Grimm BD, Leas DP, Poletti SC, Johnson DR 2nd (2016) Postoperative Complications Within the First Year After Extreme Lateral Interbody Fusion: Experience of the First 108 Patients. Clin Spine Surg 29:E151-156
Hou Y, Luo Z (2009) A study on the structural properties of the lumbar endplate: histological structure, the effect of bone density, and spinal level. Spine 34:E427-433 (Phila Pa 1976)
Kim WJ, Lee JW, Park KY, Chang SH, Song DG, Choy WS (2019) Treatment of Adult Spinal Deformity with Sagittal Imbalance Using Oblique Lumbar Interbody Fusion: Can We Predict How Much Lordosis Correction Is Possible? Asian Spine J 13:1017–1027
Kim YH, Ha KY, Kim KT, Chang DG, Park HY, Yoon EJ, Kim SI (2021) Risk factors for intraoperative endplate injury during minimally-invasive lateral lumbar interbody fusion. Sci Rep 11:20149
Kim YH, Ha KY, Kim YS, Kim KW, Rhyu KW, Park JB, Shin JH, Kim YY, Lee JS, Park HY, Ko J, Kim SI (2022) Lumbar Interbody Fusion and Osteobiologics for Lumbar Fusion. Asian Spine J 16:1022–1033
Kim YH, Ha KY, Rhyu KW, Park HY, Cho CH, Kim HC, Lee HJ, Kim SI (2020) Lumbar Interbody Fusion: Techniques, Pearls and Pitfalls. Asian Spine J 14:730–741
Le TV, Smith DA, Greenberg MS, Dakwar E, Baaj AA, Uribe JS (2012) Complications of lateral plating in the minimally invasive lateral transpsoas approach. J Neurosurg Spine 16:302–307
Oxland TR, Grant JP, Dvorak MF, Fisher CG (2003) Effects of endplate removal on the structural properties of the lower lumbar vertebral bodies. Spine 28:771–777 (Phila Pa 1976)
Park HY, Ha KY, Kim YH, Chang DG, Kim SI, Lee JW, Ahn JH, Kim JB (2018) Minimally Invasive Lateral Lumbar Interbody Fusion for Adult Spinal Deformity: Clinical and Radiological Efficacy With Minimum Two Years Follow-up. Spine 43:E813-e821 (Phila Pa 1976)
Park HY, Kim YH, Ha KY, Kim SI, Min HK, Oh IS, Seo JY, Chang DG, Park JT (2019) Minimally Invasive Lateral Lumbar Interbody Fusion for Clinical Adjacent Segment Pathology: A Comparative Study With Conventional Posterior Lumbar Interbody Fusion. Clin Spine Surg 32:E426-e433
Park J, Ham DW, Kwon BT, Park SM, Kim HJ, Yeom JS (2020) Minimally Invasive Spine Surgery: Techniques, Technologies, and Indications. Asian Spine J 14:694–701
Polikeit A, Ferguson SJ, Nolte LP, Orr TE (2003) The importance of the endplate for interbody cages in the lumbar spine. Eur Spine J 12:556–561
Rodgers WB, Gerber EJ, Patterson J (2011) Intraoperative and early postoperative complications in extreme lateral interbody fusion: an analysis of 600 cases. Spine 36:26–32 (Phila Pa 1976)
Satake K, Kanemura T, Yamaguchi H, Segi N, Ouchida J (2016) Predisposing Factors for Intraoperative Endplate Injury of Extreme Lateral Interbody Fusion. Asian Spine J 10:907–914
Tempel ZJ, Gandhoke GS, Bolinger BD, Okonkwo DO, Kanter AS (2015) Vertebral body fracture following stand-alone lateral lumbar interbody fusion (LLIF): report of two events out of 712 levels. Eur Spine J 24(Suppl 3):409–413
Tender GC (2014) Caudal vertebral body fractures following lateral interbody fusion in nonosteoporotic patients. Ochsner J 14:123–130
Walker CT, Farber SH, Cole TS, Xu DS, Godzik J, Whiting AC, Hartman C, Porter RW, Turner JD, Uribe J (2019) Complications for minimally invasive lateral interbody arthrodesis: a systematic review and meta-analysis comparing prepsoas and transpsoas approaches. J Neurosurg Spine 30:446–460
Weishaupt D, Zanetti M, Boos N, Hodler J (1999) MR imaging and CT in osteoarthritis of the lumbar facet joints. Skeletal Radiol 28:215–219
Zeng ZY, Xu ZW, He DW, Zhao X, Ma WH, Ni WF, Song YX, Zhang JQ, Yu W, Fang XQ, Zhou ZJ, Xu NJ, Huang WJ, Hu ZC, Wu AL, Ji JF, Han JF, Fan SW, Zhao FD, Jin H, Pei F, Fan SY, Sui DX (2018) Complications and Prevention Strategies of Oblique Lateral Interbody Fusion Technique. Orthop Surg 10:98–106
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Kee-Yong Ha: conceptualization, methodology, writing.
Young-Hoon Kim: data curation, supervision.
Yong-Chan Kim: original draft preparation.
Hyung-Youl Park: investigation.
Hyun Bae: validation.
Sang-Il Kim: writing and revision.
Corresponding author
Ethics declarations
Conflicts of interest/Competing interests
Not applicable.
Ethics approval
Approved by IRB of our institute.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ha, KY., Kim, YH., Kim, YC. et al. Coronal vertical fracture of vertebral body following minimally invasive lateral lumbar interbody fusion: risk factor analysis in consecutive case series. Acta Neurochir 166, 143 (2024). https://doi.org/10.1007/s00701-024-06043-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00701-024-06043-9