Abstract
Background
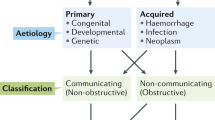
The molecular mechanisms underlying development of posthemorrhagic hydrocephalus (PHH) remain elusive. The aim of this systematic review was to evaluate existing literature on increased CSF secretion and impaired CSF absorption as pathogenic contributors to CSF accumulation in neonatal and adult PHH.
Methods
The systematic review was conducted in accordance with the PRISMA guidelines. Relevant studies published before March 11th, 2023, were identified from PubMed and reference lists. Studies were screened for eligibility using predefined inclusion and exclusion criteria. Data from eligible studies were extracted and potential sources of bias were evaluated.
Results
Nineteen studies quantified CSF production rates and/or CSF absorption capacity in human patients with PHH or animals with experimentally induced PHH. Increased CSF production was reported as early as 24 h and as late as 28 days post ictus in six out of eight studies quantifying CSF production rates in animals with experimentally induced PHH. Impaired CSF absorption was reported in all four studies quantifying CSF absorption capacity in human patients with PHH and in seven out of nine studies quantifying CSF absorption capacity in animals with experimentally induced PHH. Impaired CSF absorption was reported as early as 30 min and as late as 10 months post ictus.
Conclusions
The pathological CSF accumulation in PHH likely arises from a combination of increased CSF secretion and impaired CSF absorption, which may manifest at different time scales following a hemorrhagic event. Emergent evidence on increased CSF secretion by the choroid plexus may herald a paradigm shift in our understanding of PHH.

Similar content being viewed by others
Data availability
Not applicable.
Abbreviations
- aCSF:
-
Artificial cerebrospinal fluid
- Akt:
-
Protein kinase B
- CLIC6:
-
Chloride intracellular channel protein 6
- CNS:
-
Central nervous system
- C out :
-
Conductance to CSF-outflow
- CSF:
-
Cerebrospinal fluid
- FGF-2:
-
Fibroblast growth factor-2
- ICH:
-
Intracerebral hemorrhage
- ICP:
-
Intracranial pressure
- IVH:
-
Intraventricular hemorrhage
- KCNJ13:
-
Potassium inwardly rectifying channel subfamily J member 13
- LPA:
-
Lysophosphatidic acid
- mTOR:
-
Mechanistic target of rapamycin
- NF-kB:
-
Nuclear factor kappa B
- NKCC1:
-
Na+/K+/2Cl– cotransporter 1
- NLRP3:
-
NOD-, LRR-, and pyrin domain-containing protein 3
- PHH:
-
Posthemorrhagic hydrocephalus
- PI3K:
-
Phosphatidylinositol 3-kinase
- R out :
-
Resistance to CSF-outflow
- SAH:
-
Subarachnoid hemorrhage
- SPAK:
-
STE20/SPS1-related proline-alanine-rich kinase
- TGF-β1:
-
Transforming growth factor beta-1
- TLR4:
-
Toll-like receptor 4
- TRPV4:
-
Transient receptor potential vanilloid 4
- WNK:
-
With-no-lysine kinase
References
Aziz AA, Coleman L, Morokoff A, Maixner W (2005) Diffuse choroid plexus hyperplasia: an under-diagnosed cause of hydrocephalus in children? Pediatr Radiol 35:815–818. https://doi.org/10.1007/s00247-005-1456-0
Banizs B, Pike MM, Millican CL, Ferguson WB, Komlosi P, Sheetz J, Bell PD, Schwiebert EM, Yoder BK (2005) Dysfunctional cilia lead to altered ependyma and choroid plexus function, and result in the formation of hydrocephalus. Development 132:5329–5339. https://doi.org/10.1242/dev.02153
Bateman GA, Alber M, Schuhmann MU (2014) An association between external hydrocephalus in infants and reversible collapse of the venous sinuses. Neuropediatrics 45:183–187. https://doi.org/10.1055/s-0033-1363092
Bateman GA, Brown KM (2012) The measurement of CSF flow through the aqueduct in normal and hydrocephalic children: from where does it come, to where does it go? Childs Nerv Syst 28:55–63. https://doi.org/10.1007/s00381-011-1617-4
