Abstract
Background
No studies have examined the impact of body mass index (BMI) on newer Patient-Reported Outcomes Measurement Information System (PROMIS) outcomes in patients undergoing lumbar decompression (LD).
Methods
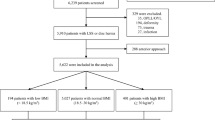
Patients undergoing LD with preoperative PROMIS measures were stratified into four cohorts: normal (18.5 ≤ BMI < 25 kg/m2), overweight (25 ≤ BMI < 30 kg/m2), obese I (30 ≤ BMI < 35 kg/m2), and obese II–III (BMI ≥ 35 kg/m2). Demographics, perioperative characteristics, and patient-reported outcomes (PROs) were obtained. PROs of PROMIS Physical Function (PROMIS-PF), PROMIS Anxiety (PROMIS-A), PROMIS Pain Interference (PROMIS-PI), PROMIS Sleep Disturbance (PROMIS-SD), Patient Health Questionnaire-9 (PHQ-9), Visual Analog Scale (VAS) Back Pain (VAS-BP), VAS Leg Pain (VAS-LP), and Oswestry Disability Index (ODI) were collected at preoperative and up to 2-year postoperative time points. Minimum clinically important difference (MCID) achievement was determined through comparison of previously established values. Comparison between cohorts were determined through inferential statistics.
Results
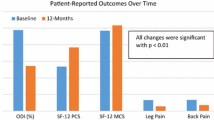
A total of 473 patients were identified, with stratification of 125 patients in the normal cohort, 161 in the overweight cohort, 101 in the obese I cohort, and 87 in the obese II–III cohort. Mean postoperative follow-up time was 13.51 ± 8.72 months. Higher BMI patients had higher operative times, longer postoperative length of stay, and greater narcotic consumption (p ≤ 0.001, all). Patients with higher BMI (obese I, obese II–III) reported inferior preoperative PROMIS-PF, VAS-BP, and ODI scores (p ≤ 0.003, all). Postoperatively, obese I–III cohorts demonstrated inferior PROMIS-PF, PHQ-9, VAS-BP, and ODI scores at final follow-up (p ≤ 0.016, all). However, patients demonstrated similar postoperative changes and MCID achievement regardless of preoperative BMI.
Conclusion
Patients undergoing lumbar decompression demonstrated similar postoperative improvement in physical function, anxiety, pain interference, sleep disturbance, mental health, pain, and disability outcomes independent of preoperative BMI. However, obese patients reported worse physical function, mental health, back pain, and disability outcomes at final postoperative follow-up. Patients with greater BMI undergoing lumbar decompression demonstrate inferior postoperative clinical outcomes.
Similar content being viewed by others
Data Availability
The data that support the findings of this study were generated at Rush University Medical Center and are available upon reasonable request from the corresponding author KS.
