Abstract
Introduction
At present, selective amygdalohippocampectomy (SAH) has become popular in the treatment of drug-resistant mesial temporal lobe epilepsy (TLE). However, there is still an ongoing discussion about the advantages and disadvantages of this approach.
Methods
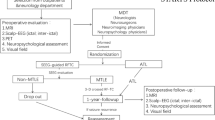
The study included a consecutive series of 43 adult patients with drug-resistant TLE, involving 24 women and 19 men (1.8/1). Surgeries were performed at the Burdenko Neurosurgery Center from 2016 to 2019. To perform subtemporal SAH through the burr hole with the diameter of 14 mm, we used two types of approaches: preauricular, 25 cases, and supra-auricular, 18 cases. The follow-up ranged from 36 to 78 months (median 59 months). One patient died 16 months after surgery (accident).
Results
By the third year after surgery, Engel I outcome was achieved in 80.9% (34 cases) of cases and Engel II in 4 (9.5%) and Engel III and Engel IV in 4 (9.6%) cases. Among the patients with Engel I outcomes, anticonvulsant therapy was completed in 15 (44.1%), and doses were reduced in 17 (50%) cases. Verbal and delayed verbal memory decreased after surgery in 38.5% and 46.1%, respectively. Verbal memory was mainly affected by preauricular approach in comparison with supra-auricular (p = 0.041). In 15 (51.7%) cases, minimal visual field defects were detected in the upper quadrant. At the same time, visual field defects did not extend into the lower quadrant and inside the 20° of the upper affected quadrant in any case.
Conclusions
Burr hole microsurgical subtemporal SAH is an effective surgical procedure for drug-resistant TLE. It involves minimal risks of loss of visual field within the 20° of the upper quadrant. Supra-auricular approach, compared to preauricular, results in a reduction in the incidence of upper quadrant hemianopia and is associated with a lower risk of verbal memory impairment.





Similar content being viewed by others
References
Blumer D, Wakhlu S, Davies K, Hermann B (1998) Psychiatric outcome of temporal lobectomy for epilepsy: incidence and treatment of psychiatric complications. Epilepsia 39:478–486. https://doi.org/10.1111/j.1528-1157.1998.tb01409.x
Boling W (2010) Minimal access keyhole surgery for mesial temporal lobe epilepsy. J Clin Neurosci 17:1180–1184. https://doi.org/10.1016/j.jocn.2010.01.030
Bujarski KA, Hirashima F, Roberts DW, Jobst BC, Gilbert KL, Roth RM, Flashman LA, McDonald BC, Saykin AJ, Scott RC, Dinnerstein E, Preston J, Williamson PD, Thadani VM (2013) Long-term seizure, cognitive, and psychiatric outcome following trans-middle temporal gyrus amygdalohippocampectomy and standard temporal lobectomy. J Neurosurg 119:16–23. https://doi.org/10.3171/2013.3.jns12714
Cendes F, Dubeau F, Olivier A, Cukiert A, Andermann E, Quesney LF, Andermann F (1993) Increased neocortical spiking and surgical outcome after selective amygdalo-hippocampectomy. Epilepsy Res 16:195–206. https://doi.org/10.1016/0920-1211(93)90080-q
Chen X, Sure U, Haag A, Knake S, Fritsch B, Müller HH, Becker R, Oertel WH, Bertalanffy H, Hamer HM, Rosenow F (2006) Predictive value of electrocorticography in epilepsy patients with unilateral hippocampal sclerosis undergoing selective amygdalohippocampectomy. Neurosurg Rev 29:108–113. https://doi.org/10.1007/s10143-005-0002-8
Clusmann H, Schramm J, Kral T, Helmstaedter C, Ostertun B, Fimmers R, Haun D, Elger CE (2002) Prognostic factors and outcome after different types of resection for temporal lobe epilepsy. J Neurosurg 97:1131–1141. https://doi.org/10.3171/jns.2002.97.5.1131
Delev D, Wabbels B, Schramm J, Nelles M, Elger CE, von Lehe M, Clusmann H, Grote A (2016) Vision after trans-sylvian or temporobasal selective amygdalohippocampectomy: a prospective randomised trial. Acta Neurochir 158:1757–1765. https://doi.org/10.1007/s00701-016-2860-y
Duckworth EA, Vale FL (2008) Trephine epilepsy surgery: the inferior temporal gyrus approach. Neurosurg 63:156-ONSI160. https://doi.org/10.1227/01.neu.0000335030.85402.5f