Bergsneider M, Egnor MR, Johnston M, Kranz D, Madsen JR, McAllister JP 2nd, Stewart C, Walker ML, Williams MA (2006) What we don’t (but should) know about hydrocephalus. J Neurosurg 104:157–159. https://doi.org/10.3171/ped.2006.104.3.157
Bettegowda C, Adogwa O, Mehta V, Chaichana KL, Weingart J, Carson BS, Jallo GI, Ahn ES (2012) Treatment of choroid plexus tumors: a 20-year single institutional experience. J Neurosurg Pediatr 10:398–405. https://doi.org/10.3171/2012.8.Peds12132
Black PM, Tzouras A, Foley L (1985) Cerebrospinal fluid dynamics and hydrocephalus after experimental subarachnoid hemorrhage. Neurosurgery 17:57–62. https://doi.org/10.1227/00006123-198507000-00009
Blasberg R, Johnson D, Fenstermacher J (1981) Absorption resistance of cerebrospinal fluid after subarachnoid hemorrhage in the monkey; effects of heparin. Neurosurgery 9:686–691. https://doi.org/10.1227/00006123-198112000-00012
Brinker T, Seifert V, Dietz H (1992) Subacute hydrocephalus after experimental subarachnoid hemorrhage: its prevention by intrathecal fibrinolysis with recombinant tissue plasminogen activator. Neurosurgery 31:306–311. https://doi.org/10.1227/00006123-199208000-00016
Brinker T, Seifert V, Stolke D (1990) Acute changes in the dynamics of the cerebrospinal fluid system during experimental subarachnoid hemorrhage. Neurosurgery 27:369–372. https://doi.org/10.1097/00006123-199009000-00005
Brinker T, Seifert V, Stolke D (1991) Effect of intrathecal fibrinolysis on cerebrospinal fluid absorption after experimental subarachnoid hemorrhage. J Neurosurg 74:789–793. https://doi.org/10.3171/jns.1991.74.5.0789
Cao Y, Liu C, Li G, Gao W, Tang H, Fan S, Tang X, Zhao L, Wang H, Peng A, You C, Tong A, Zhou L (2022) Metformin alleviates delayed hydrocephalus after intraventricular hemorrhage by inhibiting inflammation and fibrosis. Transl Stroke Res. https://doi.org/10.1007/s12975-022-01026-3
Castaneyra-Ruiz L, Morales DM, McAllister JP, Brody SL, Isaacs AM, Strahle JM, Dahiya SM, Limbrick DD (2018) Blood exposure causes ventricular zone disruption and glial activation in vitro. J Neuropathol Exp Neurol 77:803–813. https://doi.org/10.1093/jnen/nly058
Chaudhry SR, Stoffel-Wagner B, Kinfe TM, Güresir E, Vatter H, Dietrich D, Lamprecht A, Muhammad S (2017) Elevated systemic IL-6 levels in patients with aneurysmal subarachnoid hemorrhage is an unspecific marker for post-SAH complications. Int J Mol Sci 18. https://doi.org/10.3390/ijms18122580
Chen Q, Feng Z, Tan Q, Guo J, Tang J, Tan L, Feng H, Chen Z (2017) Post-hemorrhagic hydrocephalus: recent advances and new therapeutic insights. J Neurol Sci 375:220–230. https://doi.org/10.1016/j.jns.2017.01.072
Chen Q, Tang J, Tan L, Guo J, Tao Y, Li L, Chen Y, Liu X, Zhang JH, Chen Z, Feng H (2015) Intracerebral hematoma contributes to hydrocephalus after intraventricular hemorrhage via aggravating iron accumulation. Stroke 46:2902–2908. https://doi.org/10.1161/strokeaha.115.009713
Chen Q, Zhang J, Guo J, Tang J, Tao Y, Li L, Feng H, Chen Z (2015) Chronic hydrocephalus and perihematomal tissue injury developed in a rat model of intracerebral hemorrhage with ventricular extension. Transl Stroke Res 6:125–132. https://doi.org/10.1007/s12975-014-0367-5
Cherian S, Thoresen M, Silver IA, Whitelaw A, Love S (2004) Transforming growth factor-betas in a rat model of neonatal posthaemorrhagic hydrocephalus. Neuropathol Appl Neurobiol 30:585–600. https://doi.org/10.1111/j.1365-2990.2004.00588.x
Crack PJ, Zhang M, Morganti-Kossmann MC, Morris AJ, Wojciak JM, Fleming JK, Karve I, Wright D, Sashindranath M, Goldshmit Y, Conquest A, Daglas M, Johnston LA, Medcalf RL, Sabbadini RA, Pébay A (2014) Anti-lysophosphatidic acid antibodies improve traumatic brain injury outcomes. J Neuroinflammation 11:37. https://doi.org/10.1186/1742-2094-11-37
