Abstract
Background
Up to 35% of aneurysmal subarachnoid haemorrhage (aSAH) cases may present as poor grade, defined as World Federation of Neurosurgical Societies (WFNS) grades IV and V. In this study, we evaluate functional outcomes and prognostic factors.
Methods
This prospective study included all patients referred to a national, centralized neurosurgical service with a diagnosis of poor-grade aSAH between 01/01/2016 and 31/12/2019. Multivariable logistic regression models were used to estimate probability of poor functional outcomes, defined as a Glasgow Outcome Scale (GOS) of 1–3 at 3 months.
Results
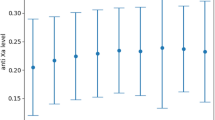
Two hundred fifty-seven patients were referred, of whom 116/257 (45.1%) underwent treatment of an aneurysm, with 97/116 (84%) treated within 48 h of referral. Median age was 62 years (IQR 51–69) with a female predominance (167/257, 65%). Untreated patients tended to be older; 123/141 (87%) had WFNS V, 60/141 (45%) unreactive pupils and 21/141 (16%) circulatory arrest. Of all referred patients, poor outcome occurred in 169/230 (73.5%). Unreactive pupils or circulatory arrest conferred a universally poor prognosis, with mortality in 55/56 (98%) and 19/19 (100%), respectively. The risk of a poor outcome was 14.1% (95% CI 4.5–23.6) higher in WFNS V compared with WFNS IV. Age was important in patients without circulatory arrest or unreactive pupils, with risk of a poor outcome increasing by 1.8% per year (95% CI 1–2.7). In patients undergoing aneurysm securement, 48/101 (47.5%) had a poor outcome, with age, rebleeding, vasospasm and cerebrospinal fluid (CSF) diversion being important prognosticators. The addition of serum markers did not add significant discrimination beyond the clinical presentation.
Conclusions
The overall outcomes of WFNS IV and V aSAH remain poor, mainly due to the devastating effects of the original haemorrhage. However, in patients selected for aneurysm securement, good outcomes can be achieved in more than half of patients. Age, pre-intervention rebleeding, vasospasm, and CSF diversion are important prognostic factors.





Similar content being viewed by others
References
(1988) Report of World Federation of Neurological Surgeons Committee on a universal subarachnoid hemorrhage grading scale. J Neurosurg 68(6):985–986
Alessandro O, Rene W, Stefan W, Miodrag F, Martin S, Oliver B, Urs P (2022) C-reactive protein elevation predicts in-hospital deterioration after aneurysmal subarachnoid hemorrhage: a retrospective observational study. Acta Neurochir (Wien) 164(7):1805–1814
Al-Khindi T, Macdonald RL, Schweizer TA (2010) Cognitive and functional outcome after aneurysmal subarachnoid hemorrhage. Stroke 41(8):e519-536
Al-Mufti F, Mayer SA, Kaur G et al (2021) Neurocritical care management of poor-grade subarachnoid hemorrhage: unjustified nihilism to reasonable optimism. Neuroradiol J 34(6):542–551
Ballarini NM, Chiu Y-D, König F, Posch M, Jaki T (2020) A critical review of graphics for subgroup analyses in clinical trials. Pharm Stat 19(5):541–560
Chen J, Zhu J, He J, Wang Y, Chen L, Zhang C, Zhou J, Yang L (2016) Ultra-early microsurgical treatment within 24 h of SAH improves prognosis of poor-grade aneurysm combined with intracerebral hematoma. Oncol Lett 11(5):3173–3178
Choudhry A, Murray D, Corr P et al (2022) Timing of treatment of aneurysmal subarachnoid haemorrhage: are the goals set in international guidelines achievable? Ir J Med Sci 191(1):401–406
