Abstract
Objective
The effectiveness of revascularization for complex aneurysms is well-established. This study aimed to describe the technical characteristics and clinical efficacy of intracranial-to-intracranial (IC-IC) bypass for the treatment of complex intracranial aneurysms.
Methods
We retrospectively reviewed all patients with aneurysms who underwent a preplanned combination of surgical or endovascular treatment and IC-IC bypass at our institution between January 2006 and September 2023. IC-IC bypass techniques included four strategies: type A (end-to-end reanastomosis), type B (end-to-side reimplantation), type C (in situ side-to-side anastomosis), and type D (IC-IC bypass with a graft vessel).
Results
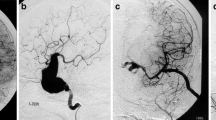
During the study period, ten patients with aneurysms each underwent IC-IC bypass surgery. Aneurysms were located in the middle cerebral artery (60.0%), anterior temporal artery (10.0%), anterior cerebral artery (20.0%), and vertebral artery (10.0%). There were three saccular aneurysms (30.0%), two fusiform aneurysms (20.0%), one dissecting aneurysm (10.0%), and four pseudoaneurysms (40.0%). We performed the type A strategy on five patients (50.0%), type B on one (10.0%), type C on one (10.0%), and type D on three (30.0%).
During a mean period of 68.3 months, good clinical outcomes (modified Rankin Scale score, 0–2) were observed in all patients. Follow-up angiography demonstrated complete aneurysmal obliteration in all patients and good bypass patency in nine of ten patients (90.0%).
Conclusion
The treatment of complex aneurysms remains a challenge with conventional surgical or endovascular treatments. IC-IC bypass surgery is a useful technique, associated with favorable clinical outcomes, for treating complex aneurysms.










Similar content being viewed by others
Data availability
Data and materials are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
References
Amin-Hanjani S, Du X, Mlinarevich N, Meglio G, Zhao M, Charbel FT (2005) The cut flow index: an intraoperative predictor of the success of extracranial-intracranial bypass for occlusive cerebrovascular disease. Neurosurgery 56:75–85. https://doi.org/10.1227/01.neu.0000143032.35416.41. discussion 75-85
Burkhardt JK, Lawton MT (2019) Practice trends in intracranial bypass surgery in a 21-year experience. World Neurosurg 125:e717–e722. https://doi.org/10.1016/j.wneu.2019.01.161
Chandela S, Alzate J, Sen C, Song J, Nimi Y, Berenstein A, Langer D (2008) Treatment of a complex posterior fossa aneurysm in a child using side-to-side posterior inferior cerebellar artery-posterior inferior cerebellar artery bypass. J Neurosurg Pediatr 1:79–82. https://doi.org/10.3171/ped-08/01/079
Chui J, Manninen P, Sacho RH, Venkatraghavan L (2015) Anesthetic management of patients undergoing intracranial bypass procedures. Anesth Analg 120:193–203. https://doi.org/10.1213/ane.0000000000000470
Cikla U, Rowley P, Jennings Simoes EL, Ozaydin B, Goodman SL, Avci E, Baskaya MK, Patel NJ (2020) Grapefruit training model for distal anterior cerebral artery side-to-side bypass. World Neurosurg 138:39–51. https://doi.org/10.1016/j.wneu.2020.02.107
Dunn GP, Gerrard JL, Jho DH, Ogilvy CS (2011) Surgical treatment of a large fusiform distal anterior cerebral artery aneurysm with in situ end-to-side A3–A3 bypass graft and aneurysm trapping: case report and review of the literature. Neurosurgery 68:E587-591. https://doi.org/10.1227/NEU.0b013e3182036012. discussion E591
Gonzalez NR, Duckwiler G, Jahan R, Murayama Y, Viñuela F (2008) Challenges in the endovascular treatment of giant intracranial aneurysms. Neurosurgery 62:1324–1335. https://doi.org/10.1227/01.neu.0000333797.59585.c0
