Abstract
Background
Traumatic peroneal nerve injuries are typically associated with high-energy injuries. The aim of this study was to evaluate the demographics and outcomes following surgical management of peroneal nerve injuries.
Methods
Patients evaluated at a single institution with peroneal nerve injuries between 2001 and 2022 were retrospectively reviewed. Mechanism of injury, time to surgery, pre- and postoperative examinations, and operative reports were recorded. Satisfactory outcome, defined as the ability to achieve anti-gravity dorsiflexion strength or stronger following surgery, was compared between nerve grafting and nerve transfers in patients with at least 9 months of postoperative follow-up.
Results
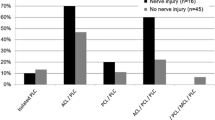
Thirty-seven patients had follow-up greater than 9 months after surgery, with an average follow-up of 3.8 years. Surgeries included neurolysis (n=5), direct repair (n=2), tibial motor nerve fascicle transfer to the anterior tibialis motor branch (n=18), or interposition nerve grafting using sural nerve autograft (n=12). At last follow-up, 59.5% (n=22) of patients had anti-gravity strength or stronger dorsiflexion. Nineteen (51.4%) patients used an ankle-foot orthosis during all or some activities. In patients that underwent nerve grafting only across the peroneal nerve defect, 44.4% (n=4) were able to achieve anti-gravity strength or stronger dorsiflexion. In patients that had a tibial nerve fascicle transfer to the tibialis anterior motor branch of the peroneal nerve, 42.9% (n=6) were able to achieve anti-gravity strength or stronger dorsiflexion at last follow-up. There was no statistical difference between nerve transfers and nerve grafting in postoperative dorsiflexion strength (p = 0.51).
Conclusion
Peroneal nerve injuries frequently occur in the setting of knee dislocations and similar high-energy injuries. Nerve surgery is not universally successful in restoration of ankle dorsiflexion, with one-third of patients requiring an ankle-foot orthosis at mid-term follow-up. Patients should be properly counseled on the treatment challenges and variable outcomes following peroneal nerve injuries.

Similar content being viewed by others
Abbreviations
- AFO:
-
Ankle-foot orthosis
- PTT:
-
Posterior tibial tendon
- mBMRC:
-
Modified British Medical Research Council
- BMI:
-
Body mass index
- CPN:
-
Common peroneal nerve
- y:
-
Years
- n :
-
Number
- SD:
-
Standard deviation
- mm:
-
Millimeter
References
Becker EH, Watson JD, Dreese JC (2013) Investigation of multiligamentous knee injury patterns with associated injuries presenting at a level I trauma center. J Orthop Trauma 27:226–231. https://doi.org/10.1097/BOT.0b013e318270def4
Chaing YH, Chang MC, Liu Y, Lo WH (2000) Surgical treatment for peroneal nerve palsy. Zhonghua Yi Xue Za Zhi 63:591–597
Cho D, Saetia K, Lee S, Kline DG, Kim DH (2011) Peroneal nerve injury associated with sports-related knee injury. Neurosurg Focus 31:E11. https://doi.org/10.3171/2011.9.Focus11187
Ciaramitaro P, Mondelli M, Logullo F, Grimaldi S, Battiston B, Sard A, Scarinzi C, Migliaretti G, Faccani G, Cocito D (2010) Traumatic peripheral nerve injuries: epidemiological findings, neuropathic pain and quality of life in 158 patients. J Peripher Nerv Syst 15:120–127. https://doi.org/10.1111/j.1529-8027.2010.00260.x
Ferris S, Maciburko SJ (2017) Partial tibial nerve transfer to tibialis anterior for traumatic peroneal nerve palsy. Microsurgery 37:596–602. https://doi.org/10.1002/micr.30174
Garozzo D, Ferraresi S, Buffatti P (2004) Surgical treatment of common peroneal nerve injuries: indications and results. A series of 62 cases. J Neurosurg Sci 48:105–112 discussion 112
Gatskiy AA, Tretyak IB, Tretiakova AI, Tsymbaliuk YV (2019) Choosing the target wisely: partial tibial nerve transfer to extensor digitorum motor branches with simultaneous posterior tibial tendon transfer. Could this be a way to improve functional outcome and gait biomechanics? J Neurosurg:1–9. https://doi.org/10.3171/2019.3.Jns182866