Ebeling U, Reulen HJ (1988) Neurosurgical topography of the optic radiation in the temporal lobe. Acta Neurochir 92:29–36. https://doi.org/10.1007/bf01401969
Eliseeva NM, Pitskhelauri DI, Serova NK, Kudieva ES (2019) Visual field disorder after surgery of temporal lobe epilepsy associated to hippocampus sclerosis. Zh Vopr Neirokhir Im N N Burdenko 83:14–20. https://doi.org/10.17116/neiro20198305114
European Commission Directive. 2009/112/EC. https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32009L0132&from=EN. Accessed September 30, 2019
Flores JAC, Sanders FH, Figueiredo EG, Teixeira MJ (2017) Transtemporal amygdalohippocampectomy: a novel minimally-invasive technique with optimal clinical results and low cost. Arq Neuropsiquiatr 75:801–808. https://doi.org/10.1590/0004-282x20170141
Helmstaedter C (2013) Cognitive outcomes of different surgical approaches in temporal lobe epilepsy. Epileptic Disord 15:221–239. https://doi.org/10.1684/epd.2013.0587
Herlopian A, Shihabuddin B (2017) Predictive value of electrocorticography in patients with mesial temporal lobe epilepsy undergoing selective amygdalohippocampectomy. J Clin Neurophysiol 34:370–374. https://doi.org/10.1097/wnp.0000000000000376
Hill SW, Gale SD, Pearson C, Smith K (2012) Neuropsychological outcome following minimal access subtemporal selective amygdalohippocampectomy. Seizure 21:353–360. https://doi.org/10.1016/j.seizure.2012.03.002
Hori T, Tabuchi S, Kurosaki M, Kondo S, Takenobu A, Watanabe T (1993) Subtemporal amygdalohippocampectomy for treating medically intractable temporal lobe epilepsy. Neurosurg 33:50–56
Hori T, Yamane F, Ochiai T, Kondo S, Shimizu S, Ishii K, Miyata H (2007) Selective subtemporal amygdalohippocampectomy for refractory temporal lobe epilepsy: operative and neuropsychological outcomes. J Neurosurg 106:134–141. https://doi.org/10.3171/jns.2007.106.1.134
Lacruz ME, Alarcón G, Akanuma N, Lum FC, Kissani N, Koutroumanidis M, Adachi N, Binnie CD, Polkey CE, Morris RG (2004) Neuropsychological effects associated with temporal lobectomy and amygdalohippocampectomy depending on Wada test failure. J Neurol Neurosurg Psychiatry 75:600–607. https://doi.org/10.1136/jnnp.2003.020248
Lee T, Mackenzie RA, Walker AJ, Matheson JM, Sachdev P (1997) Effects of left temporal lobectomy and amygdalohippocampectomy on memory. J Clin Neurosci 4:314–319. https://doi.org/10.1016/s0967-5868(97)90098-9
Little AS, Smith KA, Kirlin K, Baxter LC, Chung S, Maganti R, Treiman DM (2009) Modifications to the subtemporal selective amygdalohippocampectomy using a minimal-access technique: seizure and neuropsychological outcomes. J Neurosurg 111:1263–1274. https://doi.org/10.3171/2008.10.17673
Mansouri A, Fallah A (2014) Neurocognitive and seizure outcomes of selective amygdalohippocampectomy versus anterior temporal lobectomy for mesial temporal lobe epilepsy. Epilepsy Res Treat 2014:306382. https://doi.org/10.1155/2014/306382
Niemeyer P (1958) The transventricular amygdalohippocampectomy in temporal lobe epilepsy. Temporal lobe epilepsy
Park TS, Bourgeois BF, Silbergeld DL, Dodson WE (1996) Subtemporal transparahippocampal amygdalohippocampectomy for surgical treatment of mesial temporal lobe epilepsy. Technical note. J Neurosurg 85:1172–1176. https://doi.org/10.3171/jns.1996.85.6.1172
Pitskhelauri DI, Konovalov AN, Shekutev GA, Rojnin NB, Kachkov IA, Samborskiy DY, Sanikidze AZ, Kopachev DN (2014) A novel device for hands-free positioning and adjustment of the surgical microscope. J Neurosurg 121:161–164. https://doi.org/10.3171/2014.3.jns12578
Pitskhelauri D, Konovalov A, Kudieva E, Bykanov A, Pronin I, Eliseeva N, Melnikova-Pitskhelauri T, Melikyan A, Sanikidze A (2019) Burr hole microsurgery for intracranial tumors and mesial temporal lobe epilepsy: results of 200 consecutive operations. World Neurosurg 126:e1257–e1267. https://doi.org/10.1016/j.wneu.2019.02.239