Crews L, Wyss-Coray T, Masliah E (2004) Insights into the pathogenesis of hydrocephalus from transgenic and experimental animal models. Brain Pathol 14:312–316. https://doi.org/10.1111/j.1750-3639.2004.tb00070.x
Dandy WE (1919) Experimental hydrocephalus. Ann Surg 70:129–142. https://doi.org/10.1097/00000658-191908000-00001
Denton DA, Blair-West JR, McBurnie M, Weisinger RS, Logan A, Gonzales AM, Baird A (1995) Central action of basic fibroblast growth factor on ingestive behaviour in mice. Physiol Behav 57:747–752. https://doi.org/10.1016/0031-9384(94)00319-x
Dewan MC, Rattani A, Mekary R, Glancz LJ, Yunusa I, Baticulon RE, Fieggen G, Wellons JC, Park KB, Warf BC (2018) Global hydrocephalus epidemiology and incidence: systematic review and meta-analysis. J Neurosurg:1–15. https://doi.org/10.3171/2017.10.Jns17439
Ding Y, Zhang T, Wu G, McBride DW, Xu N, Klebe DW, Zhang Y, Li Q, Tang J, Zhang JH (2019) Astrogliosis inhibition attenuates hydrocephalus by increasing cerebrospinal fluid reabsorption through the glymphatic system after germinal matrix hemorrhage. Exp Neurol 320:113003. https://doi.org/10.1016/j.expneurol.2019.113003
Domínguez-Pinos MD, Páez P, Jiménez AJ, Weil B, Arráez MA, Pérez-Fígares JM, Rodríguez EM (2005) Ependymal denudation and alterations of the subventricular zone occur in human fetuses with a moderate communicating hydrocephalus. J Neuropathol Exp Neurol 64:595–604. https://doi.org/10.1097/01.jnen.0000171648.86718.bb
Dong C, Ming X, Ye Z, Wang P, Wang L, Li Z, Pan B (2018) Icariside II attenuates chronic hydrocephalus in an experimental subarachnoid hemorrhage rat model. J Pharm Pharm Sci, 318 21:–325. https://doi.org/10.18433/jpps29811
Fang Y, Wang X, Lu J, Shi H, Huang L, Shao A, Zhang A, Liu Y, Ren R, Lenahan C, Tang J, Zhang J, Zhang JH, Chen S (2022) Inhibition of caspase-1-mediated inflammasome activation reduced blood coagulation in cerebrospinal fluid after subarachnoid haemorrhage. EBioMedicine 76:103843. https://doi.org/10.1016/j.ebiom.2022.103843
Fejes Z, Pócsi M, Takai J, Erdei J, Tóth A, Balogh E, Rusznyák Á, Fenyvesi F, Nagy A, Kappelmayer J, Jeney V, Nagy B Jr (2021) Preterm intraventricular hemorrhage-induced inflammatory response in human choroid plexus epithelial cells. Int J Mol Sci 22:–8648. https://doi.org/10.3390/ijms22168648
Fukumizu M, Takashima S, Becker LE (1995) Neonatal posthemorrhagic hydrocephalus: neuropathologic and immunohistochemical studies. Pediatr Neurol 13:230–234. https://doi.org/10.1016/0887-8994(95)00183-g
Galbreath E, Kim SJ, Park K, Brenner M, Messing A (1995) Overexpression of TGF-beta 1 in the central nervous system of transgenic mice results in hydrocephalus. J Neuropathol Exp Neurol 54:339–349. https://doi.org/10.1097/00005072-199505000-00007
Giray S, Sen O, Sarica FB, Tufan K, Karatas M, Goksel BK, Yerdelen D, Cekinmez M, Can U (2009) Spontaneous primary intraventricular hemorrhage in adults: clinical data, etiology and outcome. Turk Neurosurg 19:338–344
Gjerris F, Børgesen SE, Sørensen PS, Boesen F, Schmidt K, Harmsen A, Lester J (1987) Resistance to cerebrospinal fluid outflow and intracranial pressure in patients with hydrocephalus after subarachnoid haemorrhage. Acta Neurochir (Wien) 88:79–86. https://doi.org/10.1007/bf01404142
Gram M, Sveinsdottir S, Cinthio M, Sveinsdottir K, Hansson SR, Mörgelin M, Åkerström B, Ley D (2014) Extracellular hemoglobin - mediator of inflammation and cell death in the choroid plexus following preterm intraventricular hemorrhage. J Neuroinflammation 11:200. https://doi.org/10.1186/s12974-014-0200-9
Hayashi M, Kobayashi H, Kawano H, Handa Y, Yamamoto S, Kitano T (1985) ICP patterns and isotope cisternography in patients with communicating hydrocephalus following rupture of intracranial aneurysm. J Neurosurg 62:220–226. https://doi.org/10.3171/jns.1985.62.2.0220