Chu KH, Mahmoud I, Hou X-Y, Winter CD, Jeffree RL, Brown NJ, Brown AF (2018) Incidence and outcome of subarachnoid haemorrhage in the general and emergency department populations in Queensland from 2010 to 2014. Emerg Med Australas 30(4):503–510
Connolly ES, Rabinstein AA, Carhuapoma JR et al (2012) Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke 43(6):1711–1737
Das KK, Singh S, Sharma P, Mehrotra A, Bhaisora K, Sardhara J, Srivastava AK, Jaiswal AK, Behari S, Kumar R (2017) Results of proactive surgical clipping in poor-grade aneurysmal subarachnoid hemorrhage: pattern of recovery and predictors of outcome. World Neurosurg 102:561–570
de Oliveira Manoel AL, Mansur A, Silva GS et al (2016) Functional outcome after poor-grade subarachnoid hemorrhage: a single-center study and systematic literature review. Neurocrit Care 25(3):338–350
de Winkel J, Cras TY, Dammers R, van Doormaal P-J, van der Jagt M, Dippel DWJ, Lingsma HF, Roozenbeek B (2022) Early predictors of functional outcome in poor-grade aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. BMC Neurol 22(1):239
Doherty RJ, Henry J, Brennan D, Javadpour M (2022) Predictive factors for pre-intervention rebleeding in aneurysmal subarachnoid haemorrhage: a systematic review and meta-analysis. Neurosurg Rev 46(1):24
Etminan N, Chang H-S, Hackenberg K, de Rooij NK, Vergouwen MDI, Rinkel GJE, Algra A (2019) Worldwide incidence of aneurysmal subarachnoid hemorrhage according to region, time period, blood pressure, and smoking prevalence in the population: a systematic review and meta-analysis. JAMA Neurol 76(5):588–597
Fisher CM, Kistler JP, Davis JM (1980) Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery 6(1):1–9
Fukuda H, Hayashi K, Moriya T, Nakashita S, Lo BWY, Yamagata S (2015) Intrasylvian hematoma caused by ruptured middle cerebral artery aneurysms predicts recovery from poor-grade subarachnoid hemorrhage. J Neurosurg 123(3):686–692
Gaastra B, Barron P, Newitt L, Chhugani S, Turner C, Kirkpatrick P, MacArthur B, Galea I, Bulters D (2021) CRP (C-reactive protein) in outcome prediction after subarachnoid hemorrhage and the role of machine learning. Stroke 52(10):3276–3285
Goldberg J, Schoeni D, Mordasini P, Z’Graggen W, Gralla J, Raabe A, Beck J, Fung C (2018) Survival and outcome after poor-grade aneurysmal subarachnoid hemorrhage in elderly patients. Stroke 49(12):2883–2889
Goldberg J, Z’Graggen WJ, Hlavica M et al (2023) Quality of life after poor-grade aneurysmal subarachnoid hemorrhage. Neurosurgery. https://doi.org/10.1227/neu.0000000000002332
Gusdon AM, Savarraj JPJ, Shihabeddin E, Paz A, Assing A, Ko S-B, McCullough LD, Choi HA (2021) Time course of peripheral leukocytosis and clinical outcomes after aneurysmal subarachnoid hemorrhage. Front Neurol 12:694996
Han Y, Ye F, Long X, Li A, Xu H, Zou L, Yang Y, You C (2018) Ultra-early treatment for poor-grade aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. World Neurosurg 115:e160–e171
Hanalioglu S, Sahin B, Sayyahmelli S, Ozaydin B, Erginoglu U, Aycan A, Baskaya MK (2022) The role of microsurgery for poor-grade aneurysmal subarachnoid hemorrhages in the endovascular era. Acta Neurochir (Wien) 164(3):781–793
Heinze G, Wallisch C, Dunkler D (2018) Variable selection - A review and recommendations for the practicing statistician. Biom J 60(3):431–449