Jahromi BS, Mocco J, Bang JA, Gologorsky Y, Siddiqui AH, Horowitz MB, Hopkins LN, Levy EI (2008) Clinical and angiographic outcome after endovascular management of giant intracranial aneurysms. Neurosurgery 63:662–674. https://doi.org/10.1227/01.neu.0000325497.79690.4c. discussion 674-665
Kalani MY, Ramey W, Albuquerque FC, McDougall CG, Nakaji P, Zabramski JM, Spetzler RF (2014) Revascularization and aneurysm surgery: techniques, indications, and outcomes in the endovascular era. Neurosurgery 74:482–497. https://doi.org/10.1227/neu.0000000000000312. discussion 497-488
Kalani MY, Rangel-Castilla L, Ramey W, Nakaji P, Albuquerque FC, McDougall CG, Spetzler RF, Zabramski JM (2015) Indications and results of direct cerebral revascularization in the modern era. World Neurosurg 83:345–350. https://doi.org/10.1016/j.wneu.2014.10.013
Kim KH, Ha EJ, Cho WS, Kang HS, Kim JE (2019) Side-to-side bypass between bilateral distal anterior cerebral arteries and surgical trapping of a pseudoaneurysm from the anterior communicating artery: lessons learnt. NMC Case Rep J 6:5–9. https://doi.org/10.2176/nmccrj.cr.2018-0142
Kim YR, Lee SH, Bae JW, Choi YH, Ha EJ, Kim KM, Cho WS, Kang HS, Kim JE (2022) Trapping and A4–A4 end-to-side anastomosis for the treatment of a ruptured A3 fusiform aneurysm: potential risk of in-situ bypass. J Cerebrovasc Endovasc Neurosurg. https://doi.org/10.7461/jcen.2022.E2022.01.003
Kimura M, Tanaka A, Matsuno H, Nagata S (1993) Use of STA-MCA anastomosis for clipping of giant middle cerebral artery aneurysm–case report. Neurol Med Chir 33:774–778. https://doi.org/10.2176/nmc.33.774
Kivipelto L, Niemelä M, Meling T, Lehecka M, Lehto H, Hernesniemi J (2014) Bypass surgery for complex middle cerebral artery aneurysms: impact of the exact location in the MCA tree. J Neurosurg 120:398–408. https://doi.org/10.3171/2013.10.jns13738
Labib MA, Gandhi S, Cavallo C, Nisson PL, Mooney MA, Catapano JS, Lang MJ, Chen T, Lawton MT (2020) Anterior cerebral artery bypass for complex aneurysms: advances in intracranial-intracranial bypass techniques. World Neurosurg 141:e42–e54. https://doi.org/10.1016/j.wneu.2020.04.124
Lang MJ, Catapano JS, Paisan GM, Koester SW, Cole TS, Labib MA, Zhou JJ, Fredrickson VL, Frisoli FA, Lawton MT (2020) Reimplantation bypass using one limb of a double-origin posterior inferior cerebellar artery for treatment of a ruptured fusiform aneurysm: case report. Oper Neurosurg (Hagerstown, Md) 19:E314-e319. https://doi.org/10.1093/ons/opaa016
Mura J, Torche E, Riquelme F, Parra M, Julio R (2012) Three-year-old patient with giant MCA aneurysm treated by trapping-resection plus STA-MCA bypass. Case report. Child’s Nerv Syst: ChNS: official journal of the International Society for Pediatric Neurosurgery 28:169–173. https://doi.org/10.1007/s00381-011-1602-y
Ravina K, Rennert RC, Brandel MG, Strickland BA, Chun A, Lee Y, Carey JN, Russin JJ (2021) Comparative assessment of extracranial-to-intracranial and intracranial-to-intracranial in situ bypass for complex intracranial aneurysm treatment based on rupture status: a case series. World Neurosurg 146:e122–e138. https://doi.org/10.1016/j.wneu.2020.10.056
Ryu J, Chung Y, Lee SH, Cho WS, Choi SK (2018) In situ side-to-side anastomosis: surgical technique and complication avoidance. World Neurosurg 110:336–344. https://doi.org/10.1016/j.wneu.2017.11.087
Sanai N, Zador Z, Lawton MT (2009) Bypass surgery for complex brain aneurysms: an assessment of intracranial-intracranial bypass. Neurosurgery 65:670–683. https://doi.org/10.1227/01.neu.0000348557.11968.f1. discussion 683