Heep A, Bartmann P, Stoffel-Wagner B, Bos A, Hoving E, Brouwer O, Teelken A, Schaller C, Sival D (2006) Cerebrospinal fluid obstruction and malabsorption in human neonatal hydrocephaly. Childs Nerv Syst 22:1249–1255. https://doi.org/10.1007/s00381-006-0102-y
Heisey SR, Held D, Pappenheimer JR (1962) Bulk flow and diffusion in the cerebrospinal fluid system of the goat. Am J Physiol 203:775–781. https://doi.org/10.1152/ajplegacy.1962.203.5.775
Hill A, Shackelford GD, Volpe JJ (1984) A potential mechanism of pathogenesis for early posthemorrhagic hydrocephalus in the premature newborn. Pediatrics 73:19–21
Hochstetler A, Raskin J, Blazer-Yost BL (2022) Hydrocephalus: historical analysis and considerations for treatment. Eur J Med Res 27:168. https://doi.org/10.1186/s40001-022-00798-6
Holste KG, Xia F, Ye F, Keep RF, Xi G (2022) Mechanisms of neuroinflammation in hydrocephalus after intraventricular hemorrhage: a review. Fluids Barriers CNS 19:28. https://doi.org/10.1186/s12987-022-00324-0
Hydrocephalus A (1841) or water in the head, an inflammatory disease, and curable equally and by the same means with other diseases of inflammation. Br Foreign Med Rev 11:151–158
Javaheri S, Wagner KR (1993) Bumetanide decreases canine cerebrospinal fluid production. In vivo evidence for NaCl cotransport in the central nervous system. J Clin Invest 92:2257–2261. https://doi.org/10.1172/jci116829
Johanson CE, Szmydynger-Chodobska J, Chodobski A, Baird A, McMillan P, Stopa EG (1999) Altered formation and bulk absorption of cerebrospinal fluid in FGF-2-induced hydrocephalus. Am J Physiol 277:R263–R271. https://doi.org/10.1152/ajpregu.1999.277.1.R263
Kahle KT, Kulkarni AV, Limbrick DD Jr, Warf BC (2016) Hydrocephalus in children. Lancet 387:788–799. https://doi.org/10.1016/s0140-6736(15)60694-8
Karimy JK, Kahle KT, Kurland DB, Yu E, Gerzanich V, Simard JM (2015) A novel method to study cerebrospinal fluid dynamics in rats. J Neurosci Methods 241:78–84. https://doi.org/10.1016/j.jneumeth.2014.12.015
Karimy JK, Reeves BC, Damisah E, Duy PQ, Antwi P, David W, Wang K, Schiff SJ, Limbrick DD Jr, Alper SL, Warf BC, Nedergaard M, Simard JM, Kahle KT (2020) Inflammation in acquired hydrocephalus: pathogenic mechanisms and therapeutic targets. Nat Rev Neurol 16:285–296. https://doi.org/10.1038/s41582-020-0321-y
Karimy JK, Zhang J, Kurland DB, Theriault BC, Duran D, Stokum JA, Furey CG, Zhou X, Mansuri MS, Montejo J, Vera A, DiLuna ML, Delpire E, Alper SL, Gunel M, Gerzanich V, Medzhitov R, Simard JM, Kahle KT (2017) Inflammation-dependent cerebrospinal fluid hypersecretion by the choroid plexus epithelium in posthemorrhagic hydrocephalus. Nat Med 23:997–1003. https://doi.org/10.1038/nm.4361
Kazumata K, Kamiyama H, Ishikawa T, Makino K, Nakamura T, Takizawa K, Komeichi T, Kubota T (2006) Clinical study of cerebrospinal fluid dynamics using 111In-DTPA SPECT in patients with subarachnoid hemorrhage. Neurol Med Chir (Tokyo) 46:11–17. https://doi.org/10.2176/nmc.46.11
Kim DJ, Kim H, Kim YT, Yoon BC, Czosnyka Z, Park KW, Czosnyka M (2015) Thresholds of resistance to CSF outflow in predicting shunt responsiveness. Neurol Res 37:332–340. https://doi.org/10.1179/1743132814y.0000000454
Kitazawa K, Tada T (1994) Elevation of transforming growth factor-beta 1 level in cerebrospinal fluid of patients with communicating hydrocephalus after subarachnoid hemorrhage. Stroke 25:1400–1404. https://doi.org/10.1161/01.str.25.7.1400
Kosteljanetz M (1984) CSF dynamics in patients with subarachnoid and/or intraventricular hemorrhage. J Neurosurg 60:940–946. https://doi.org/10.3171/jns.1984.60.5.0940
