Abstract
Background
There is uncertainty regarding delayed removal versus retention of minimally invasive screws following percutaneous fixation for thoracolumbar fractures. We conducted a systematic review and case–control study to test the hypothesis that delayed metalwork removal following percutaneous fixation for thoracolumbar fractures improves outcome.
Methods
A systematic review was performed in accordance with the PRISMA guidelines. Our case–control study retrospectively evaluated 55 consecutive patients with thoracolumbar fractures who underwent percutaneous fixation in a single unit: 19 with metalwork retained (controls) and 36 with metalwork removed. Outcomes were the Oswestry Disability Index (ODI), a supplemental questionnaire, and complications.
Results
The systematic review evaluated nine articles. Back pain was reduced in most patients after metalwork removal. One study found no difference in the ODI after versus before metalwork removal, whereas three studies reported significant improvement. Six studies noted no significant alterations in radiological markers of stability after metalwork removal. Mean complication rate was 1.7% (0–6.7). Complications were superficial wound infection, screw breakage at the time of removal, pull-out screw, and a broken rod. In the case–control study, both groups were well matched. For metalwork removal, mean operative time was 69.5 min (range 30–120) and length of stay was 1.3 days (0–4). After metalwork removal, 24 (68.6%) patients felt better, 10 (28.6%) the same and one felt worse. Two patients had superficial hematomas, one had a superficial wound infection, and none required re-operation. Metalwork removal was a significant predictor of return to work or baseline household duties (odds ratio 5.0 [1.4–18.9]). The ODI was not different between groups.
Conclusions
The findings of both the systematic review and our case–control study suggest that removal of metalwork following percutaneous fixation of thoracolumbar fractures is safe and is associated with improved outcome in most patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 90% of spinal fractures are thoracolumbar [7]; some of which are managed conservatively [1, 7] and some operatively by pedicle screws and rod fixation [3, 18, 23]. Increasingly, surgical fixation is performed percutaneously rather than open [3, 18, 23]. Advantages of the percutaneous versus the open technique include: smaller wounds, less blood loss, shorter surgery, less pain, less muscle dissection, shorter stay, and lower infection rate [18].
Once the fractures have healed, some surgeons remove the metalwork while others leave it in situ [24]. A meta-analysis of the removal versus retention of metalwork after open placement found variable outcomes with sample and study heterogeneity; removal in younger patients achieved superior functional outcomes without progressive deformity [12]. The argument for removing the metalwork is more compelling for percutaneous than open surgery, because removing percutaneously placed screws and rods is a small procedure that involves re-opening the small stab incisions and little tissue dissection compared with re-opening the long midline incision and extensive muscle dissection when removing openly placed pedicle screws and rods [15].
To investigate the evidence base in favour of removal versus retention of percutaneously placed metalwork, we performed a systematic review of relevant studies. This identified a gap in knowledge regarding which management option is superior. In our unit, some spinal surgeons do and some do not routinely remove the metalwork after percutaneous placement in neurologically intact patients. We exploited this variability in practice, performing a case–control study, to evaluate whether the routine removal of metalwork in these patients is beneficial. Based on published evidence and our study, we analyse whether the two are congruent and propose guidelines for the routine removal of metalwork after percutaneous pedicle screw and rod fixation for thoracolumbar fractures.
The specific aims of the study were.
-
1.
To perform a systematic review to evaluate if there are clinical and/or functional differences in patients’ in whom metalwork is removed
-
2.
To test the hypothesis that following percutaneous fixation for thoracolumbar fractures, metalwork removal improves functional outcome
Materials and methods
Systematic review
PICO
Population: patients with thoracolumbar fractures who underwent percutaneous pedicle screw/rod fixation.
Intervention: elective removal of metalwork.
Comparison: retention of metalwork.
Outcome: any clinical or functional outcome.
