Abstract
Background
Diagnosis of idiopathic normal pressure hydrocephalus (iNPH) is based on clinical, radiological, and hydrodynamic data of cerebrospinal fluid (CSF) obtained by invasive methods such as lumbar infusion test, which is used to determine the resistance to CSF outflow (Rout). However, Rout has limitations, and its value as predictor of valve response is questioned. Other variables can be obtained by lumbar infusion test, such as the time to reach the plateau (TRP) and the slope until reaching the plateau (SRP). The objectives were to determine if SRP could be a predictor of response to ventriculoperitoneal shunt (VPS) and what variable (Rout versus SRP) would have greater predictive value.
Method
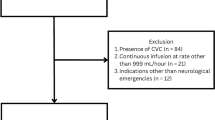
Patients with probable iNPH who underwent a lumbar infusion test and were indicated for a VPS were retrospectively studied. Two groups were established, responders and non-responders. Rout, TRP (period between the start of infusion until reaching the plateau measured in seconds) and SRP ((plateau pressure-opening pressure)/TRP) were obtained. For Rout and SRP, the receiver operating curves (ROC) with its areas under the curve (AUC) were calculated.
Results
One hundred ten patients were included, being 86 responders (78.20%). Shunt responders had a significantly greater Rout (17.02 (14.45–20.23) versus 13.34 (12.10–16.28) mmHg/ml/min, p = 0.002) and SRP (0.049 (0.043–0.054) versus 0.031 (0.026–0.036) mmHg/sec, p < 0.001) and smaller TRP (641.28 (584.83–697.73) versus 777.65 (654.03–901.27) sec, p = 0.028) than non-responders. The AUC for SRP was greater than the AUC for Rout (0.763 (95 % CI 0.655–0.871, p < 0.001) versus 0.673 (95 % CI 0.595–0.801, p = 0.008), respectively), but the differences were not significant (p = 0.180).
Conclusions
SRP could be considered predictor of response to VPS, and its accuracy tends to be better than Rout. So, this variable may be a useful tool to select shunt candidates among patients with probable iNPH.



Similar content being viewed by others
References
Adachi M, Kawanami T, Ohsima F, Kato T (2006) Upper midbrain profile sign and cingulate sulcus sign: MRI findings on sagittal images in idiopathic normal-pressure hydrocephalus, Alzheimer´s disease, and progressive supranuclear palsy. Radiat Med 24:568–572
Adams RD, Fisher CM, Hakim S, Ojemann RG, Sweet WH (1965) Symptomatic occult hydrocephalus with ‘normal’ cerebrospinal-fluid pressure. A treatable syndrome. N Engl J Med 273:117–126
Albeck MJ, Borgesen SE, Gjerris F, Schmidt JF, Sorensen PS (1991) Intracranial pressure and cerebrospinal fluid outflow conductance in healthy subjects. J Neurosurg 74:597–600
Boon AJ, Tans JT, Delwel EJ, Egeler-Peerdeman SM, Hanlo PW, Wurzar HA et al (1997) Dutch normal-pressure hydrocephalus study: prediction of outcome after shunting by resistance to outflow of cerebrospinal fluid. J Neurosurg 87(5):687–693
Boon AJ, Tans JT, Delwel EJ, Egeler-Peerdeman SM, Hanlo PW, Wurzer HA et al (2000) The Dutch normal-pressure hydrocephalus study. How to select patients for shunting? An analysis of four diagnostic criteria. Surg Neurol 53:201–207
Borgesen SE, Gjerris F (1982) The predictive value of conductance to outflow of CSF in normal pressure hydrocephalus. Brain 105:65–86
Cordero Tous N, Román Cutillas AM, Jorqués Infante AM, Olivares Granados G, Saura Rojas JE, Iáñez Velasco B et al (2013) Hidrocefalia crónica del adulto: diagnóstico, tratamiento y evolución Estudio prospectivo. Neurocirugia 24:93–101
Eide PK, Brean A (2010) Cerebrospinal fluid pulse pressure amplitude during lumbar infusion in idiopathic normal pressure hydrocephalus can predict response to shunting. Cerebrospinal Fluid Res 7:5–15
Eide PK, Due-Tonnessen B, Helseth E, Lundar T (2001) Assessment of intracranial pressure volume relationships in childhood: the lumbar infusion test versus intracranial pressure monitoring. Child’s Nerv Syst 17:382–390
Girdan E, Palandri G, Lazino G, Murad MH, Elder BD (2018) Outcomes and complications of different surgical treatments for idiopathic normal pressure hydrocephalus: a systematic review and meta-analysis. J Neurosurg 131(4):1024–1036
Hashimoto M, Ishikawa M, Mori E, Kuwana N (2010) Study of iNPH on neurological improvement (SINPHONI): diagnosis of idiopathic normal pressure hydrocephalus is supported by MRI-based scheme: a prospective cohort study. Cerebrospinal Fluid Res 7:18–27