Hoogmoed J, van den Berg R, Coert BA, Rinkel GJE, Vandertop WP, Verbaan D (2017) A strategy to expeditious invasive treatment improves clinical outcome in comatose patients with aneurysmal subarachnoid haemorrhage. Eur J Neurol 24(1):82–89
Hoogmoed J, Coert BA, van den Berg R, Roos YBWEM, Horn J, Vandertop WP, Verbaan D (2018) Early treatment decisions in poor-grade patients with subarachnoid hemorrhage. World Neurosurg 119:e568–e573
Hoogmoed J, de Oliveira Manoel AL, Coert BA, Marotta TR, Macdonald RL, Vandertop WP, Verbaan D, Germans MR (2019) Why do patients with poor-grade subarachnoid hemorrhage die? World Neurosurg 131:e508–e513
Hutchinson PJ, Power DM, Tripathi P, Kirkpatrick PJ (2000) Outcome from poor grade aneurysmal subarachnoid haemorrhage–which poor grade subarachnoid haemorrhage patients benefit from aneurysm clipping? Br J Neurosurg 14(2):105–109
Inamasu J, Nakae S, Ohmi T et al (2016) The outcomes of early aneurysm repair in world federation of neurosurgical societies grade V subarachnoid haemorrhage patients with emphasis on those presenting with a glasgow coma scale score of 3. J Clin Neurosci 33:142–147
Jennett B, Bond M (1975) Assessment of outcome after severe brain damage. Lancet 1(7905):480–484
Kaneko J, Tagami T, Unemoto K et al (2019) Functional outcome following ultra-early treatment for ruptured aneurysms in patients with poor-grade subarachnoid hemorrhage. J Nippon Med Sch 86(2):81–90
Kassell NF, Drake CG (1982) Timing of aneurysm surgery. Neurosurgery 10(4):514–519
Kassell NF, Torner JC, Haley EC, Jane JA, Adams HP, Kongable GL (1990) The international cooperative study on the timing of aneurysm surgery. Part 1: overall management results. J Neurosurg 73(1):18–36
Korja M, Lehto H, Juvela S, Kaprio J (2016) Incidence of subarachnoid hemorrhage is decreasing together with decreasing smoking rates. Neurology 87(11):1118–1123
Kramer AH, Couillard PL, Kromm JA, Ruddell S, Demers-Marcil S, Mitha AP, Sutherland GR, Wong JH (2021) Findings predictive of poor outcome in grade 5 subarachnoid hemorrhage: a cohort study. Can J Neurol Sci 48(6):807–816
Kranthi S, Sahu BP, Aniruddh P (2016) Factors affecting outcome in poor grade subarachnoid haemorrhage: an institutional study. Asian J Neurosurg 11(4):365–371
Krishnamurthi RV, Barker-Collo S, Parag V, Parmar P, Witt E, Jones A, Mahon S, Anderson CS, Barber PA, Feigin VL (2018) Stroke incidence by major pathological type and ischemic subtypes in the Auckland regional community stroke studies: changes between 2002 and 2011. Stroke 49(1):3–10
Lashkarivand A, Sorteberg W, Rosseland LA, Sorteberg A (2020) Survival and outcome in patients with aneurysmal subarachnoid hemorrhage in Glasgow coma score 3–5. Acta Neurochir (Wien) 162(3):533–544
Le Roux PD, Elliott JP, Newell DW, Grady MS, Winn HR (1996) Predicting outcome in poor-grade patients with subarachnoid hemorrhage: a retrospective review of 159 aggressively managed cases. J Neurosurg 85(1):39–49
Li P, Stuart EA, Allison DB (2015) Multiple imputation: a flexible tool for handling missing data. JAMA 314(18):1966–1967
Li R, Lin F, Chen Y et al (2022) Elevated blood hemoglobin on admission as an independent predictor of unfavorable outcomes in patients with aneurysmal subarachnoid hemorrhage. Neurosurg Rev 45(4):2689–2699