Krishnamurthy S, Li J, Schultz L, McAllister JP 2nd (2009) Intraventricular infusion of hyperosmolar dextran induces hydrocephalus: a novel animal model of hydrocephalus. Cerebrospinal Fluid Res 6:16. https://doi.org/10.1186/1743-8454-6-16
Kuo LT, Huang AP (2021) The pathogenesis of hydrocephalus following aneurysmal subarachnoid hemorrhage. Int J Mol Sci 22. https://doi.org/10.3390/ijms22095050
Li Q, Ding Y, Krafft P, Wan W, Yan F, Wu G, Zhang Y, Zhan Q, Zhang JH (2018) Targeting germinal matrix hemorrhage-induced overexpression of sodium-coupled bicarbonate exchanger reduces posthemorrhagic hydrocephalus formation in neonatal rats. J Am Heart Assoc 7. https://doi.org/10.1161/jaha.117.007192
Lindeman GJ, Dagnino L, Gaubatz S, Xu Y, Bronson RT, Warren HB, Livingston DM (1998) A specific, nonproliferative role for E2F-5 in choroid plexus function revealed by gene targeting. Genes Dev 12:1092–1098. https://doi.org/10.1101/gad.12.8.1092
Liu G, Mestre H, Sweeney AM, Sun Q, Weikop P, Du T, Nedergaard M (2020) Direct measurement of cerebrospinal fluid production in mice. Cell Rep 33:108524. https://doi.org/10.1016/j.celrep.2020.108524
Lodhia KR, Shakui P, Keep RF (2006) Hydrocephalus in a rat model of intraventricular hemorrhage. Acta Neurochir Suppl 96:207–211. https://doi.org/10.1007/3-211-30714-1_45
Lolansen SD, Rostgaard N, Barbuskaite D, Capion T, Olsen MH, Norager NH, Vilhardt F, Andreassen SN, Toft-Bertelsen TL, Ye F, Juhler M, Keep RF, MacAulay N (2022) Posthemorrhagic hydrocephalus associates with elevated inflammation and CSF hypersecretion via activation of choroidal transporters. Fluids Barriers CNS 19:62. https://doi.org/10.1186/s12987-022-00360-w
Lummis NC, Sánchez-Pavón P, Kennedy G, Frantz AJ, Kihara Y, Blaho VA, Chun J (2019) LPA(1/3) overactivation induces neonatal posthemorrhagic hydrocephalus through ependymal loss and ciliary dysfunction. Sci Adv 5:eaax2011. https://doi.org/10.1126/sciadv.aax2011
MacAulay N (2021) Molecular mechanisms of brain water transport. Nat Rev Neurosci 22:326–344. https://doi.org/10.1038/s41583-021-00454-8
Malm J, Lundkvist B, Eklund A, Koskinen LO, Kristensen B (2004) CSF outflow resistance as predictor of shunt function. A long-term study. Acta Neurol Scand 110:154–160. https://doi.org/10.1111/j.1600-0404.2004.00302.x
Manaenko A, Lekic T, Barnhart M, Hartman R, Zhang JH (2014) Inhibition of transforming growth factor-β attenuates brain injury and neurological deficits in a rat model of germinal matrix hemorrhage. Stroke 45:828–834. https://doi.org/10.1161/strokeaha.113.003754
Mansoor N, Solheim O, Fredriksli OA, Gulati S (2021) Shunt complications and revisions in children: a retrospective single institution study. Brain Behav 11:e2390. https://doi.org/10.1002/brb3.2390
Mayfrank L, Kissler J, Raoofi R, Delsing P, Weis J, Küker W, Gilsbach JM (1997) Ventricular dilatation in experimental intraventricular hemorrhage in pigs. Characterization of cerebrospinal fluid dynamics and the effects of fibrinolytic treatment. Stroke 28:141–148. https://doi.org/10.1161/01.str.28.1.141
McAllister JP 2nd, Williams MA, Walker ML, Kestle JR, Relkin NR, Anderson AM, Gross PH, Browd SR (2015) An update on research priorities in hydrocephalus: overview of the third National Institutes of Health-sponsored symposium "Opportunities for Hydrocephalus Research: Pathways to Better Outcomes". J Neurosurg 123:1427–1438. https://doi.org/10.3171/2014.12.Jns132352
McAllister JP, Guerra MM, Ruiz LC, Jimenez AJ, Dominguez-Pinos D, Sival D, den Dunnen W, Morales DM, Schmidt RE, Rodriguez EM, Limbrick DD (2017) Ventricular zone disruption in human neonates with intraventricular hemorrhage. J Neuropathol Exp Neurol 76:358–375. https://doi.org/10.1093/jnen/nlx017
Moinuddin SM, Tada T (2000) Study of cerebrospinal fluid flow dynamics in TGF-beta 1 induced chronic hydrocephalic mice. Neurol Res 22:215–222. https://doi.org/10.1080/01616412.2000.11741064