Abbreviations
- ANOVA:
-
Analysis of variance
- ASA:
-
American Society of Anesthesiologists
- BMI :
-
Body mass index
- CCI:
-
Charlson Comorbidity Index
- EBL:
-
Estimated blood loss
- LD:
-
Lumbar decompression
- LOS:
-
Length of stay
- MCID:
-
Minimum clinically important difference
- ODI:
-
Oswestry Disability Index
- ORA :
-
Office of Regulatory Affairs
- PHQ-9:
-
Patient Health Questionnaire-9
- POD:
-
Postoperative day
- PROMIS:
-
Patient-Reported Outcomes Measurement Information System
- PROMIS-A:
-
Patient-Reported Outcomes Measurement Information System Anxiety
- PROMIS-PF:
-
Patient-Reported Outcomes Measurement Information System Physical Function
- PROMIS-PI:
-
Patient-Reported Outcomes Measurement Information System Pain Interference
- PROMIS-SD:
-
Patient-Reported Outcomes Measurement Information System Sleep Disturbance
- PROs :
-
Patient-reported outcome
- SF-12:
-
12-Item Short Form
- SF-36 PCS :
-
36-Item Short Form Physical Component Score
- VAS:
-
Visual Analog Scale
- VAS-BP:
-
Visual Analog Scale Back Pain
- VAS-LP:
-
Visual Analog Scale Leg Pain
References
Amtmann D, Cook KF, Jensen MP et al (2010) Development of a PROMIS item bank to measure pain interference. Pain 150(1):173–182
Belcaid I, Eipe N (2019) Perioperative pain management in morbid obesity. Drugs 79(11):1163–1175
Bryan S, Afful J, Carroll M et al (2021) NHSR 158. National Health and Nutrition Examination Survey 2017–March 2020 pre-pandemic data files. Centers for Disease Control and Prevention. https://doi.org/10.15620/cdc:106273
Chen CX, Kroenke K, Stump TE et al (2018) Estimating minimally important differences for the PROMIS pain interference scales: results from 3 randomized clinical trials. Pain 159(4):775–782
Chiolero A, Faeh D, Paccaud F, Cornuz J (2008) Consequences of smoking for body weight, body fat distribution, and insulin resistance. Am J Clin Nutr 87(4):801–809
Chou L, Brady SRE, Urquhart DM et al (2016) The association between obesity and low back pain and disability is affected by mood disorders: a population-based, cross-sectional study of men. Medicine (Baltimore) 95(15):e3367
De la Garza-Ramos R, Bydon M, Abt NB et al (2015) The impact of obesity on short- and long-term outcomes after lumbar fusion. Spine (Phila Pa 1976) 40(1):56–61
Dority J, Hassan ZU, Chau D (2011) Anesthetic implications of obesity in the surgical patient. Clin Colon Rectal Surg 24(4):222–228
Epstein NE (2017) More risks and complications for elective spine surgery in morbidly obese patients. Surg Neurol Int 8(1):66
Goyal A, Elminawy M, Kerezoudis P et al (2019) Impact of obesity on outcomes following lumbar spine surgery: a systematic review and meta-analysis. Clin Neurol Neurosurg 177:27–36
Gu JK, Charles LE, Andrew ME et al (2016) Prevalence of work-site injuries and relationship between obesity and injury among U.S. workers: NHIS 2004–2012. J Saf Res 58:21–30
Haws BE, Khechen B, Bawa MS et al (2019) The Patient-Reported Outcomes Measurement Information System in spine surgery: a systematic review. J Neurosurg Spine 30(3):405–413
Ibaseta A, Rahman R, Andrade NS et al (2021) Determining validity, discriminant ability, responsiveness, and minimal clinically important differences for PROMIS in adult spinal deformity. J Neurosurg Spine 34(5):725–733
Jackson KL 2nd, Devine JG (2016) The effects of obesity on spine surgery: a systematic review of the literature. Glob Spine J 6(4):394–400
Jiang J, Teng Y, Fan Z, Khan S, Xia Y (2014) Does obesity affect the surgical outcome and complication rates of spinal surgery? A meta-analysis. Clin Orthop Relat Res 472(3):968–975
Lim Y, Boster J (2022) Obesity and comorbid conditions. In: StatPearls [Internet]. StatPearls Publishing
Lynch CP, Cha EDK, Jenkins NW et al (2021) The minimum clinically important difference for patient health questionnaire-9 in minimally invasive transforaminal interbody fusion. Spine 46(9):603–609
Ogden CL, Fryar CD, Hales CM, Carroll MD, Aoki Y, Freedman DS (2018) Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013–2016. JAMA 319(23):2410
Pantalone KM, Hobbs TM, Chagin KM et al (2017) Prevalence and recognition of obesity and its associated comorbidities: cross-sectional analysis of electronic health record data from a large US integrated health system. BMJ Open 7(11):e017583
Park C, Garcia AN, Cook C, Shaffrey CI, Gottfried ON (2020) Long-term impact of obesity on patient-reported outcomes and patient satisfaction after lumbar spine surgery: an observational study. J Neurosurg Spine 34(1):1–10
