Abstract
Background
Chronically elevated intracranial pressure (ICP) seen in idiopathic intracranial hypertension (IIH) can cause the development of skull base encephaloceles and cerebrospinal fluid (CSF) leaks. Surgical repair and ventriculoperitoneal shunt (VPS) placement are mainstays of treatment. Venous sinus stenting (VSS) is a newly accepted treatment modality. The goal of this study was thus to determine if VSS can be used to treat symptoms and prevent recurrence after surgical encephalocele repair.
Methods
Retrospective chart review of patients that had surgical repair of encephaloceles followed by VSS for symptomatic stenosis with elevated pressure gradient.
Results
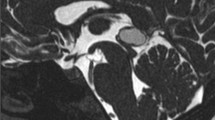
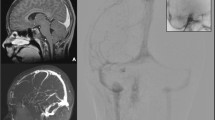
A total of 13 patients underwent a combined encephalocele repair and VSS. Seventy-two percent were female; 46% had headaches, 69% pulsatile tinnitus, and 92% CSF rhinorrhea or otorrhea. One had seizures. Mean lumbar opening pressure was 23.3 ± 2.6 cm H2O; the average sagittal-to-jugular pressure gradient was 12.7 ± 1.8 cmH2O and was elevated in all patients. Four patients had middle fossa craniotomy for repair of tegmen defect (one bilateral); one had a retrosigmoid craniotomy for repair of a sigmoid plate defect. Eight had an endoscopic endonasal repair for sphenoid or cribriform plate encephalocele. There were no VSS procedural complications or complications associated with dual antiplatelet therapy. One patient had meningitis after endoscopic repair that was treated with antibiotics. One patient had recurrence of both CSF leak and venous stenosis adjacent to the stent requiring repeat repair and VSS. There was no further recurrence.
Conclusion
In patients with dural sinus stenosis and encephaloceles requiring repair, VSS can be performed safely within weeks of surgery for relief of symptoms, resolution of underlying pathology, and prevention of CSF leak recurrence.




Similar content being viewed by others
References
Akhter A, Schulz L, Inger HE, McGregor JM (2022) Current indications for management options in pseudotumor cerebri. Neurol Clin 40:391–404. https://doi.org/10.1016/j.ncl.2021.11.011
Algattas HN, Wang EW, Zenonos GA, Snyderman CH, Gardner PA (2021) Endoscopic endonasal surgery for anterior cranial fossa meningiomas. J Neurosurg Sci 65:118–132. https://doi.org/10.23736/s0390-5616.20.05085-7
Arnaout MM, Hanz SZ, Heier LA, Schwartz TH (2021) Prevalence and outcome of anterior and middle cranial fossae encephaloceles without cerebrospinal fluid leak or meningitis. World Neurosurg 149:e828–e835. https://doi.org/10.1016/j.wneu.2021.01.088
Barrero Ruiz E, Iglesias Moroño S, Ros López B, Morales Martinez A, Díaz T, Arráez Sánchez M (2022) Life-threatening idiopathic intracranial hypertension: the role of venous sinus stenting. Childs Nerv Syst. https://doi.org/10.1007/s00381-022-05564-x
Bidot S, Levy JM, Saindane AM, Narayana KM, Dattilo M, DelGaudio JM, Mattox DE, Oyesiku NM, Peragallo JH, Solares CA, Vivas EX, Wise SK, Newman NJ, Biousse V (2021) Spontaneous skull base cerebrospinal fluid leaks and their relationship to idiopathic intracranial hypertension. Am J Rhinol Allergy 35:36–43. https://doi.org/10.1177/1945892420932490
Bidot S, Levy JM, Saindane AM, Oyesiku NM, Newman NJ, Biousse V (2019) Do most patients with a spontaneous cerebrospinal fluid leak have idiopathic intracranial hypertension? J Neuroophthalmol 39:487–495. https://doi.org/10.1097/wno.0000000000000761
Camras LR, Ecanow JS, Abood CA (1998) Spontaneous cerebrospinal fluid rhinorrhea in a patient with pseudotumor cerebri. J Neuroimaging 8:41–42. https://doi.org/10.1111/jon19988141
Carrau RL, Snyderman CH, Kassam AB (2005) The management of cerebrospinal fluid leaks in patients at risk for high-pressure hydrocephalus. Laryngoscope 115:205–212. https://doi.org/10.1097/01.mlg.0000154719.62668.70
Dinkin MJ, Patsalides A (2017) Venous sinus stenting for idiopathic intracranial hypertension: where are we now? Neurol Clin 35:59–81. https://doi.org/10.1016/j.ncl.2016.08.006
Fargen KM (2022) Venous stenting for idiopathic intracranial hypertension: lessons learned from a high-volume practice. J Neurointerv Surg 14:528–532. https://doi.org/10.1136/neurintsurg-2021-018184