Systematic search
A systematic search according to PRISMA guidelines utilizing the PubMed, EMBASE, Cochrane Database and Google Scholar was conducted. The databases were queried with the following search terms using different Boolean combinations to maximize data capture: ‘percutaneous’, ‘implant’, ‘instrument*’, ‘fixation’, ‘metalwork’, ‘metalware’, ‘remov*’, ‘thoracolumbar’, ‘vertebra’, and ‘fracture’. Only studies with the full text available in English were included. All retrieved titles and abstracts were independently screened by two reviewers (RV and MCP). The full texts of the most relevant studies were evaluated to assess their eligibility for inclusion.
Inclusion/exclusion
Inclusion criteria were 1) randomized or non-randomized controlled trials, cohort, or case series examining thoracolumbar fractures with or without neurological deficit, 2) posterior percutaneous fixation of thoracolumbar fractures with planned removal of metalwork, and 3) reported clinical or radiological follow-up outcomes after metalwork removal, relating to pain and/or functional status. The included studies were stratified according to the presence or absence of neurological deficit.
Case control study
Patients
We performed a retrospective service evaluation of patients consecutively treated in our unit (2014–2020). The inclusion criteria were: 1) thoracic or lumbar fracture, 2) traumatic injury, and 3) percutaneous pedicle screw or rod fixation. The exclusion criteria were 1) neurological deficit at presentation, 2) non-traumatic cause (e.g., cancer), 3) open pedicle screw/rod fixation, and 4) no follow-up. The patients were divided into two groups according to whether the metalwork was retained (group A) or removed (group B).
Baseline characteristics
For all patients, we collected demographics (age at injury, sex, and Charlson morbidity index), and injury characteristics (AO classification, mechanism, other injuries, and levels). There are different methods of accounting for the confounding effect of multiple variables. We opted to perform univariate logistic regression and then include all significant variables in a multivariate logistic model.
Metalwork insertion
Percutaneous pedicle screw fixation was performed under general anaesthesia with the Stryker ES-II system using bi-planar X-ray guidance. The operating surgeon determined the number of vertebral levels to be fixed. We recorded the number of fixed levels (i.e., L2–4 fixation for L3 burst fracture denotes a 2-level fixation reflecting the number of instrumented vertebral levels), duration of surgery, blood loss, length of stay (LOS), and complications.
Metalwork removal
Metalwork removal surgery was performed 1 year (median; range 5–27 months) post-fixation. The decision for removal at this time was dependent upon patients’ symptoms, satisfactory post-operative imaging, and patient/surgeon preference. Surgery was performed under general anaesthesia by re-opening the stab incisions to remove the blockers, rods, and screws. We recorded the duration of surgery, blood loss, LOS, and complications.
Long-term follow-up
For all patients, we recorded the post-operative Oswestry Disability Index (ODI) [5] and a 6-point questionnaire administered by phone or post as follows:
-
1.
If you still take pain medication, please write down the names of the medications and how often you take them.
-
2.
What date was your original operation?
-
3.
Have you had your metalwork removed? If so, what date was it done?
-
4.
Did you require any further spinal operations after removal of your metalwork?
-
5.
Did removing the metalwork make you feel better, worse, or no change?
-
6.
Have you returned to work or homemaking duties? If not, can you state why?
Statistical analysis
Data are presented as mean (range) for continuous variables and frequency (%) for categorical variables. Baseline characteristics for group A versus group B were compared using the Student’s t-test (Microsoft Excel for Mac 2021, v.16.54) or Fisher’s exact test. Statistical analyses were performed using XLSTAT-Life Sciences software (v. 2021.5 by Addinsoft). Binary logistic regression was used to identify predictive factors for: 1) return to work or baseline activities and 2) analgesia use. Multinomial logistic regression was used to identify the predictive factors for the ODI. Statistical significance was set at P < 0.05.