Motohashi O, Suzuki M, Yanai N, Umezawa K, Shida N, Yoshimoto T (1995) Thrombin and TGF-beta promote human leptomeningeal cell proliferation in vitro. Neurosci Lett 190:105–108. https://doi.org/10.1016/0304-3940(95)11513-v
Nielsen S, Smith BL, Christensen EI, Agre P (1993) Distribution of the aquaporin CHIP in secretory and resorptive epithelia and capillary endothelia. Proc Natl Acad Sci U S A 90:7275–7279. https://doi.org/10.1073/pnas.90.15.7275
Oernbo EK, Steffensen AB, Razzaghi Khamesi P, Toft-Bertelsen TL, Barbuskaite D, Vilhardt F, Gerkau NJ, Tritsaris K, Simonsen AH, Lolansen SD, Andreassen SN, Hasselbalch SG, Zeuthen T, Rose CR, Kurtcuoglu V, MacAulay N (2022) Membrane transporters control cerebrospinal fluid formation independently of conventional osmosis to modulate intracranial pressure. Fluids Barriers CNS 19:65. https://doi.org/10.1186/s12987-022-00358-4
Oi S, Di Rocco C (2006) Proposal of "evolution theory in cerebrospinal fluid dynamics" and minor pathway hydrocephalus in developing immature brain. Childs Nerv Syst 22:662–669. https://doi.org/10.1007/s00381-005-0020-4
Orešković D, Klarica M (2014) Measurement of cerebrospinal fluid formation and absorption by ventriculo-cisternal perfusion: what is really measured? Croat Med J 55:317–327. https://doi.org/10.3325/cmj.2014.55.317
Oreskovic D, Klarica M, Vukic M, Marakovic J (2003) Evaluation of ventriculo-cisternal perfusion model as a method to study cerebrospinal fluid formation. Croat Med J 44:161–164
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj 372:n71. https://doi.org/10.1136/bmj.n71
Passero S, Ulivelli M, Reale F (2002) Primary intraventricular haemorrhage in adults. Acta Neurol Scand 105:115–119. https://doi.org/10.1034/j.1600-0404.2002.1o118.x
Pearce RK, Collins P, Jenner P, Emmett C, Marsden CD (1996) Intraventricular infusion of basic fibroblast growth factor (bFGF) in the MPTP-treated common marmoset. Synapse 23:192–200. https://doi.org/10.1002/(sici)1098-2396(199607)23:3%3C192::Aid-syn8.3.0.Co;2-3
Proulx ST (2021) Cerebrospinal fluid outflow: a review of the historical and contemporary evidence for arachnoid villi, perineural routes, and dural lymphatics. Cell Mol Life Sci 78:2429–2457. https://doi.org/10.1007/s00018-020-03706-5
Reddy GK, Bollam P, Caldito G (2014) Long-term outcomes of ventriculoperitoneal shunt surgery in patients with hydrocephalus. World Neurosurg 81:404–410. https://doi.org/10.1016/j.wneu.2013.01.096
Redzic ZB, Segal MB (2004) The structure of the choroid plexus and the physiology of the choroid plexus epithelium. Adv Drug Deliv Rev 56:1695–1716. https://doi.org/10.1016/j.addr.2004.07.005
Rekate HL (2011) A consensus on the classification of hydrocephalus: its utility in the assessment of abnormalities of cerebrospinal fluid dynamics. Childs Nerv Syst 27:1535–1541. https://doi.org/10.1007/s00381-011-1558-y
Riva-Cambrin J, Kestle JRW, Rozzelle CJ, Naftel RP, Alvey JS, Reeder RW, Holubkov R, Browd SR, Cochrane DD, Limbrick DD, Shannon CN, Simon TD, Tamber MS, Wellons JC, Whitehead WE, Kulkarni AV (2019) Predictors of success for combined endoscopic third ventriculostomy and choroid plexus cauterization in a North American setting: a Hydrocephalus Clinical Research Network study. J Neurosurg Pediatr 24:128–138. https://doi.org/10.3171/2019.3.Peds18532
Robert SM, Reeves BC, Kiziltug E, Duy PQ, Karimy JK, Mansuri MS, Marlier A, Allington G, Greenberg ABW, DeSpenza T Jr, Singh AK, Zeng X, Mekbib KY, Kundishora AJ, Nelson-Williams C, Hao LT, Zhang J, Lam TT, Wilson R et al (2023) The choroid plexus links innate immunity to CSF dysregulation in hydrocephalus. Cell 186:764–785.e721. https://doi.org/10.1016/j.cell.2023.01.017