Fargen KM, Liu K, Garner RM, Greeneway GP, Wolfe SQ, Crowley RW (2018) Recommendations for the selection and treatment of patients with idiopathic intracranial hypertension for venous sinus stenting. J Neurointerv Surg 10:1203–1208. https://doi.org/10.1136/neurintsurg-2018-014042
Ha CM, Hong SD, Choi JW, Seol HJ, Nam DH, Lee JI, Kong DS (2021) Graded reconstruction strategy using a multilayer technique without lumbar drainage after endoscopic endonasal surgery. World Neurosurg. https://doi.org/10.1016/j.wneu.2021.11.003
Hanz SZ, Lt A, Schmidt F, Kacker A, Tsiouris AJ, Anand VK, Schwartz TH (2020) Low incidence of true Sternberg’s canal defects among lateral sphenoid sinus encephaloceles. Acta Neurochir (Wien) 162:2413–2420. https://doi.org/10.1007/s00701-020-04329-2
Hegazy HM, Carrau RL, Snyderman CH, Kassam A, Zweig J (2000) Transnasal endoscopic repair of cerebrospinal fluid rhinorrhea: a meta-analysis. Laryngoscope 110:1166–1172. https://doi.org/10.1097/00005537-200007000-00019
Hong CS, Kundishora AJ, Elsamadicy AA, Vining EM, Manes RP, Omay SB (2022) A unique subset: idiopathic intracranial hypertension presenting as spontaneous CSF leak of the anterior skull base. J Neurol Surg B Skull Base 83:105–115. https://doi.org/10.1055/s-0040-1716898
Hubbard JL, McDonald TJ, Pearson BW, Laws ER Jr (1985) Spontaneous cerebrospinal fluid rhinorrhea: evolving concepts in diagnosis and surgical management based on the Mayo Clinic experience from 1970 through 1981. Neurosurgery 16:314–321. https://doi.org/10.1227/00006123-198503000-00006
Kalyvas A, Neromyliotis E, Koutsarnakis C, Komaitis S, Drosos E, Skandalakis GP, Pantazi M, Gobin YP, Stranjalis G, Patsalides A (2021) A systematic review of surgical treatments of idiopathic intracranial hypertension (IIH). Neurosurg Rev 44:773–792. https://doi.org/10.1007/s10143-020-01288-1
Lal D, Cain RB (2014) Updates in reconstruction of skull base defects. Curr Opin Otolaryngol Head Neck Surg 22:419–428. https://doi.org/10.1097/moo.0000000000000082
Lee JA, Byun YJ, Nguyen SA, Schlosser RJ, Gudis DA (2020) Endonasal endoscopic surgery for pediatric anterior cranial fossa encephaloceles: a systematic review. Int J Pediatr Otorhinolaryngol 132:109919. https://doi.org/10.1016/j.ijporl.2020.109919
Lenck S, Nouet A, Shotar E, Abi Jaoudé S, Nicholson P, Premat K, Corcy C, Boch AL, Sourour NA, Tankere F, Carpentier A, Clarençon F (2021) Transverse sinus stenting without surgical repair in idiopathic CSF rhinorrhea associated with transverse sinus stenoses: a pilot study. J Neurosurg 136(6):1745–1751. https://doi.org/10.3171/2021.5.Jns21894
Manjubashini D, Kiran M, Akshaya S, Nagarajan K (2019) Intrasphenoidal encephalocele with spontaneous cerebrospinal fluid rhinorrhea in idiopathic intracranial hypertension: need for clarity in terminology and imaging delineation. World Neurosurg 132:129–133. https://doi.org/10.1016/j.wneu.2019.08.186
Martin TJ, Loehrl TA (2007) Endoscopic CSF leak repair. Curr Opin Otolaryngol Head Neck Surg 15:35–39. https://doi.org/10.1097/MOO.0b013e3280123fce
Mattox DE, Kennedy DW (1990) Endoscopic management of cerebrospinal fluid leaks and cephaloceles. Laryngoscope 100:857–862. https://doi.org/10.1288/00005537-199008000-00012
Mirza S, Thaper A, McClelland L, Jones NS (2005) Sinonasal cerebrospinal fluid leaks: management of 97 patients over 10 years. Laryngoscope 115:1774–1777. https://doi.org/10.1097/01.mlg.0000175679.68452.75
Owler BK, Allan R, Parker G, Besser M (2003) Pseudotumour cerebri, CSF rhinorrhoea and the role of venous sinus stenting in treatment. Br J Neurosurg 17:79–83. https://doi.org/10.3109/02688690309177979
Pan DW, Vanstrum E, Doherty JK (2022) Idiopathic intracranial hypertension: implications for the otolaryngologist. Otolaryngol Clin North Am 55:579–594. https://doi.org/10.1016/j.otc.2022.02.005
Peng D, Yang K, Wu C, Gao F, Sun W, Lu G (2022) Ventriculoperitoneal shunt alone for cerebrospinal fluid rhinorrhea with neuroendocrine alterations in idiopathic intracranial hypertension: a case report and literature review. Front Neurol 13:809224. https://doi.org/10.3389/fneur.2022.809224
Pérez MA, Bialer OY, Bruce BB, Newman NJ, Biousse V (2013) Primary spontaneous cerebrospinal fluid leaks and idiopathic intracranial hypertension. J Neuroophthalmol 33:330–337. https://doi.org/10.1097/WNO.0b013e318299c292