Li R, Zhao Y, Chen X, Hao Q (2022) Predictive values of white blood cell count in peripheral blood at admission on in-hospital complications and 90-day outcomes of patients with aneurysmal subarachnoid hemorrhage: insights from the LongTEAM Registry. J Inflamm Res 15:6481–6494
Lindbohm JV, Kaprio J, Jousilahti P, Salomaa V, Korja M (2017) Risk factors of sudden death from subarachnoid hemorrhage. Stroke 48(9):2399–2404
Mack WJ, Hickman ZL, Ducruet AF et al (2008) Pupillary reactivity upon hospital admission predicts long-term outcome in poor grade aneurysmal subarachnoid hemorrhage patients. Neurocrit Care 8(3):374–379
Mahta A, Azher AI, Moody S et al (2021) Association of Early white blood cell trend with outcomes in aneurysmal subarachnoid hemorrhage. World Neurosurg 151:e803–e809
Newgard CD, Lewis RJ (2015) Missing data: how to best account for what is not known. JAMA 314(9):940–941
Norton EC, Dowd BE, Maciejewski ML (2019) Marginal effects-quantifying the effect of changes in risk factors in logistic regression models. JAMA 321(13):1304–1305
Post R, Germans MR, Tjerkstra MA et al (2021) Ultra-early tranexamic acid after subarachnoid haemorrhage (ULTRA): a randomised controlled trial. Lancet 397(10269):112–118
Raabe A, Beck J, Goldberg J et al (2022) Herniation World Federation of Neurosurgical Societies scale improves prediction of outcome in patients with poor-grade aneurysmal subarachnoid hemorrhage. Stroke 53(7):2346–2351
R Core Team (2022) R: a language and environment for statistical computing
Ridwan S, Kristof R (2019) Cardiac arrest in patients with poor-grade aneurysmal subarachnoid hemorrhage: a single-center experience. J Neurol Surg A Cent Eur Neurosurg 80(6):409–412
Roozenbeek B, Lingsma HF, Perel P, Edwards P, Roberts I, Murray GD, Maas AI, Steyerberg EW, IMPACT (International Mission on Prognosis and Clinical Trial Design in Traumatic Brain Injury) Study Group, CRASH (Corticosteroid Randomisation After Significant Head Injury) Trial Collaborators (2011) The added value of ordinal analysis in clinical trials: an example in traumatic brain injury. Crit Care 15(3):R127
Rordorf G, Ogilvy CS, Gress DR, Crowell RM, Choi IS (1997) Patients in poor neurological condition after subarachnoid hemorrhage: early management and long-term outcome. Acta Neurochir (Wien) 139(12):1143–1151
Said M, Gümüs M, Rodemerk J et al (2022) Systematic review and meta-analysis of outcome-relevant anemia in patients with subarachnoid hemorrhage. Sci Rep 12(1):20738
Schatlo B, Fung C, Stienen MN et al (2021) Incidence and outcome of aneurysmal subarachnoid hemorrhage: the Swiss study on subarachnoid hemorrhage (Swiss SOS). Stroke 52(1):344–347
Sonne A, Bækgaard ES, Banner J, Rasmussen LS (2020) Spontaneous subarachnoid haemorrhage as a cause of out-of-hospital death. J Stroke Cerebrovasc Dis 29(11):105239
Sweeney K, Silver N, Javadpour M (2016) Subarachnoid haemorrhage (spontaneous aneurysmal). BMJ Clin Evid 2016:1213
Tasiou A, Brotis AG, Paschalis T, Tzerefos C, Kapsalaki EZ, Giannis T, Tzannis A, Fountas KN (2022) Intermediate surgical outcome in patients suffering poor-grade aneurysmal subarachnoid hemorrhage. A single center experience. Int J Neurosci 132(1):38–50
Teo M, Guilfoyle MR, Turner C, Kirkpatrick PJ, Collaborators STASH (2017) What factors determine treatment outcome in aneurysmal subarachnoid hemorrhage in the modern era? A post hoc STASH analysis. World Neurosurg 105:270–281