Sadegh C, Xu H, Sutin J, Fatou B, Gupta S, Pragana A, Taylor M, Kalugin PN, Zawadzki ME, Alturkistani O, Shipley FB, Dani N, Fame RM, Wurie Z, Talati P, Schleicher RL, Klein EM, Zhang Y, Holtzman MJ et al (2023) Choroid plexus-targeted NKCC1 overexpression to treat post-hemorrhagic hydrocephalus. Neuron. https://doi.org/10.1016/j.neuron.2023.02.020
Shibukawa S, Miyati T, Niwa T, Matsumae M, Ogino T, Horie T, Imai Y, Muro I (2018) Time-spatial labeling inversion pulse (Time-SLIP) with pencil beam pulse: a selective labeling technique for observing cerebrospinal fluid flow dynamics. Magn Reson Med Sci 17:259–264. https://doi.org/10.2463/mrms.tn.2017-0032
Simard PF, Tosun C, Melnichenko L, Ivanova S, Gerzanich V, Simard JM (2011) Inflammation of the choroid plexus and ependymal layer of the ventricle following intraventricular hemorrhage. Transl Stroke Res 2:227–231. https://doi.org/10.1007/s12975-011-0070-8
Steffensen AB, Oernbo EK, Stoica A, Gerkau NJ, Barbuskaite D, Tritsaris K, Rose CR, MacAulay N (2018) Cotransporter-mediated water transport underlying cerebrospinal fluid formation. Nat Commun 9:2167. https://doi.org/10.1038/s41467-018-04677-9
Stein M, Luecke M, Preuss M, Boeker DK, Joedicke A, Oertel MF (2010) Spontaneous intracerebral hemorrhage with ventricular extension and the grading of obstructive hydrocephalus: the prediction of outcome of a special life-threatening entity. Neurosurgery 67:1243–1251; discussion 1252. https://doi.org/10.1227/NEU.0b013e3181ef25de
Strahle J, Garton HJ, Maher CO, Muraszko KM, Keep RF, Xi G (2012) Mechanisms of hydrocephalus after neonatal and adult intraventricular hemorrhage. Transl Stroke Res 3:25–38. https://doi.org/10.1007/s12975-012-0182-9
Takizawa H, Gabra-Sanders T, Miller JD (1985) Validity of measurements of cerebrospinal fluid outflow resistance estimated by the bolus injection method. Neurosurgery 17:63–66. https://doi.org/10.1227/00006123-198507000-00010
Takizawa T, Tada T, Kitazawa K, Tanaka Y, Hongo K, Kameko M, Uemura KI (2001) Inflammatory cytokine cascade released by leukocytes in cerebrospinal fluid after subarachnoid hemorrhage. Neurol Res 23:724–730. https://doi.org/10.1179/016164101101199243
Toft-Bertelsen TL, Barbuskaite D, Heerfordt EK, Lolansen SD, Andreassen SN, Rostgaard N, Olsen MH, Norager NH, Capion T, Rath MF, Juhler M, MacAulay N (2022) Lysophosphatidic acid as a CSF lipid in posthemorrhagic hydrocephalus that drives CSF accumulation via TRPV4-induced hyperactivation of NKCC1. Fluids Barriers CNS 19:69. https://doi.org/10.1186/s12987-022-00361-9
Ulfig N, Bohl J, Neudörfer F, Rezaie P (2004) Brain macrophages and microglia in human fetal hydrocephalus. Brain Dev 26:307–315. https://doi.org/10.1016/s0387-7604(03)00172-4
Wang Y, Pan XF, Liu GD, Liu ZH, Zhang C, Chen T, Wang YH (2021) FGF-2 suppresses neuronal autophagy by regulating the PI3K/Akt pathway in subarachnoid hemorrhage. Brain Res Bull 173:132–140. https://doi.org/10.1016/j.brainresbull.2021.05.017
Warf BC (2005) Comparison of endoscopic third ventriculostomy alone and combined with choroid plexus cauterization in infants younger than 1 year of age: a prospective study in 550 African children. J Neurosurg 103:475–481. https://doi.org/10.3171/ped.2005.103.6.0475
Weed LH (1914) Studies on cerebro-spinal fluid. No. III : the pathways of escape from the Subarachnoid Spaces with particular reference to the Arachnoid Villi. J Med Res 31:51–91
Whitelaw A (1997) We need a new understanding of the reabsorption of cerebrospinal fluid. Acta Paediatr 86:133–134. https://doi.org/10.1111/j.1651-2227.1997.tb08852.x
Whitelaw A (2001) Intraventricular haemorrhage and posthaemorrhagic hydrocephalus: pathogenesis, prevention and future interventions. Semin Neonatol 6:135–146. https://doi.org/10.1053/siny.2001.0047