Sato K, Endo H, Fujimura M, Endo T, Matsumoto Y, Shimizu H, Tominaga T (2018) Endovascular treatments in combination with extracranial-intracranial bypass for complex intracranial aneurysms. World Neurosurg 113:e747–e760. https://doi.org/10.1016/j.wneu.2018.02.143
See AP, Charbel FT (2021) Bypass for flow-augmentation in atherosclerotic carotid occlusion: a review of the literature and career experience. J Neurosurg Sci 65:305–321. https://doi.org/10.23736/s0390-5616.21.05094-3
Straus DC, Brito da Silva H, McGrath L, Levitt MR, Kim LJ, Ghodke BV, Barber JK, Sekhar LN (2017) Cerebral revascularization for aneurysms in the flow-diverter era. Neurosurgery 80:759–768. https://doi.org/10.1093/neuros/nyx064
Sughrue ME, Saloner D, Rayz VL, Lawton MT (2011) Giant intracranial aneurysms: evolution of management in a contemporary surgical series. Neurosurgery 69:1261–1270. https://doi.org/10.1227/NEU.0b013e31822bb8a6. discussion 1270-1261
Wang J, Liu XF, Li BM, Li S, Cao XY, Liang YP, Ge AL, Feng HM (2017) Application of parallel stent placement in the treatment of unruptured vertebrobasilar fusiform aneurysms. J Neurosurg 126:45–51. https://doi.org/10.3171/2015.12.jns151716
Wang L, Cai L, Qian H, Lawton MT, Shi X (2018) The in situ side-to-side bypass technique: a comprehensive review of the technical characteristics, current anastomosis approaches, and surgical experience. World Neurosurg 115:357–372. https://doi.org/10.1016/j.wneu.2018.04.173
Wang L, Cai L, Qian H, Song J, Tanikawa R, Lawton M, Shi X (2019) Intracranial-intracranial bypass with a graft vessel: a comprehensive review of technical characteristics and surgical experience. World Neurosurg 125:285–298. https://doi.org/10.1016/j.wneu.2019.01.259
Yang K, Ahn JS, Park JC, Kwon DH, Kwun BD, Kim CJ (2015) The efficacy of bypass surgery using a short interposition graft for the treatment of intracranial complex aneurysm. World Neurosurg 83:197–202. https://doi.org/10.1016/j.wneu.2014.06.008
Funding
This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: H122C1015).
Author information
Authors and Affiliations
Contributions
Sue-Jee Park: investigation and data curation, writing—original draft preparation, and writing—reviewing and editing. Sung-Pil Joo: conceptualization, writing—reviewing and editing, and supervision. Young-Jun Lee: investigation and data curation. Woong-Beom, Kim: software. You-Sub Kim: software and validation. Tae-Sun Kim: validation and methodology.
Corresponding author
Ethics declarations
Ethics approval
This study was in accordance with the ethical standards of the Institutional Review Board of our hospital.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Comments
A brief summary of the literature on flow-guided surgery would be a suitable accompaniment to this nice description of IC-IC bypass. Quantitative pre-operative flow measurements are important in planning the revascularization strategy and confirming successful intraoperative flow replacement. Although in practice, many surgeons succeed due to patients’ tolerance and adaptability, we have many tools to maximize the success rate of bypass surgery.
Alfred Pokmeng See
Boston, USA
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Park, SJ., Lee, YJ., Kim, WB. et al. Intracranial–intracranial bypass strategies for the treatment of complex intracranial aneurysms: anatomical characteristics and surgical intervention. Acta Neurochir 166, 42 (2024). https://doi.org/10.1007/s00701-024-05945-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00701-024-05945-y