Turner CL, Budohoski K, Smith C, Hutchinson PJ, Kirkpatrick PJ, Murray GD, STASH collaborators, (2015) Elevated baseline C-reactive protein as a predictor of outcome after aneurysmal subarachnoid hemorrhage: data from the simvastatin in aneurysmal subarachnoid hemorrhage (STASH) trial. Neurosurgery 77(5):786–792 (discussion 792-793)
Välimäki V, Luostarinen T, Satopää J, Raj R, Virta JJ (2021) Neurointensive care results and risk factors for unfavorable outcome in aneurysmatic SAH: a comparison of two age groups. Acta Neurochir (Wien) 163(5):1469–1478
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, Initiative STROBE (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370(9596):1453–1457
Wang X, Han C, Xing D, Wang C, Ding X (2019) Early management of poor-grade aneurysmal subarachnoid hemorrhage: a prognostic analysis of 104 patients. Clin Neurol Neurosurg 179:4–8
Weir RU, Marcellus ML, Do HM, Steinberg GK, Marks MP (2003) Aneurysmal subarachnoid hemorrhage in patients with Hunt and Hess grade 4 or 5: treatment using the Guglielmi detachable coil system. AJNR Am J Neuroradiol 24(4):585–590
White P, Gregson B, McColl E, et al (2021) Emergent aneurysm treatment compared with treatment on neurological improvement in patients with ruptured poor-grade aneurysmal subarachnoid haemorrhage: the TOPSAT2 RCT. NIHR J Libr, Southampton (UK)
Whitfield PC, Kirkpatrick PJ (2001) Timing of surgery for aneurysmal subarachnoid haemorrhage. Cochrane Database Syst Rev 2:CD001697
Wolfert C, Maurer CJ, Berlis A, Schneider H, Steininger K, Motov S, Krauss P, Sommer B, Shiban E (2022) Hydrocephalus, cerebral vasospasm, and delayed cerebral ischemia following non-aneurysmatic spontaneous subarachnoid hemorrhages: an underestimated problem. Neurosurg Rev 46(1):23
Wostrack M, Sandow N, Vajkoczy P et al (2013) Subarachnoid haemorrhage WFNS grade V: is maximal treatment worthwhile? Acta Neurochir (Wien) 155(4):579–586
Zhao B, Zhao Y, Tan X, Cao Y, Wu J, Zhong M, Wang S (2015) Factors and outcomes associated with ultra-early surgery for poor-grade aneurysmal subarachnoid haemorrhage: a multicentre retrospective analysis. BMJ Open 5(4):e007410
Zheng K, Zhao B, Tan X-X, Li Z-Q, Xiong Y, Zhong M, Chen S-Y (2018) Comparison of aggressive surgical treatment and palliative treatment in elderly patients with poor-grade intracranial aneurysmal subarachnoid hemorrhage. Biomed Res Int 2018:5818937
Funding
The study was partially funded by Friends of A, a charitable organization.
Author information
Authors and Affiliations
Contributions
Concept and design: JH, MOD, MJ.
Acquisition of data: MOD, DK, PC, DN, DC, JT, AOH, SP, DR.
Interpretation of data: JH, MOD, MJ, JT, AOH, SP, DR.
Statistical analysis: JH.
Drafting of the manuscript: JH, MJ.
Critical revision of the manuscript for important intellectual content: all authors.
Supervision: MJ.
All authors reviewed the manuscript prior to final submission.
Corresponding authors
Ethics declarations
Ethical approval
This study was approved by the local institutional review board (CA248) and performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All participants provided informed consent to all treatment.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Henry, J., Dablouk, M.O., Kapoor, D. et al. Outcomes following poor-grade aneurysmal subarachnoid haemorrhage: a prospective observational study. Acta Neurochir 165, 3651–3664 (2023). https://doi.org/10.1007/s00701-023-05884-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05884-0