Results
Initially, we present the preliminary findings of the (i) systematic review and (ii) case–control study. Then, we present a parameter-based comparative analysis of the findings between the systematic review then our-case control study, and summaries. Parameters evaluated include timing of metalwork removal, pain outcomes, disability, return-to-work status, deformity, and complication rates.
Systematic review
Study inclusion
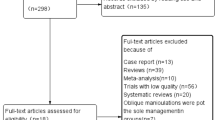
A systematic search yielded 12,264 articles, which were reduced to 8,376 after removing duplicates; 4,542 articles were removed using automation tools, leaving 3,834 abstracts for screening. After excluding papers not relevant to our PICO query, there were 25 left for full-text eligibility assessment, of which 9 were ultimately included in the review [2, 4, 8, 11, 13, 14, 16, 20, 21] (Fig. 1) [17]. Reasons for exclusion were other fracture locations, non-percutaneous/open or heterogeneous fixation techniques, unreported parameters of interest, or whether the study research question was irrelevant to our PICO query. Table 1 summarizes the nine relevant studies. There are two class II (prospective), six class III (retrospective), and one class IV (case series) studies. Six studies consider neurologically intact patients and three consider patients with a neurological deficit. The one study comparing patients with metalwork removed versus not removed [14] had selection bias as the metalwork removed group comprises 6 cases with complications from the primary surgery that prompted the metalwork removal. No other study other than our own compares instrumentation removed versus retained patient groups. Therefore, from the systematic review, there are only comparisons of pre- versus post-metalwork removal. No studies comprehensively looked at postoperative analgesia requirement, return to work/functional status, and operative factors (blood loss, operative time, and length of stay) of the metalwork removal group. These were incorporated in our case–control study.
Case control study
Patient characteristics
One hundred patient records met the inclusion/exclusion criteria, of which complete follow-up was available for 55 cases; all of which were included. Overall, mean age was 43.4 years (range 12–74), male:female was 1.04:1 (50.9%:49.1%), 7 fractures were only thoracic, 15 only lumbar, and 33 thoracolumbar, mean number of levels fixed was 3 (2–4), minimal blood loss (< 100 ml) was commonest (67.3%; in the remainder, mean was 205 mL [100–300]), and mean length of stay was 8.1 days (3–20). We then compared the 19 group A versus the 36 group B patients. There was a higher proportion of females in group B but this difference was not significant. Patients were followed-up for a mean of 44.9 months (10–83) in group A and 43.3 months (11–76) in group B post-surgery. Table 1 shows no significant differences in group A versus group B patients for demographics, co-morbidities, level of injury, fracture morphology, injury mechanism, operative levels fixed, number of screws placed, blood loss, and complications.
Comparative analysis of parameters between systematic review and case–control study
Timing of metalwork removal
The timing of metalwork removal surgery was clearly reported in 7/9 (77.8%) studies. Overall, the mean was 14.1 months (10–24), compared with 13.3 (5–27) months in our study (Table 2).
Summary: timing of metalwork removal was similar in the review and our study.
Pain outcomes
Six (66.7%) out of 9 studies [2, 8, 11, 13, 14, 20] used the visual analogue score and reported less pain after versus before metalwork removal; 1/9 (11.1%) study [14] concluded minimal pain post-metalwork removal; 1/9 (11.1%) study [16] reported no difference in pain between patients who had the metalwork removed before versus after 12 months of insertion. In our study, the pain component of the ODI and supplemental questionnaire captured pain evaluation. Most patients reported metalwork removal as beneficial: 24 (68.6%) felt better, 10 (28.6%) the same, and 1 worse (2.8%). Our univariate binary logistic regression model found that the number of fixed levels was a predictor of analgesic use, i.e., the greater the number of levels fixed, the increased likelihood of long-term analgesia requirement. This finding remained significant in the multivariate analysis (Supplemental Table 1).
Summary: pain outcomes are more frequently improved post metalwork removal in the review and our study.
