Abstract
Purpose
Despite significant advances, the literature on the optimal surgical treatment for spontaneous supratentorial intracerebral haematoma (ICH) remains lacking. Intraoperative ICP measured on closure (closure ICP) was reported to be a potential marker of adequate decompression in various neurosurgical conditions. We hypothesize that closure ICP also correlates with outcomes in ICH.
Methods
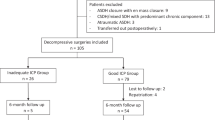
A multicentre retrospective study of 203 decompressive surgeries performed for ICHs was conducted (clot evacuation with either craniectomy or craniotomy). Receiver operating characteristic analysis on closure ICP was performed and an optimal threshold of 5 separated the patients into inadequate (iICP; ICP > 5 mmHg) and good decompression (gICP; ICP ≤ 5 mmHg). Postoperative ICP control, modified Rankin scale (mRS) and mortality were reported.
Results
There were 85 patients in the iICP and 118 patients in the gICP group respectively. The mean age, median preoperative Glasgow coma scale, ICH laterality, location, and volume were similar. After multivariable analysis, the need for (OR 2.55 [1.31–4.97]) and the duration of postoperative hyperosmolar therapy (iICP: 3 days, gICP: 1 day; p = 0.045), and repeat surgery for refractory ICP (OR 5.80 [1.53–22]) were more likely in the iICP group. The likelihood of mRS improvement at 1-year follow up was significantly worse in the iICP group (OR 0.38 [0.17–0.83], p = 0.015).
Conclusion
Closure ICP is an objective and reproducible surgical target. When planning for surgical decompression, obtaining closure ICP of ≤ 5 mmHg is potentially able to improve postoperative ICP management and optimise functional recovery in a well selected patient population.

Similar content being viewed by others
Data Availability
This data is original and available upon request.
References
Davis SM, Broderick J, Hennerici M et al (2006) Haematoma growth is a determinant of mortality and poor outcome after intracerebral hemorrhage. Neurology 66:1175–1181
Dowlatshahi D, Demchuk AM, Flaherty ML et al (2011) Defining hematoma expansion in intracerebral hemorrhage: relationship with patient outcomes. Neurology 76:1238–1244
Feigin VL, Lawes CMM, Bennett DA et al (2003) Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol 2:43–53
Greenberg SM, Ziai WC, Cordonnier C et al (2022) 2002 guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke 53:e282–e361
Gregson BA, Mitchell P, Mendelow AD (2019) Surgical decision making in brain hemorrhage. Stroke 50:1108–1115
Hadjiathanasiou A, Schuss P, Ilic I et al (2018) Decompressive craniectomy for intracerebral haematoma: the influence of additional haematoma evacuation. Neurosurg Rev 41:649–654
Hanley DF, Thompson RE, MMISTIEIII Rosenblum Investigators et al (2019) Efficacy and safety of minimally invasive surgery with thrombolysis in intracerebral haemorrhage evacuation (MISTIE III) a randomised, controlled, open-label, blinded endpoint phase 3 trial. Lancet 393:1021–1032
Hawryluk GWJ, Aguilera S, Buki A et al (2019) A management algorithm for patients with intracranial pressure monitoring: the Seattle international severe traumatic brain injury consensus conference (SIBICC). Intensive Care Med 45:1783–1794
Ironside N, Chen CJ, Ding D et al (2019) Perihematomal edema after spontaneous intracerebral hemorrhage. Stroke 50:1626–1633
Law ZK, Ali A, Krishnan K et al (2020) Noncontrast computed tomography sings as predictors of hematoma expansion, clinical outcome, and response to tranexamic acid in acute intracerebral hemorrhage. Stroke 51:121–128
Leasure AC, Qureshi AI, Murthy SB et al (2019) Intensive blood pressure reduction and perihematomal edema expansion in deep intracerebral hemorrhage. Stroke 50:2016–2022
Li L, Molian VA, Seaman SC et al (2021) Impact of intracerebral hematoma evacuation during decompressive hemicraniectomy on functional outcomes. Stroke 52:1105–1108
Lim JX, Liu JS, Cheong TM et al (2022) Closure intracranial pressure is an objective intraoperative determinant of the adequacy of surgical decompression in traumatic acute subdural haematoma: a multicentre observational study. Acta Neurochir. https://doi.org/10.1007/s00701-022-05270-2
Lim JX, Liu JS, Cheong TM et al (2022) Intracranial pressure as an objective biomarker of decompression adequacy in large territory infarction: a multicenter observational study. Front Surg. https://doi.org/10.3389/fsurg.2022.823899
Mendelow AD, Gregson BA, Rowan EN et al (2013) STITCH II Investigators/ Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STITCH II): a randomised trial. Lancet 382:397–408
Mould WA, Carhuapoma JR, Muschelli J et al (2013) Minimally invasive surgery plus recombinant tissue-type plasminogen activator for intracerebral haemorrhage evacuation decreases perihematomal edema. Stroke 44:627–634
O’Donnell MJ, Xavier D, Liu L et al (2010) Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet 376:112–123
Park J, Lim E, Kim GY et al (2009) External decompressive craniectomy including resection of temporal muscle and fascia in malignant hemispheric infarction. J Neurosurg 110:101–105
Sauvigny T, Gottsche J, Czorlich P, Vettorazzi E, Westphal M, Regelsberger J (2018) Intracranial pressure in patients undergoing decompressive craniectomy: new perspectives on thresholds. J Neurosurg 128:819–827
Shoamanesh A, Lindsay MP, Castellucci LA et al (2021) Int J Stroke 16:321–341
Velanovich V, Antoine H, Swartz A et al (2013) Accumulating deficits model of frailty and postoperative mortality and morbidity: its application to a national database. J Surg Res 183:104–110
Virani SS, Alonso A, Aparicio JH et al (2021) Heart disease and stroke statistics – 2021 update: a report from the American Heart Association. Circulation 143:e254–e743
Wang YF, Wu JS, Mao Y et al (2008) The optimal time-window for surgical treatment of spontaneous intracerebral hemorrhage: result of prospective randomized controlled trial of 500 cases. Acta Neurochir Suppl 105:141–145
Yogendrakumar V, Moores M, Sikora L et al (2020) Evaluating hematoma expansion scores in acute spontaneous intracerebral hemorrhage. Stroke 51:1305–1308
Yogendrakumar V, Ramsay T, Fergusson DA et al (2020) Redefining hematoma expansion with the inclusion of intraventricular hemorrhage growth. Stroke 51:1120–1127
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors did not receive support from any organisation for the submitted work. The authors have no relevant financial or non-financial interests to disclose.
Competing interests
The authors do not report any conflicting interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jia Xu Lim and Nivedh Dinesh are co-first authors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lim, J.X., Dinesh, N., Liu, J.S. et al. Closure intracranial pressure as a determinant of surgical decompression adequacy in spontaneous supratentorial intracerebral haematoma: a multicentre observational study. Acta Neurochir 165, 3805–3813 (2023). https://doi.org/10.1007/s00701-023-05790-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05790-5