Abstract
Background
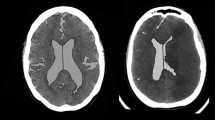
The effect of posterior cranial fossa stroke on changes in cerebral volume is not known. We assessed cerebral volume changes in patients with acute posterior fossa stroke using CT scans, and looked for risk factors for cerebral atrophy.
Methods
Patients with cerebellar or brainstem hemorrhage/infarction admitted to the ICU, and who underwent at least two subsequent inpatient head CT scans during hospitalization were included (n = 60). The cerebral volume was estimated using an automatic segmentation method. Patients with cerebral volume reduction > 0% from the first to the last scan were defined as the “cerebral atrophy group (n = 47),” and those with ≤ 0% were defined as the “no cerebral atrophy group (n = 13).”
Results
The cerebral atrophy group showed a significant decrease in cerebral volume (first CT scan: 0.974 ± 0.109 L vs. last CT scan: 0.927 ± 0.104 L, P < 0.001). The mean percentage change in cerebral volume between CT scans in the cerebral atrophy group was –4.7%, equivalent to a cerebral volume of 46.8 cm3, over a median of 17 days. The proportions of cases with a history of hypertension, diabetes mellitus, and median time on mechanical ventilation were significantly higher in the cerebral atrophy group than in the no cerebral atrophy group.
Conclusions
Many ICU patients with posterior cranial fossa stroke showed signs of cerebral atrophy. Those with rapidly progressive cerebral atrophy were more likely to have a history of hypertension or diabetes mellitus and required prolonged ventilation.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, RN, upon reasonable request.
Abbreviations
- CSF:
-
Cerebrospinal fluid
- DM:
-
Diabetes mellitus
- GCS:
-
Glasgow Coma Scale
- GM:
-
Gray matter
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- MNI:
-
Montreal Neurological Institute
- mRS:
-
Modified Rankin Scale
- PEEP:
-
Positive end-expiratory pressure
- SPECT:
-
Single-photon emission computed tomography
- SPM:
-
Statistical parametric mapping
- WM:
-
White matter
References
Adduru V, Baum SA, Zhang C, Helguera M, Zand R, Lichtenstein M, Griessenauer CJ, Michael AM (2020) A method to estimate brain volume from head CT images and application to detect brain atrophy in Alzheimer disease. AJNR Am J Neuroradiol 41:224–230
Andersen SM, Rapcsak SZ, Beeson PM (2010) Cost function masking during normalization of brains with focal lesions: still a necessity? Neuroimage 53:78–84
Ashburner J, Friston KJ (2005) Unified segmentation. Neuroimage 26:839–851
Bae HJ, Lee J, Park JM, Kwon O, Koo JS, Kim BK, Pandey DK (2007) Risk factors of intracranial cerebral atherosclerosis among asymptomatics. Cerebrovasc Dis 24:355–360
Baron JC, Bousser MG, Comar D, Castaigne P (1981) “Crossed cerebellar diaschisis” in human supratentorial brain infarction. Trans Am Neurol Assoc 105:459–461
Brett M, Leff AP, Rorden C, Ashburner J (2001) Spatial normalization of brain images with focal lesions using cost function masking. Neuroimage 14:486–500
Chen H, Menon DK, Kavanagh BP (2019) Impact of altered airway pressure on intracranial pressure, perfusion, and oxygenation: a narrative review. Crit Care Med 47:254–263
Committee for Stroke Guideline 2009, the Japan Stroke Society (2009) Japan Stroke Society Guideline 2009 for the Treatment of Stroke. Kyowa-Kikaku Ltd, Tokyo (in Japanese)
Committee for Stroke Guideline 2015, the Japan Stroke Society (2015) Japan Stroke Society Guideline 2015 for the Treatment of Stroke. Kyowa-Kikaku Ltd, Tokyo (in Japanese)
Craig BT, Olsen C, Mah S, Carlson HL, Wei XC, Kirton A (2019) Crossed cerebellar atrophy in perinatal stroke. Stroke. https://doi.org/10.1161/STROKEAHA118022423
Evered L, Silbert B, Scott DA, Zetterberg H, Blennow K (2018) Association of changes in plasma neurofilament light and tau levels with anesthesia and surgery: results from the CAPACITY and ARCADIAN Studies. JAMA Neurol 75:542–547
Fazekas F, Payer F, Valetitsch H, Schmidt R, Flooh E (1993) Brain stem infarction and diaschisis. a spect cerebral perfusion study. Stroke 24:1162–1166
Georgiadis D, Schwarz S, Baumgartner RW, Veltkamp R, Schwab S (2001) Influence of positive end-expiratory pressure on intracranial pressure and cerebral perfusion pressure in patients with acute stroke. Stroke 32:2088–2092
Giorgio A, De Stefano N (2013) Clinical use of brain volumetry. J Magn Reson Imaging 37:1–14
Hammers A, Allom R, Koepp MJ, Free SL, Myers R, Lemieux L, Mitchell TN, Brooks DJ, Duncan JS (2003) Three-dimensional maximum probability atlas of the human brain, with particular reference to the temporal lobe. Hum Brain Mapp 19:224–247
Hocker S, Nagarajan E, Rabinstein AA, Hanson D, Britton JW (2016) Progressive brain atrophy in super-refractory status epilepticus. JAMA Neurol 73:1201–1207
Hoffmann M, Watts A (1998) Cognitive dysfunction in isolated brainstem stroke: a neuropsychological and SPECT study. J Stroke Cerebrovasc Dis 7:24–31