Disability
One (11.1%) out of nine studies found no difference in ODI after versus before metalwork removal [16], whereas 3/9 (33.3%) studies reported significant improvement in ODI [2, 8, 20], all in patients with preoperative neurological deficit. In our study, the mean ODI at follow-up was lower in group B than in group A, but the difference was not significant. A multinomial logistic regression model revealed that metalwork removal, age, Charlson co-morbidity index, spinal injury level, and number of levels fixed were not significant predictors of ODI (Supplemental Table 2).
Summary: Although the systematic review showed that ODI tends to be better in post-metalwork removal, our study did not replicate this finding to statistical significance.
Return to work
Only 1/9 (11.1%) studies examined return to work [14], reporting mean of 7 months in the metalwork removed group versus 6 months in the metalwork retained group (not significant); in this study, the metalwork was removed due to complications from the primary surgery. In our study, a univariate binary logistic regression model showed that group B patients are 5 times more likely to return to work or baseline household activities than group A patients (Table 3). Age, Charlson co-morbidity index, injury level, and the number of fixed levels were not significant predictors of return to work or baseline household activities.
Summary: Our finding of enhanced return to work/function, unaffected by several other variables, is not consistent with the single study from the review that evaluated this parameter. Clearly, this is an understudied yet critical metric, which warrants further evaluation.
Deformity
Seven (77.8%) out of 9 studies examined various radiographic markers of stability/deformity (correction loss, fracture angle, sagittal index, compression %, degree of displacement, deformation angle, local kyphosis, Cobb angle, disc degeneration, vertebral height loss, range of motion, radiographic fusion, segmental motion angle, canal stenosis index, and residual mobility). Of these seven studies, six (85.8%) concluded that there was no significant alteration in markers of stability after versus before metalwork removal. Although 1/7 (14.2%) studies [8] noted kyphotic recurrence in 4/31 (12.9%) patients after metalwork removal, there were significant improvements in pain measures in these patients and no patient required additional surgery. Our study did not specifically examine radiological markers of stability. No patients from our removal group required further surgery for progressive instability.
Summary: in the vast majority of cases from the review, there is no clinically significant progressive deformity warranting further surgery following metalwork removal.
Complications
Reported risks of metalwork removal surgery from the review were low with a mean complication rate of 1.7% (0–6.7). Complications were minor, including superficial wound infection, screw breakage at the time of removal, one pull-out screw, and broken rod. No studies specifically examined blood loss, operative time, and length of stay, which we examined in our study. In our study, metalwork removal surgery had minimal blood loss in 94% of cases, mean operative time was 69.5 min (39–120), and mean length of stay was 1.3 days (0–4). Complication rate was low (n = 3/33, 9.1%) including 2 superficial hematomas and 1 superficial wound infection; all were managed conservatively with no long-term adverse sequelae (Table 4). Patients were followed up for a mean of 31.8 months (4–71) post-metalwork removal. Data from the second operation (removal) was not combined with data from the first operation (fixation).
Summary: Metalwork removal is associated with a low rate of complications (1.7%) in the review. Similarly, our study had a low complication rate.
Discussion
The systematic review highlights that metalwork removal of percutaneously placed metalwork is safe and beneficial with improvements in pain and disability scores without compromising stability and causing significant complications. The key finding from our case–control study is that removal of metalwork benefits an earlier return to work or baseline function, independent of demographics, co-morbidities, or injury level. We also found that a greater number of fixed levels were predictive of higher analgesic use at follow-up. There is reasonable agreement between the findings of the systematic review and our case–control study in terms of timing of surgery, pain outcomes, and complication rates. However, in our study, the ODI measures were not significantly different between groups and we did not objectively assess deformity measures. Deficient in the systematic review were return to work rates and operative factors of metalwork removal (blood loss, length of stay), warranting further studies.