Parker SL, Adogwa O, Paul AR et al (2011) Utility of minimum clinically important difference in assessing pain, disability, and health state after transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Neurosurg Spine 14(5):598–604
Patel N, Bagan B, Vadera S et al (2007) Obesity and spine surgery: relation to perioperative complications. J Neurosurg Spine 6(4):291–297
Pi-Sunyer FX (1999) Comorbidities of overweight and obesity: current evidence and research issues. Med Sci Sports Exerc 31(11 Suppl):S602–S608
Rihn JA, Radcliff K, Hilibrand AS et al (2012) Does obesity affect outcomes of treatment for lumbar stenosis and degenerative spondylolisthesis? Analysis of the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976) 37(23):1933–1946
Shiri R, Lallukka T, Karppinen J, Viikari-Juntura E (2014) Obesity as a risk factor for sciatica: a meta-analysis. Am J Epidemiol 179(8):929–937
Soroceanu A, Burton DC, Diebo BG et al (2015) Impact of obesity on complications, infection, and patient-reported outcomes in adult spinal deformity surgery. J Neurosurg Spine 23(5):656–664
Stokes A, Berry KM, Collins JM et al (2019) The contribution of obesity to prescription opioid use in the United States. Pain 160(10):2255–2262
Witter JP (2016) The promise of Patient-Reported Outcomes Measurement Information System-turning theory into reality: a uniform approach to patient-reported outcomes across rheumatic diseases. Rheum Dis Clin N Am 42(2):377–394
Zhang TT, Liu Z, Liu YL, Zhao JJ, Liu DW, Tian QB (2018) Obesity as a risk factor for low back pain: a meta-analysis. Clin Spine Surg 31(1):22–27
Author information
Authors and Affiliations
Contributions
James W. Nie, BS: Conceptualization, methodology, visualization, formal analysis, software, investigation, writing — original draft, writing — review and editing.
Timothy J. Hartman, MD: Conceptualization, methodology, visualization, formal analysis, software, investigation, writing — original draft, writing — review and editing.
Eileen Zheng, BS: Project administration, data curation, investigation, writing — review and editing.
Omolabake O. Oyetayo, BS: Project administration, data curation, investigation, writing — review and editing.
Keith R. MacGregor, BS: Project administration, data curation, investigation, writing — review and editing.
Vincent P. Federico, MD: Conceptualization, methodology, supervision, resources, investigation, writing — review and editing.
Dustin H. Massel, MD: Conceptualization, methodology, supervision, resources, investigation, writing — review and editing.
Arash J. Sayari, MD: Conceptualization, methodology, supervision, resources, investigation, writing — review and editing.
Corresponding author
Ethics declarations
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Review Board (IRB) of Rush University Medical Center (ORA #14051301).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Financial interests
Kern Singh, MD, receives royalties from Zimmer Biomet, Stryker, RTI Surgical, Lippincott Williams and Wilkins, Thieme, Jaypee Publishing, and Slack Publishing. Kern Singh, MD, owns stock in Avaz Surgical LLC and Vital 5 LLC. Kern Singh, MD, holds a consulting position with Zimmer Biomet and K2M. Kern Singh, MD, holds board membership with Vital 5 LLC. Kern Singh, MD, is on the editorial board of Contemporary Spine Surgery. Kern Singh, MD, received a research grant from the Cervical Spine Research Society.
Non-financial interests
Kern Singh, MD, holds board membership with TDi LLC and Minimally Invasive Spine Study Group and receives no compensation as board member. Kern Singh, MD, is on the editorial board of Orthopedics Today and Vertebral Columns and receives no compensation as member of the editorial board. Kern Singh, MD, is on the board of directors of Cervical Spine Research Society, International Society for the Advancements of Spine Surgery, and American Academy of Orthopaedic Surgeons and receives no compensation as member of the board of directors.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Spine - Other
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nie, J.W., Hartman, T.J., Zheng, E. et al. Impact of body mass index on PROMIS outcomes following lumbar decompression. Acta Neurochir 165, 1427–1434 (2023). https://doi.org/10.1007/s00701-023-05534-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05534-5