Abstract
Background
Isolated fourth ventricle (IFV) is a challenging entity to manage. In recent years, endoscopic treatment for aqueductoplasty has been on the rise. However, in patients with complex hydrocephalus and distorted ventricular system, its implementation can be complex.
Methods
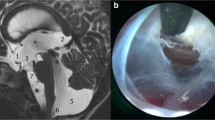
We present a 3-year-old patient with myelomeningocele and postnatal hydrocephalus treated by ventriculoperitoneal shunt. In follow-up, a progressive IFV and isolated lateral ventricle with symptoms of the posterior fossa developed. An endoscopic aqueductoplasty (EA) with panventricular stent plus septostomy guided with neuronavigation was decided due to the complexity of the ventricular system.
Conclusion
In IFV associated with complex hydrocephalus with distortion of the ventricular system, navigation can be of great help for planning and as a guide for performing EA.





Similar content being viewed by others
Abbreviations
- IFV :
-
Isolated fourth ventricle
- EA :
-
Endoscopic aqueductoplasty
- CT :
-
Computer tomography
- MRI :
-
Magnetic resonance imaging
- EVD :
-
External ventricular drain
References
Fritsch MJ, Schroeder HW (2013) Endoscopic aqueductoplasty and stenting. World Neurosurg 79(2 Suppl):S20.e15–S20.e18
Gomar-Alba M, Parrón-Carreño T, Guil-Ibáñez JJ, Vargas-López AJ, Castelló-Ruiz MJ, García-Pérez F, Masegosa-González J (2023) Role of endoscopic aqueductoplasty with panventricular stent in the treatment of isolated fourth ventricle during shunt malfunction: 2-dimensional operative video. Oper Neurosurg (Hagerstown). https://doi.org/10.1227/ons.0000000000000682 Advance online publication
Harter DH (2004) Management strategies for treatment of the trapped fourth ventricle. Childs Nerv Syst 20(10):710–716
Longatti P, Fiorindi A, Perin A, Martinuzzi A (2007) Endoscopic anatomy of the cerebral aqueduct. Neurosurgery 61(3 Suppl):1–6
Panagopoulos D, Karydakis P, Themistocleous M (2021) The entity of the trapped fourth ventricle: a review of its history, pathophysiology, and treatment options. Brain Circ 7(3):147–158
Pomeraniec IJ, Ksendzovsky A, Ellis S, Roberts SE, Jane JA Jr (2016) Frequency and long-term follow-up of trapped fourth ventricle following neonatal posthemorrhagic hydrocephalus. J Neurosurg Pediatr 17(5):552–557
Rekate HL (2005) Endoscopic fourth ventricular aqueductoplasty. J Neurosurg 103(5):773–775
Sagan LM, Kojder I, Poncyljusz W (2006) Endoscopic aqueductal stent placement for the treatment of a trapped fourth ventricle. J Neurosurg 105(4 Suppl):275–280
Schroeder HW, Gaab MR (1999) Endoscopic aqueductoplasty: technique and results. Neurosurgery 45(3):508–518
Schulz M, Goelz L, Spors B, Haberl H, Thomale UW (2012) Endoscopic treatment of isolated fourth ventricle: clinical and radiological outcome. Neurosurgery 70(4):847–859
Tirado-Caballero J, Rivero-Garvia M, Moreno-Madueño G, Gómez-González E, Márquez-Rivas J (2021) Cranial expansion and aqueductoplasty for combined isolated fourth ventricle and slit-ventricle syndrome: a surgical alternative. Childs Nerv Syst 37(3):885–894
Tirado-Caballero J, Herreria-Franco J, Rivero-Garvía M, Moreno-Madueño G, Mayorga-Buiza MJ, Marquez-Rivas J (2021) Technical nuances in neuroendoscopic lavage for germinal matrix hemorrhage in preterm infants: twenty tips and pearls after more than one hundred procedures. Pediatr Neurosurg 56(4):392–400. https://doi.org/10.1159/000516183
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in the studies involving human participants were in accordance with ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standard.
Consent to participate and consent for publication
Informed consent to participate and consent for publication was obtained from the patient included in this report.
Conflict of interest
The authors declare no competing interests.
Additional information
Key points
Determine the indications for surgery. Patients with clinical symptoms should undergo surgery. In cases where the patient is asymptomatic but has radiological progression, risk/benefit assessment is necessary.
Establish the approach route. If an endoscopic aqueductoplasty is being considered, the patient must have a ventricular size large enough to accommodate the system. Otherwise, alternatives such as EVD placement or cranial expansion may be considered.
Study preoperative images and develop a surgical plan by identifying limiting structures and the best surgical route.
In complex anatomies, consider the use of neuronavigation.
Explain to the patient and family the possibility of transient neurological alterations, particularly in eye mobility.
Knowledge of ventricular anatomy and experience in intraventricular endoscopy are crucial to obtain good outcomes.
The use of stents appears to show a lower rate of restenosis in the literature.
A proper technique for closing the cortical-subcortical tract is ideal to avoid the risk of cerebrospinal fluid leak.
Periodic follow-up with MRI is recommended for patients. We have protocolized the performance of a control magnetic resonance imaging before discharge, another 1 month after the procedure, at 3 months, 6 months, and then annually. During the interpretation of these images, we investigate possible signs of system failure (e.g., signs of hyperdrainage) and combine it with the information provided by the parents about the patient’s neurological (cognitive, school, motor, etc.) evolution.
In patients with shunts and a history of obstructive hydrocephalus, consideration should be given to endoscopic third ventriculostomy to remove the ventricular shunt.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Guil-Ibáñez, J.J., Parrón-Carreño, T., Gomar-Alba, M. et al. Neuronavigated endoscopic aqueductoplasty with panventricular stent plus septostomy for isolated fourth ventricle in complex hydrocephalus and syringomyelia associated with myelomeningocele: how I do it. Acta Neurochir 165, 2333–2338 (2023). https://doi.org/10.1007/s00701-023-05649-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05649-9