Patients often mention that the fixation limits their range of movements, causes stiffness, and causes intermittent pain (may be related to occupation) that is positional or related to prominent metalwork under the skin. Theories of instrumentation-related symptoms include micromotion, metal fretting, allergic reaction, low-grade infection, and stress concentration at the adjacent segments [6, 9, 10, 19, 22]. These factors likely influence return to work or baseline activities but may not be captured by the ODI or pain score and are eliminated by metalwork removal.
Our systematic review revealed that although the question of whether percutaneous screws should be retained or removed has received little attention, the published reports favour removal. Most studies report that metalwork removal improves pain [2, 4, 8, 11, 13, 14, 20] and, importantly, there are no reports of worse pain. There are also significant improvements in disability or the chance of returning to work [2, 8, 14, 20, 21]. Removing the metalwork does not cause progressive deformity in most patients [2, 11, 13, 16, 20, 21]. The increased deformity reported in a few patients [8] is clinically unimportant, because it was associated with improved pain scores and did not necessitate additional surgery. The complication rate is low, and the complications are minor and short term. On average, most surgeons remove the metalwork after a year [2, 8, 11, 13, 14, 16, 20, 21], although there is evidence that earlier removal may be associated with an increased range of movements [20].
Study limitations
The limitations of published studies include heterogeneity of outcomes and patient inclusion criteria, no class I evidence, and no controls. There is no specific consideration to operative factors of metalwork removal surgery. Limitations of our case–control study include the small numbers of patients, retrospective nature, loss to follow-up, and lack of long-term radiological stability data. Due to the small numbers of patients, it was impossible to examine the effect of patient age or length of construct on outcome. However, we used demographically matched groups to compare outcomes, and none of our cohort with the metalwork removed required further surgery for kyphotic deformity correction, which is in line with the literature. None of the studies (including ours) performed an economic analysis to compare the cost of removal surgery versus the financial gains of improved quality of life and return to work after metalwork removal. In addition, none of the studies (including ours) evaluated the psychosocial morbidity, which may influence subjective measures of postoperative pain and return to normal function after spinal injury.
Based on the literature review and our case–control study, we make the following eight recommendations to guide spinal surgeons facing the question of whether to remove the metalwork after percutaneous fixation of thoracolumbar fractures. We note that there is no class I evidence, and the strength of recommendations (SOR) is based on a small number of studies with small numbers of patients:
-
1.
Should the metalwork be removed? The review and our study favour metalwork removal. SOR: moderate.
-
2.
Does it make a difference whether there is neurological deficit or not? From the review, both patient groups may benefit. SOR: moderate.
-
3.
Does metalwork removal reduce pain? There is evidence of improvement in pain; however, this finding is not consistent across studies. SOR: weak.
-
4.
Does metalwork removal reduce disability? There is evidence of improvement in disability; however, this finding is not consistent across studies. SOR: weak.
-
5.
Does metalwork removal improve the chances of returning to work? Yes, based on our study, not the review. SOR: weak.
-
6.
Will metalwork removal de-stabilize the spine to require further surgery? There is consistent evidence that the spine does not de-stabilize and that removal does not lead to further surgery. SOR: strong.
-
7.
What is the optimal time for metalwork removal? On average, one year after insertion. There is evidence that earlier removal (6–12 months) is equally safe and effective and more likely to restore movement. SOR: moderate.
-
8.
What does the removal surgery involve? Based on our experience, it involves a small operation under general anaesthesia. Hospital stay is usually 1–2 nights. The risk of complications is low, and the commonest complications are minor, including superficial wound infection and hematoma. SOR: strong.
Conclusions
Based on the systematic review and our study, metalwork removal is safe and may confer benefits including reduced pain and disability and increased chance of returning to work. On average, removal was performed approximately 1 year after the injury. The level of evidence is low.