Pitskhelauri DI, Kudieva ES, Melikyan AG, Vlasov PA, Kamenetskaya MI, Zaitsev OS, Kozlova AB, Eliseeva NM, Shishkina LV, Danilov GV, Nagorskaya IA, Sanikidze AZ, Melnikova-Pitskhelauri TV, Pronin IN, Konovalov AN (2021) Surgical treatment of drug-resistant epilepsy following hippocampal sclerosis. Zh Vopr Neirokhir Im N N Burdenko 85:31–40. https://doi.org/10.17116/neiro20218505131
Sajko T, Skoro I, Rotim K (2013) How I do it - selective amygdalohippocampectomy via subtemporal approach. Acta Neurochir 155:2381–2387. https://doi.org/10.1007/s00701-013-1846-2
Schmeiser B, Wagner K, Schulze-Bonhage A, Mader I, Wendling AS, Steinhoff BJ, Prinz M, Scheiwe C, Weyerbrock A, Zentner J (2017) Surgical treatment of mesiotemporal lobe epilepsy: which approach is favorable? Neurosurgery 81:992–1004. https://doi.org/10.1093/neuros/nyx138
Schmeiser B, Daniel M, Kogias E, Böhringer D, Egger K, Yang S, Foit NA, Schulze-Bonhage A, Steinhoff BJ, Zentner J, Lagrèze WA, Gross NJ (2017) Visual field defects following different resective procedures for mesiotemporal lobe epilepsy. Epilepsy Behav 76:39–45. https://doi.org/10.1016/j.yebeh.2017.08.037
Schramm J, Clusmann H (2008) The surgery of epilepsy. Neurosurgery 62 Suppl 2:463–481; discussion 481. https://doi.org/10.1227/01.neu.0000316250.69898.23
Sincoff EH, Tan Y, Abdulrauf SI (2004) White matter fiber dissection of the optic radiations of the temporal lobe and implications for surgical approaches to the temporal horn. J Neurosurg 101:739–746. https://doi.org/10.3171/jns.2004.101.5.0739
Uda T, Morino M, Minami N, Matsumoto T, Uchida T, Kamei T (2015) Abnormal discharges from the temporal neocortex after selective amygdalohippocampectomy and seizure outcomes. J Clin Neurosci 22:1797–1801. https://doi.org/10.1016/j.jocn.2015.03.063
von Rhein B, Nelles M, Urbach H, Von Lehe M, Schramm J, Helmstaedter C (2012) Neuropsychological outcome after selective amygdalohippocampectomy: subtemporal versus transsylvian approach. J Neurol Neurosurg Psychiatry 83:887–893. https://doi.org/10.1136/jnnp-2011-302025
Wendling AS, Hirsch E, Wisniewski I, Davanture C, Ofer I, Zentner J, Bilic S, Scholly J, Staack AM, Valenti MP, Schulze-Bonhage A, Kehrli P, Steinhoff BJ (2013) Selective amygdalohippocampectomy versus standard temporal lobectomy in patients with mesial temporal lobe epilepsy and unilateral hippocampal sclerosis. Epilepsy Res 104:94–104. https://doi.org/10.1016/j.eplepsyres.2012.09.007
Wrench JM, Wilson SJ, O’Shea MF, Reutens DC (2009) Characterising de novo depression after epilepsy surgery. Epilepsy Res 83:81–88. https://doi.org/10.1016/j.eplepsyres.2008.09.007
Yang PF, Zhang HJ, Pei JS, Lin Q, Mei Z, Chen ZQ, Jia YZ, Zhong ZH, Zheng ZY (2016) Neuropsychological outcomes of subtemporal selective amygdalohippocampectomy via a small craniotomy. J Neurosurg 125:67–74. https://doi.org/10.3171/2015.6.jns1583
Yaşargil MG, Teddy PJ, Roth P (1985) Selective amygdalo-hippocampectomy. Operative anatomy and surgical technique. Adv Tech Stand Neurosurg 12:93–123. https://doi.org/10.1007/978-3-7091-7008-3_2
Yaşargil MG, Krayenbühl N, Roth P, Hsu SP, Yaşargil DC (2010) The selective amygdalohippocampectomy for intractable temporal limbic seizures. J Neurosurg 112:168–185. https://doi.org/10.3171/2008.12.jns081112
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee of Burdenko Neurosurgery Institute and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors have no personal, financial, or institutional interest in any of the drugs and materials, described in this article. Dr. Pitskhelauri is the inventor of the Mari device and has ownership in Tolikety Co., Ltd., the company that manufactures the Mari device.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Functional Neurosurgery – Epilepsy
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 82865 KB)
Supplementary file2 (MP4 76494 KB)
Supplementary file3 (MP4 69490 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pitskhelauri, D., Kudieva, E., Vlasov, P. et al. Burr hole microsurgical subtemporal selective amygdalohippocampectomy. Acta Neurochir 165, 1215–1226 (2023). https://doi.org/10.1007/s00701-023-05536-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05536-3