Abstract
Background
Cerebral metastases (CM) are the most common intracranial tumors; several studies have underlined the fundamental role of neurosurgical lesion removal.
Method
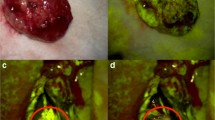
We describe the surgical resection of a left frontal single metastasis. We attempted to achieve a radical resection under the intraoperative guidance of fluorescein, with the aid of intraoperative neurological monitoring. This technique can be applied to each contrast enhancing, intra-axial, infiltrative lesion.
Conclusion
Fluorescein-guided surgery is a valuable tool in CM surgery to increase the rate of resection; further prospective evaluation of the role of fluorescein in this field is in planning, aiming to study the prognostic impact.





Similar content being viewed by others
Data availability
The data presented in this study are available on request from the authors.
Abbreviations
- BBB:
-
Blood-brain barrier
- CM:
-
Cerebral metastases
- CUSA:
-
Cavitron ultrasound aspirator
- SF:
-
Sodium fluorescein
- TcMEP:
-
Transcranial motor evoked potentials
References
Acerbi F, Broggi M, Broggi G, Ferroli P (2015) What is the best timing for fluorescein injection during surgical removal of high-grade gliomas? Acta Neurochir (Wien). https://doi.org/10.1007/s00701-015-2455-z
Belykh E, Shaffer KV, Lin C, Byvaltsev VA, Preul MC (2020) Blood-brain barrier, blood-brain fluorescence-guided neurosurgical oncology: delivering optical labels to brain tumors. Front Oncol. https://doi.org/10.3389/fonc.2020.00739
Berghoff AS, Rajky O, Winkler F, Bartsch R, Furtner J, Hainfellner JA, Goodman SL, Weller M, Schittenhelm J, Preusser M (2013) Invasion patterns in brain metastases of solid cancers. Neuro Oncol. https://doi.org/10.1093/neuonc/not112
Cagney DN, Martin AM, Catalano PJ et al (2017) Incidence and prognosis of patients with brain metastases at diagnosis of systemic malignancy: a population-based study. Neuro Oncol. https://doi.org/10.1093/neuonc/nox077
Cavallo C, De Laurentis C, Vetrano IG, Falco J, Broggi M, Schiariti M, Ferroli P, Acerbi F (2018) The utilization of fluorescein in brain tumor surgery: a systematic review. J Neurosurg Sci. https://doi.org/10.23736/S0390-5616.18.04480-6
Falco J, Cavallo C, Vetrano IG, de Laurentis C, Siozos L, Schiariti M, Broggi M, Ferroli P, Acerbi F (2019) Fluorescein application in cranial and spinal tumors enhancing at preoperative MRI and operated with a dedicated filter on the surgical microscope: preliminary results in 279 patients enrolled in the FLUOCERTUM prospective study. Front Surg. https://doi.org/10.3389/fsurg.2019.00049
Ferguson SD, Wagner KM, Prabhu SS, McAleer MF, McCutcheon IE, Sawaya R (2017) Neurosurgical management of brain metastases. Clin Exp Metastasis. https://doi.org/10.1007/s10585-017-9860-z
Höhne J, Hohenberger C, Proescholdt M, Riemenschneider MJ, Wendl C, Brawanski A, Schebesch KM (2017) Fluorescein sodium-guided resection of cerebral metastases—an update. Acta Neurochir (Wien). https://doi.org/10.1007/s00701-016-3054-3
Kavouridis VK, Harary M, Hulsbergen AFC, Lo YT, Reardon DA, Aizer AA, Iorgulescu JB, Smith TR (2019) Survival and prognostic factors in surgically treated brain metastases. J Neurooncol. https://doi.org/10.1007/s11060-019-03171-6
Kofoed MS, Pedersen CB, Schulz MK, Kristensen BW, Hansen RW, Markovic L, Halle B, Poulsen FR (2022) Fluorescein-guided resection of cerebral metastases is associated with greater tumor resection. Acta Neurochir (Wien). https://doi.org/10.1007/s00701-021-04796-1
Acknowledgements
The authors thank all the neurophysiologists and technicians for their valuable work during eloquent tumor removal and, in particular, Paola Lanteri and Valentina Catanzaro for their contribution in this specific case and during manuscript production.
Funding
This study was partially supported by the Associazione Paolo Zorzi per le Neuroscienze, ONLUS and by the Italian Ministry of Health (RRC).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Francesco Acerbi received honoraria from Carl Zeiss Meditec for lectures in International Meetings.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
(1) Select for neurosurgery the correct patient after a multidisciplinary discussion with a shared therapeutic rationale.
(2) Strong collaboration with neurophysiologists during surgical procedure.
(3) Fluorescein injection at the standardized low dose of 5 mg/kg, immediately upon completion of general anesthesia; take care to discuss with the patient regarding the advantages of this dye and the related low risks.
(4) Use neuronavigation to tailor surgical approach and craniotomy.
(5) Start from enucleation and en-bloc removal of the lesion.
(6) Prosecute by aspirating the infiltrative micro-metastases, detectable with YELLOW560 filter activated.
(7) Indocyanine green video-angiography could be safely performed to study major vessels: both dyes are compatible.
(8) Perform hemostasis under white-light illumination after arterial pressure challenge.
(9) Finally check resection borders comparing white light and YELLOW560 visualization.
(10) An early postoperative MRI is mandatory, and an oncological follow-up is necessary to guarantee the adequate path of care.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 90705 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Acerbi, F., Broggi, M., Ferroli, P. et al. Fluorescein-guided resection of a left frontal pre-rolandic cerebral metastasis: how I do it. Acta Neurochir 165, 2519–2524 (2023). https://doi.org/10.1007/s00701-023-05635-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05635-1