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ASIA:
-
American Spinal Injury Association Impairment Scale
- AVHR :
-
Anterior vertebral height ratio
- CI:
-
Confidence interval
- CA :
-
Cobb’s angle
- CL :
-
Correction loss
- C% :
-
Compression percentage
- CSI :
-
Canal stenosis index
- DA :
-
Deformation angle
- DD :
-
Degree displacement
- FA :
-
Fracture angle
- KA :
-
Correction loss
- L:
-
Lumbar
- LOS :
-
Length of stay
- NRS-B/L :
-
Numeric Rating Scales for Back and Leg pain
- ODI :
-
Oswestry Disability Index
- PICO :
-
Population, Intervention, Comparison, Outcome [framework]
- ROM:
-
Range of movement
- RTA:
-
Road traffic accident
- RTW:
-
Return to work
- SF-12 :
-
12-Item short-form survey
- SI:
-
Sagittal index
- SMA :
-
Segmental motion angle
- T:
-
Thoracic
- TLICS :
-
Thoracolumbar Injury Classification and Severity Scale
- TLJ:
-
Thoracolumbar junction
- VAS :
-
Visual Analog Scale
- VBH :
-
Vertebral body height
- VH :
-
Vertebral height loss
References
Abudou M, Chen X, Kong X, Wu T (2013) Surgical versus non-surgical treatment for thoracolumbar burst fractures without neurological deficit. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD005079.pub3
Chen L, Liu H, Hong Y, Yang Y, Hu L (2020) Minimally invasive decompression and intracorporeal bone grafting combined with temporary percutaneous short-segment pedicle screw fixation for treatment of thoracolumbar burst fracture with neurological deficits. World Neurosurg 135:e209–e220
Cheng LM, Wang JJ, Zeng ZL, Zhu R, Yu Y, Li C, Wu ZR (2013) Pedicle screw fixation for traumatic fractures of the thoracic and lumbar spine. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD009073.pub2
Cox JB, Yang M, Jacob RP, Pincus DW (2013) Temporary percutaneous pedicle screw fixation for treatment of thoracolumbar injuries in young adults. J Neurol Surg A Cent Eur Neurosurg 74(1):7–11
Fairbank JC, Pynsent PB (2000) The Oswestry Disability Index. Spine (Phila Pa 1976) 25(22):2940–52
Gaine WJ, Andrew SM, Chadwick P, Cooke E, Williamson JB (2001) Late operative site pain with Isola posterior instrumentation requiring implant removal. Spine (Phila Pa 1976) 26(5):583–587
Ghobrial GM, Maulucci CM, Maltenfort M, Dalyai RT, Vaccaro AR, Fehlings MG, Street J, Arnold PM, Harrop JS (2014) Operative and nonoperative adverse events in the management of traumatic fractures of the thoracolumbar spine: a systematic review. Neurosurg Focus 37(1):E8
Han M-S, Lee G-J, Lee S-K, Jang J-W, Moon BJ, Lee J-K, Lee S-S (2021) Risks and benefits of timely screw removal after thoracolumbar spine fractures treated with non-fusion technique. J Clin Neurosci 89:397–404
Kim H-J, Chun H-J, Moon S-H, Kang K-T, Kim H-S, Park J-O, Moon E-S, Sohn J-S, Lee H-M (2010) Analysis of biomechanical changes after removal of instrumentation in lumbar arthrodesis by finite element analysis. Med Biol Eng Comput 48(7):703–709
Kim H-J, Kang K-T, Moon S-H, Chun H-J, Kim H-S, Park J-O, Moon E-S, Kim B-R, Sohn J-S, Lee H-M (2011) The quantitative assessment of risk factors to overstress at adjacent segments after lumbar fusion. Spine (Phila Pa 1976) 36(17):1367–1373
Kim HS, Kim SW, Il JuC, Wang HS, Lee SM, Kim DM (2014) Implant removal after percutaneous short segment fixation for thoracolumbar burst fracture : does it preserve motion? J Korean Neurosurg Soc 55(2):73–77
Kweh BTS, Tan T, Lee HQ, Hunn M, Liew S, Tee JW (2022) Implant removal versus implant retention following posterior surgical stabilization of thoracolumbar burst fractures: a systematic review and meta-analysis. Global Spine J 12(4):700–718