Horstmann A, Frisch S, Jentzsch RT, Muller K, Villringer A, Schroeter ML (2010) Resuscitating the heart but losing the brain: brain atrophy in the aftermath of cardiac arrest. Neurology 74:306–312
Huang HW, Guo MH, Lin RJ, Chen YL, Luo Q, Zhang Y, Wong KS (2007) Prevalence and risk factors of middle cerebral artery stenosis in asymptomatic residents in Rongqi County, Guangdong. Cerebrovasc Dis 24:111–115
Irimia A, Maher AS, Rostowsky KA, Chowdhury NF, Hwang DH, Law EM (2019) Brain segmentation from computed tomography of healthy aging and geriatric concussion at variable spatial resolutions. Front Neuroinform 13:9
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Lahiri S, Regis GC, Koronyo Y, Fuchs DT, Sheyn J, Kim EH, Mastali M, Van Eyk JE, Rajput PS, Lyden PD, Black KL, Ely EW, Jones HD, Koronyo-Hamaoui M (2019) Acute neuropathological consequences of short-term mechanical ventilation in wild-type and Alzheimer’s disease mice. Crit Care 23:63
Marchi NA, Ramponi C, Hirotsu C, Haba-Rubio J, Lutti A, Preisig M, Marques-Vidal P, Vollenweider P, Kherif F, Heinzer R, Draganski B (2020) Mean oxygen saturation during sleep is related to specific brain atrophy pattern. Ann Neurol 87:921–930
Miyamoto S, Ogasawara K, Kuroda S, Itabashi R, Toyoda K, Itoh Y, Iguchi Y, Shiokawa Y, Takagi Y, Ohtsuki T, Kinouchi H, Okada Y, Takahashi JC, Nakase H, Kakuda W (2022) Japan Stroke Society Guideline 2021 for the Treatment of Stroke. Int J Stroke 17:1039–1049
Nakae R, Sekine T, Tagami T, Murai Y, Kodani E, Warnock G, Sato H, Morita A, Yokota H, Yokobori S (2021) Rapidly progressive brain atrophy in septic ICU patients: a retrospective descriptive study using semiautomatic CT volumetry. Crit Care 25:411
Nyquist P, Stevens RD, Mirski MA (2008) Neurologic injury and mechanical ventilation. Neurocrit Care 9:400–408
Paulson OB, Strandgaard S, Edvinsson L (1990) Cerebral autoregulation. Cerebrovasc Brain Metab Rev 2:161–192
Prassopoulos P, Cavouras D, Golfinopoulos S, Evlogias N, Theodoropoulos V, Panagiotou J (1996) Quantitative assessment of cerebral atrophy during and after treatment in children with acute lymphoblastic leukemia. Invest Radiol 31:749–754
Qureshi AI, Caplan LR (2014) Intracranial atherosclerosis. Lancet 383:984–998
Rorden C, Bonilha L, Fridriksson J, Bender B, Karnath HO (2012) Age-specific CT and MRI templates for spatial normalization. Neuroimage 61:957–965
Rousseaux M, Steinling M (1992) Crossed hemispheric diaschisis in unilateral cerebellar lesions. Stroke 23:511–514
Rousseaux M, Steinling M, Mazingue A, Benaim C, Froger J (1995) Cerebral blood flow in lateral medullary infarcts. Stroke 26:1404–1408
Sasannejad C, Ely EW, Lahiri S (2019) Long-term cognitive impairment after acute respiratory distress syndrome: a review of clinical impact and pathophysiological mechanisms. Crit Care 23:352
Steiner T, Mendoza G, De Georgia M, Schellinger P, Holle R, Hacke W (1997) Prognosis of stroke patients requiring mechanical ventilation in a neurological critical care unit. Stroke 28:711–715
Strandgaard S (1991) Cerebral blood flow in the elderly: impact of hypertension and antihypertensive treatment. Cardiovasc Drugs Ther 4(Suppl 6):1217–1221
Tien RD, Ashdown BC (1992) Crossed cerebellar diaschisis and crossed cerebellar atrophy: correlation of MR findings, clinical symptoms, and supratentorial diseases in 26 patients. AJR Am J Roentgenol 158:1155–1159
Tsuda Y, Ayada Y, Izumi Y, Ichihara S, Hosomi N, Ohkawa M, Matsuo H (1995) Cerebellar diaschisis in pontine infarctions: a report of five cases. Eur J Nucl Med 22:413–418
Uehara T, Tabuchi M, Mori E (2005) Risk factors for occlusive lesions of intracranial arteries in stroke-free Japanese. Eur J Neurol 12:218–222
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Acknowledgements
We thank Libby Cone, MD, MA, from Dmed (www.dmed.co.jp) for editing drafts of this manuscript.
Author information
Authors and Affiliations
Contributions
Conception and design: YM, RN. Acquisition of data: YM, TS, EK. Analysis and interpretation of data: YM, RN, YI, TT, YM. Drafting the article: YM, RN, TS. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: RN. Statistical analysis: YM, RN. Study supervision: GW, KS, SY.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethics Committee of Nippon Medical School Hospital and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The Institutional Review Board of Nippon Medical School Hospital approved this study (B-2022–552) and waived the need for informed consent due to the observational nature of the study.
Conflict of interest
One author (Geoffrey Warnock) is an employee of PMOD Technologies Ltd. Only PMOD non-employees had control of inclusion of data and other information.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Matsumoto, Y., Nakae, R., Sekine, T. et al. Rapidly progressive cerebral atrophy following a posterior cranial fossa stroke: Assessment with semiautomatic CT volumetry. Acta Neurochir 165, 1575–1584 (2023). https://doi.org/10.1007/s00701-023-05609-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05609-3