Reddy M, Baugnon K (2017) Imaging of cerebrospinal fluid rhinorrhea and otorrhea. Radiol Clin North Am 55:167–187. https://doi.org/10.1016/j.rcl.2016.08.005
Schlosser RJ, Wilensky EM, Grady MS, Palmer JN, Kennedy DW, Bolger WE (2004) Cerebrospinal fluid pressure monitoring after repair of cerebrospinal fluid leaks. Otolaryngol Head Neck Surg 130:443–448. https://doi.org/10.1016/j.otohns.2003.12.018
Schlosser RJ, Woodworth BA, Wilensky EM, Grady MS, Bolger WE (2006) Spontaneous cerebrospinal fluid leaks: a variant of benign intracranial hypertension. Ann Otol Rhinol Laryngol 115:495–500. https://doi.org/10.1177/000348940611500703
Schwarz J, Al Balushi A, Sundararajan S, Dinkin M, Oliveira C, Greenfield JP, Patsalides A (2021) Management of idiopathic intracranial hypertension in children utilizing venous sinus stenting. Interv Neuroradiol 27:257–265. https://doi.org/10.1177/1591019920976234
Sinclair AJ, Kuruvath S, Sen D, Nightingale PG, Burdon MA, Flint G (2011) Is cerebrospinal fluid shunting in idiopathic intracranial hypertension worthwhile? A 10-year review. Cephalalgia 31:1627–1633. https://doi.org/10.1177/0333102411423305
Smith JL (1985) Whence pseudotumor cerebri? J Clin Neuroophthalmol 5:55–56
Spacca B, Amasio ME, Giordano F, Mussa F, Busca G, Donati P, Genitori L (2009) Surgical management of congenital median perisellar transsphenoidal encephaloceles with an extracranial approach: a series of 6 cases. Neurosurgery 65:1140–1145; discussion 1145–1146. https://doi.org/10.1227/01.Neu.0000351780.23357.F5
Tam EK, Gilbert AL (2019) Spontaneous cerebrospinal fluid leak and idiopathic intracranial hypertension. Curr Opin Ophthalmol 30:467–471. https://doi.org/10.1097/icu.0000000000000603
Teachey W, Grayson J, Cho DY, Riley KO, Woodworth BA (2017) Intervention for elevated intracranial pressure improves success rate after repair of spontaneous cerebrospinal fluid leaks. Laryngoscope 127:2011–2016. https://doi.org/10.1002/lary.26612
Thanki S, Guerrero W, Mokin M (2022) Treatment of pseudotumor cerebri (sinus stenosis). Neurosurg Clin N Am 33:207–214. https://doi.org/10.1016/j.nec.2021.11.002
Tuță S (2022) Cerebral venous outflow implications in idiopathic intracranial hypertension-from physiopathology to treatment. Life (Basel) 12(6):854. https://doi.org/10.3390/life12060854
Wang EW, Vandergrift WA 3rd, Schlosser RJ (2011) Spontaneous CSF leaks. Otolaryngol Clin North Am 44(845–856):vii. https://doi.org/10.1016/j.otc.2011.06.018
Wang S, Tong X, Li X, Liu L, Liu Z, Mo D, Wang Y (2022) Association of post-intervention pressure gradient with symptom-free at 6 months in idiopathic intracranial hypertension with venous sinus stenosis treated by stenting. Interv Neuroradiol 15910199221095044. https://doi.org/10.1177/15910199221095044
Wang S, Tong X, Li X, Liu L, Liu Z, Mo D, Wang Y (2022) Comparison of microcatheter and pressure wire for venous sinus manometric evaluation of patients with idiopathic intracranial hypertension. Interv Neuroradiol 15910199221096679. https://doi.org/10.1177/15910199221096679
Woodworth BA, Prince A, Chiu AG, Cohen NA, Schlosser RJ, Bolger WE, Kennedy DW, Palmer JN (2008) Spontaneous CSF leaks: a paradigm for definitive repair and management of intracranial hypertension. Otolaryngol Head Neck Surg 138:715–720. https://doi.org/10.1016/j.otohns.2008.02.010
Youngerman BE, Kosty JA, Gerges MM, Tabaee A, Kacker A, Anand VK, Schwartz TH (2020) Acellular dermal matrix as an alternative to autologous fascia lata for skull base repair following extended endoscopic endonasal approaches. Acta Neurochir (Wien) 162:863–873. https://doi.org/10.1007/s00701-019-04200-z
Zhao K, Gu W, Liu C, Kong D, Zheng C, Chen W, Li X, Liang Y, Zhou H (2022) Advances in the understanding of the complex role of venous sinus stenosis in idiopathic intracranial hypertension. J Magn Reson Imaging. https://doi.org/10.1002/jmri.28177
Acknowledgements
The authors are grateful to Mr. Thom Graves for his skillful artwork.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tosi, U., Ramos, A., Rampichini, M. et al. Combined surgical repair and venous sinus stenting for patients with skull base encephaloceles secondary to dural venous sinus stenosis. Acta Neurochir 165, 2283–2292 (2023). https://doi.org/10.1007/s00701-023-05680-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05680-w