Lorente R, Palacios P, Vaccaro A, Mariscal G, Diamantopoulus J, Lorente A (2021) Safety and utility of implant removal after percutaneous osteosynthesis of type A thoracolumbar and lumbar fracture. Orthop Traumatol Surg Res 107(7):102740
Manson N, El-Mughayyar D, Bigney E, Richardson E, Abraham E (2020) Instrumentation removal following minimally invasive posterior percutaneous pedicle screw-rod stabilization (PercStab) of thoracolumbar fractures is not always required. Adv Orthop 2020:7949216
Ntilikina Y, Bahlau D, Garnon J, Schuller S, Walter A, Schaeffer M, Steib J-P, Charles YP (2017) Open versus percutaneous instrumentation in thoracolumbar fractures: magnetic resonance imaging comparison of paravertebral muscles after implant removal. J Neurosurg Spine 27(2):235–241
Oh H-S, Seo H-Y (2019) Percutaneous pedicle screw fixation in thoracolumbar fractures: comparison of results according to implant removal time. Clin Orthop Surg 11(3):291–296
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Phan K, Rao PJ, Mobbs RJ (2015) Percutaneous versus open pedicle screw fixation for treatment of thoracolumbar fractures: systematic review and meta-analysis of comparative studies. Clin Neurol Neurosurg 135:85–92
Pinto MR, Bressan C, Wroblewski JM, Wild A, Butler L (2003) Removal of lumbar instrumentation for the treatment of recurrent low back pain in the absence of pseudarthrosis. Arch Orthop Trauma Surg 123(8):414–418
Proietti L, Perna A, Schirò GR, Noia G, Fumo C, Tamburrelli FC (2019) Residual mobility after removal of instrumentation in patient, with type a2-a3 vertebral fractures, treated with percutaneous pedicle screw fixation. J Biol Regul Homeost Agents. 2019 Mar-Apr;33(2 Suppl. 1):133-139. XIX Congresso Nazionale S.I.C.O.O.P. Societa' Italiana Chirurghi Ortopedici Dell'ospedalita' Privata Accreditata
Sasagawa T, Takagi Y, Hayashi H, Nanpo K (2021) Patient satisfaction with implant removal after stabilization using percutaneous pedicle screws for traumatic thoracolumbar fracture. Asian J Neurosurg 16(4):765
Stavridis SI, Bücking P, Schaeren S, Jeanneret B, Schnake KJ (2010) Implant removal after posterior stabilization of the thoraco-lumbar spine. Arch Orthop Trauma Surg 130(1):119–123
Tian F, Tu L-Y, Gu W-F, Zhang E-F, Wang Z-B, Chu G, Ka H, Zhao J (2018) Percutaneous versus open pedicle screw instrumentation in treatment of thoracic and lumbar spine fractures. Med (Baltimore) 97(41):e12535
Wu J, Zhu J, Wang Z et al (2022) Outcomes in thoracolumbar and lumbar traumatic fractures: does restoration of unfused segmental mobility correlated to implant removal time? World Neurosurg 157:e254–e263
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed consent was obtained from all patients before each surgical procedure. The project was part of a departmental audit to evaluate outcome after percutaneous pedicle screw fixation in our unit. Our hospital clinical audit facilitator advised that this project did not need to be submitted to a Research Ethics Committee for ethical approval because nothing was done to the patients beyond their routine clinical management.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Spine trauma
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Visagan, R., Kearney, S., Trifoi, S. et al. Removal or retention of minimally invasive screws in thoracolumbar fractures? Systematic review and case–control study. Acta Neurochir 165, 885–895 (2023). https://doi.org/10.1007/s00701-023-05514-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05514-9