Giuffre JL, Bishop AT, Spinner RJ, Levy BA, Shin AY (2012) Partial tibial nerve transfer to the tibialis anterior motor branch to treat peroneal nerve injury after knee trauma. Clin Orthop Relat Res 470:779–790. https://doi.org/10.1007/s11999-011-1924-9
Gosk J, Rutowski R, Rabczyński J (2005) The lower extremity nerve injuries - own experience in surgical treatment. Folia Neuropathol 43:148–152
Harner CD, Waltrip RL, Bennett CH, Francis KA, Cole B, Irrgang JJ (2004) Surgical management of knee dislocations. J Bone Joint Surg Am 86:262–273. https://doi.org/10.2106/00004623-200402000-00008
Ho B, Khan Z, Switaj PJ, Ochenjele G, Fuchs D, Dahl W, Cederna P, Kung TA, Kadakia AR (2014) Treatment of peroneal nerve injuries with simultaneous tendon transfer and nerve exploration. J Orthop Surg Res 9:67. https://doi.org/10.1186/s13018-014-0067-6
Hochman MG, Zilberfarb JL (2004) Nerves in a pinch: imaging of nerve compression syndromes. Radiologic Clinics 42:221–245
Horteur C, Forli A, Corcella D, Pailhé R, Lateur G, Saragaglia D (2019) Short- and long-term results of common peroneal nerve injuries treated by neurolysis, direct suture or nerve graft. Eur J Orthop Surg Traumatol 29:893–898. https://doi.org/10.1007/s00590-018-2354-0
Jennette MR, Payne R, Rizk E (2020) Internal neurolysis of the common peroneal nerve with lower extremity flexion increases likelihood for direct end-end nerve repairs. Cureus 12:e10355. https://doi.org/10.7759/cureus.10355
Johnson KA, Strom DE (1989) Tibialis posterior tendon dysfunction. Clin Orthop Relat Res 239:196–206
Johnson ME, Foster L, DeLee JC (2008) Neurologic and vascular injuries associated with knee ligament injuries. Am J Sports Med 36:2448–2462. https://doi.org/10.1177/0363546508325669
Kim DH, Kline DG (1996) Management and results of peroneal nerve lesions. Neurosurgery 39:312–319; discussion 319-320. https://doi.org/10.1097/00006123-199608000-00014
Kim DH, Murovic JA, Tiel RL, Kline DG (2004) Management and outcomes in 318 operative common peroneal nerve lesions at the Louisiana State University Health Sciences Center. Neurosurgery 54:1421–1428; discussion 1428-1429. https://doi.org/10.1227/01.neu.0000124752.40412.03
Krych AJ, Giuseffi SA, Kuzma SA, Stuart MJ, Levy BA (2014) Is peroneal nerve injury associated with worse function after knee dislocation? Clin Orthop Relat Res 472:2630–2636. https://doi.org/10.1007/s11999-014-3542-9
Kutubidze A (2009) Upper and lower extremities nerve injuries--own experience in surgical treatment. Georgian Med News (166):7–9
Leclère FM, Badur N, Mathys L, Vögelin E (2015) Nerve transfers for persistent traumatic peroneal nerve palsy: the Inselspital Bern experience. Neurosurgery 77:572–579; discussion 579-580. https://doi.org/10.1227/neu.0000000000000897
Lingaiah P, Jaykumar K, Sural S, Dhal A (2018) Functional evaluation of early tendon transfer for foot drop. J Orthop Surg 26:2309499018799766. https://doi.org/10.1177/2309499018799766
Mackay MJ, Ayres JM, Harmon IP, Tarakemeh A, Brubacher J, Vopat BG (2022) Traumatic peroneal nerve injuries: a systematic review. JBJS Reviews 10:e20.00256. https://doi.org/10.2106/jbjs.Rvw.20.00256
Matejcik V, Steno J, Benetin J, Kuchar M (2001) Surgical treatment of injuries of nervus fibularis. Bratisl Lek Listy 102:361–364
Moatshe G, Dornan GJ, Løken S, Ludvigsen TC, LaPrade RF, Engebretsen L (2017) Demographics and injuries associated with knee dislocation: a prospective review of 303 patients. Orthop J Sports Med 5:2325967117706521. https://doi.org/10.1177/2325967117706521
Mont MA, Dellon AL, Chen F, Hungerford MW, Krackow KA, Hungerford DS (1996) The operative treatment of peroneal nerve palsy. J Bone Joint Surg Am 78:863–869
Niall DM, Nutton RW, Keating JF (2005) Palsy of the common peroneal nerve after traumatic dislocation of the knee. J Bone Joint Surg 87:664–667. https://doi.org/10.1302/0301-620x.87b5.15607
Noble J, Munro CA, Prasad VS, Midha R (1998) Analysis of upper and lower extremity peripheral nerve injuries in a population of patients with multiple injuries. J Trauma 45:116–122. https://doi.org/10.1097/00005373-199807000-00025
Noland SS, Bishop AT, Spinner RJ, Shin AY (2019) Adult traumatic brachial plexus injuries. J Am Acad Orthop Surg 27:705–716. https://doi.org/10.5435/jaaos-d-18-00433