Whitelaw A, Cherian S, Thoresen M, Pople I (2004) Posthaemorrhagic ventricular dilatation: new mechanisms and new treatment. Acta Paediatr Suppl 93:11–14. https://doi.org/10.1111/j.1651-2227.2004.tb03041.x
Whitelaw A, Christie S, Pople I (1999) Transforming growth factor-beta1: a possible signal molecule for posthemorrhagic hydrocephalus? Pediatr Res 46:576–580. https://doi.org/10.1203/00006450-199911000-00014
Wyss-Coray T, Feng L, Masliah E, Ruppe MD, Lee HS, Toggas SM, Rockenstein EM, Mucke L (1995) Increased central nervous system production of extracellular matrix components and development of hydrocephalus in transgenic mice overexpressing transforming growth factor-beta 1. Am J Pathol 147:53–67
Xu H, Fame RM, Sadegh C, Sutin J, Naranjo C, Della S, Cui J, Shipley FB, Vernon A, Gao F, Zhang Y, Holtzman MJ, Heiman M, Warf BC, Lin PY, Lehtinen MK (2021) Choroid plexus NKCC1 mediates cerebrospinal fluid clearance during mouse early postnatal development. Nat Commun 12:447. https://doi.org/10.1038/s41467-020-20666-3
Yamada S, Miyazaki M, Kanazawa H, Higashi M, Morohoshi Y, Bluml S, McComb JG (2008) Visualization of cerebrospinal fluid movement with spin labeling at MR imaging: preliminary results in normal and pathophysiologic conditions. Radiology 249:644–652. https://doi.org/10.1148/radiol.2492071985
Yan H, Chen Y, Li L, Jiang J, Wu G, Zuo Y, Zhang JH, Feng H, Yan X, Liu F (2016) Decorin alleviated chronic hydrocephalus via inhibiting TGF-β1/Smad/CTGF pathway after subarachnoid hemorrhage in rats. Brain Res 1630:241–253. https://doi.org/10.1016/j.brainres.2015.11.004
Yung YC, Mutoh T, Lin ME, Noguchi K, Rivera RR, Choi JW, Kingsbury MA, Chun J (2011) Lysophosphatidic acid signaling may initiate fetal hydrocephalus. Sci Transl Med 3:99ra87. https://doi.org/10.1126/scitranslmed.3002095
Zacharia BE, Vaughan KA, Hickman ZL, Bruce SS, Carpenter AM, Petersen NH, Deiner S, Badjatia N, Connolly ES Jr (2012) Predictors of long-term shunt-dependent hydrocephalus in patients with intracerebral hemorrhage requiring emergency cerebrospinal fluid diversion. Neurosurg Focus 32:E5. https://doi.org/10.3171/2012.2.Focus11372
Zhan C, Xiao G, Zhang X, Chen X, Zhang Z, Liu J (2020) Decreased MiR-30a promotes TGF-β1-mediated arachnoid fibrosis in post-hemorrhagic hydrocephalus. Transl Neurosci 11:60–74. https://doi.org/10.1515/tnsci-2020-0010
Zhang C, Long SY, You WD, Xu XX, Gao GY, Yang XF (2022) The value of the correlation coefficient between the ICP wave amplitude and the mean ICP level (RAP) combined with the resistance to CSF outflow (Rout) for early prediction of the outcome before shunting in posttraumatic hydrocephalus. Front Neurol 13:881568. https://doi.org/10.3389/fneur.2022.881568
Zhang Z, Tan Q, Guo P, Huang S, Jia Z, Liu X, Feng H, Chen Y (2022) NLRP3 inflammasome-mediated choroid plexus hypersecretion contributes to hydrocephalus after intraventricular hemorrhage via phosphorylated NKCC1 channels. J Neuroinflammation 19:163. https://doi.org/10.1186/s12974-022-02530-x
Code availability
Not applicable.
Funding
This project was funded by the IMK Almene Fond (to NM) and the Novo Nordisk Foundation (Tandem Grant NNF17OC0024718 to NM).
Author information
Authors and Affiliations
Contributions
Idea conception: NM; design of study protocol/search strategy: SBS, NM; literature search: SBS; data analysis: SBS, SDL; writing—original draft preparation: SBS; writing—review and editing: SDL; critical revision: TIM, NM.
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ben-Shoshan, S.D., Lolansen, S.D., Mathiesen, T.I. et al. CSF hypersecretion versus impaired CSF absorption in posthemorrhagic hydrocephalus: a systematic review. Acta Neurochir 165, 3271–3287 (2023). https://doi.org/10.1007/s00701-023-05746-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05746-9