Kahlon B, Sundbärg G, Rehncrona S (2002) Comparison between the lumbar infusion and CSF tap test to predict outcome after shunt surgery in suspected normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry 73:721–726
Kahlon B, Sundbarg G, Rehncrona S (2005) Lumbar infusion test in normal pressure hydrocephalus. Acta Neurol Scand 111:379–384
Kiefer M, Eymann R, Steudel WI (2006) Outcome predictors for normal-pressure hydrocephalus. Acta Neurochir Suppl 96:364–367
Malm J, Eklund A (2006) Idiopathic normal pressure hydrocephalus. Pract Neurol 6:14–27
Malm J, Jacobsson J, Birgander R, Eklund A (2011) Reference values for CSF outflow resistance and intracranial pressure in healthy elderly. Neurology 76:903–909
Marmarou A, Bergsneider M, Klinge P, Relkin N, Black PM (2005) The value of supplemental prognostic test for the preoperative assessment of idiopathic normal-pressure hydrocephalus. Neurosurgery 57(3 Suppl):S2–S17
Marmarou A, Young HF, Aygok GA, Sawauchi S, Tsuji O, Yamamoto T et al (2005) Diagnosis and management of idiopathic normal-pressure hydrocephalus: a prospective study in 151 patients. J Neurosurg 102:987–997
Mori E, Ishikawa M, Kato T, Kazui H, Miyake H, Miyajima M et al (2012) Guidelines for management of idiopathic normal pressure hydrocephalus: second edition. Neurol Med Chir (Tokyo) 52:775–809
Nkajima M, Yamada S, Miyajima M, Ishii K, Kuriyama N, Kazui H et al (2021) Guidelines for management of idiopathic normal pressure hydrocephalus (Third edition): endorsed by the Japanese Society of Normal Pressure Hydrocephalus. Neurol Med Chir (Tokio) 61(2):63–97
Otero-Rodríguez A, Arandia-Guzmán DA, García-Martín A, Torres-Carretero L, Garrido-Ruiz A, Sousa-Casasnovas P et al (2022) Prognostic value of pulse pressure amplitudes, time to reach the plateau and the slope obtained in the lumbar infusion test for the study if idiopathic normal pressure hydrocephalus. Neurocirugia 33(3):120–129
Otero-Rodriguez A, Sousa-Casasnovas P, Cruz-Terrón H, Arandia-Guzman DA, García-Martin A, Pascual-Argente D et al (2019) Utility of radiologic variables to predict the result of lumbar infusion test in the diagnosis of idiopathic normal pressure hydrocephalus. World Neurosurg 127:e957–e964
Qvarlander S, Lundkvist B, Koskines LD, Malm J, Eklund A (2013) Pulsatility in CSF dynamics: pathophysiology of idiopathic normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry 84:735–741
Skalickú P, Mládek A, Vlasák A, De Lacy P, Benes V, Bradác O (2020) Normal pressure hydrocephalus-an overview of pathophysiological mechanisms and diagnostic procedures. Neurosurg Rev 43:1451–1464
Sorteberg A, Eide PK, Fremming AD (2004) A prospective study on clinical effect of surgical treatment of normal pressure hydrocephalus: the value of hydrodynamic evaluation. Br J Neurosurg 18:149–157
Virhammar J, Laurell K, Cesarini KG, Larsson EM (2014) The callosal angle measured on MRI as a predictor of outcome in idiopathic normal-pressure hydrocephalus. J Neurosurg 120(1):178–184
Wang Z, Zhang Y, Hu F, Ding J, Wang X (2020) Pathogenesis and pathophysiology of idiopathic normal pressure hydrocephalus. CNS Neurosci Ther 26(12):1230–1240
Wikkelso C, Hellstrom P, Klinge PM, Tans JT (2013) The European iNPH Multicentre Study on the predictive values of resistance to CSF outflow and the CSF Tap Test in patients with idiopathic normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry 84:562–568
Acknowledgements
The authors would like to thank the operating theater nursing staff and porters for their help with the lumbar infusion tests. We would also like to thank Neuropicture™ developer Fernando Reviriego for making the changes suggested by our group to the software.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study was approved by our Institutional Review Board.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Otero-Rodriguez, A., Arandia-Guzman, D.A., Pascual-Argente, D. et al. Slope until reaching the plateau: a new predictor of valve response obtained by lumbar infusion test for idiopathic normal pressure hydrocephalus. Acta Neurochir 165, 2533–2539 (2023). https://doi.org/10.1007/s00701-023-05670-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05670-y