Ozkan T, Tuncer S, Ozturk K, Aydin A, Ozkan S (2009) Tibialis posterior tendon transfer for persistent drop foot after peroneal nerve repair. J Reconstr Microsurg 25:157–164. https://doi.org/10.1055/s-0028-1103502
Peskun CJ, Chahal J, Steinfeld ZY, Whelan DB (2012) Risk factors for peroneal nerve injury and recovery in knee dislocation. Clin Orthop Relat Res 470:774–778. https://doi.org/10.1007/s11999-011-1981-0
Prahinski JR, McHale KA, Temple HT, Jackson JP (1996) Bridle transfer for paresis of the anterior and lateral compartment musculature. Foot Ankle Int 17:615–619. https://doi.org/10.1177/107110079601701005
Roganovic Z (2005) Missile-caused complete lesions of the peroneal nerve and peroneal division of the sciatic nerve: results of 157 repairs. Neurosurgery 57:1201–1212; discussion 1201-1212. https://doi.org/10.1227/01.neu.0000186034.58798.bf
Ryan W, Mahony N, Delaney M, O'Brien M, Murray P (2003) Relationship of the common peroneal nerve and its branches to the head and neck of the fibula. Clin Anat 16:501–505
Seidel JA, Koenig R, Antoniadis G, Richter HP, Kretschmer T (2008) Surgical treatment of traumatic peroneal nerve lesions. Neurosurgery 62:664–673; discussion 664-673. https://doi.org/10.1227/01.neu.0000317315.48612.b1
Senes FM, Campus R, Becchetti F, Catena N (2007) Lower limb nerve injuries in children. Microsurgery 27:32–36. https://doi.org/10.1002/micr.20304
Sunderland S (1965) The connective tissues of peripheral nerves. Brain 88:841–854
Sunderland S, Bradley K (1949) The cross-sectional area of peripheral nerve trunks devoted to nerve fibres. Brain 72:428–449
Sunderland S, Ray LJ (1948) The intraneural topography of the sciatic nerve and its popliteal divisions in man. Brain 71:242–273. https://doi.org/10.1093/brain/71.3.242
Terzis JK, Kostas I (2020) Outcomes with microsurgery of common peroneal nerve lesions. J Plast Reconstr Aesthet Surg 73:72–80. https://doi.org/10.1016/j.bjps.2019.02.031
Terzis JK, Kostopoulos VK (2010) Vascularized nerve grafts for lower extremity nerve reconstruction. Ann Plast Surg 64:169–176. https://doi.org/10.1097/SAP.0b013e3181a5742
Toussaint CP, Perry EC, Pisansky MT, Anderson DE (2010) What’s new in the diagnosis and treatment of peripheral nerve entrapment neuropathies. Neurol Clin 28:979–1004
Van den Bergh FR, Vanhoenacker FM, De Smet E, Huysse W, Verstraete KL (2013) Peroneal nerve: normal anatomy and pathologic findings on routine MRI of the knee. Insights Imaging 4:287–299. https://doi.org/10.1007/s13244-013-0255-7
Vieira R, Rosenberg Z, Kiprovski K (2007) Musculoskeletal imaging-original research-MRI of the distal biceps femoris muscle: normal anatomy, variants, and association with common peroneal entrapment neuropathy. Am J Roentgenol 189:549–555
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Courtney Carlson Strother and Lauren E. Dittman. The first draft of the manuscript was written by Courtney Carlson Strother, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Mayo Clinic and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was conducted retrospectively from data obtained for clinical purpose. We consulted with the IRB of Mayo Clinic who determined that our study did not need ethical approval. An IRB official waiver of ethical approval was granted from the IRB of Mayo Clinic.
Conflict of interest
CCS, LED, and ATB certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. Author AYS receives royalties from Mayo Medical Ventures and TriMed and is on the editorial or governing board of Techniques in Hand and Upper Extremity Surgery. RJS receives royalties from Johnson & Johnson, Mayo Medical Ventures, and Saunders/Mosby-Elsevier and is part of the editorial or governing board of Clinical Anatomy, J Surgical Orthopedic Advances, Mayo Clinic Proceedings, Neurosurgery, and World Neurosurgery.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Carlson Strother, C., Dittman, L.E., Spinner, R.J. et al. Surgical management of peroneal nerve injuries. Acta Neurochir 165, 2573–2580 (2023). https://doi.org/10.1007/s00701-023-05727-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05727-y