Abstract
Background
There is a scarcity of literature that examines clinical outcomes through patient-reported outcomes (PROs), minimum clinically important difference (MCID), and recovery ratios (RR) for workers’ compensation (WC) recipients undergoing minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) versus anterior lumbar interbody fusion (ALIF).
Methods
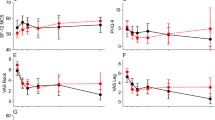
WC claimants undergoing MIS-TLIF versus ALIF were propensity score matched to account for demographic differences. Demographics, perioperative characteristics, and PROs were collected. PROs of Patient-Reported Outcomes Measurement Information System Physical Function (PROMIS-PF), 12-Item Short Form Physical Composite Score (SF-12 PCS), Visual Analog Scale (VAS) back, VAS leg, and Oswestry Disability Index (ODI) were collected at preoperative and postoperative time points. MCID achievement was determined through comparison to values in literature. RR was calculated as the difference between postoperative and preoperative PROs over potential improvement. Comparison between surgical techniques was through non-parametric inferential statistics.
Results
Eighty-four WC claimants, with 50 patients undergoing MIS-TLIF, were identified after propensity score matching. ALIF patients had higher estimated blood loss. MIS-TLIF patients had higher postoperative day (POD) 0 VAS pain and POD 0 + 1 narcotic consumption. Patients undergoing either MIS-TLIF or ALIF reported significant improvement in pain and disability. ALIF patients reported significant improvement in physical function. ALIF patients reported superior 1-year PROMIS-PF, 6-week SF-12 PCS, 6-month VAS back, and 12-week VAS leg. No significant differences in MCID achievement rates were noted between cohorts. ALIF patients had higher RR in 6-week and 1-year PROMIS-PF and 6-week SF-12 PCS.
Conclusion
Workers’ compensation claimants undergoing either MIS-TLIF or ALIF reported significant improvement in pain and disability. ALIF patients reported superior postoperative physical function and pain. ALIF patients had higher recovery ratios in physical function. Workers’ compensation claimants undergoing ALIF may experience greater physical function recovery and superior clinical outcomes in physical function and pain.
Similar content being viewed by others
Data Availability
The data that support the findings of this study were generated at Rush University Medical Center and are available upon reasonable request from the corresponding author KS.
Abbreviations
- ALIF:
-
Anterior lumbar interbody fusion
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
Body mass index
- CCI:
-
Charlson Comorbidity Index
- HNP:
-
Herniated nucleus pulposus
- IRB:
-
Institutional Review Board
- MCID:
-
Minimum clinically important difference
- MIS-TLIF:
-
Minimally invasive transforaminal lumbar interbody
- ODI:
-
Oswestry Disability Index
- PLIF:
-
Posterior lumbar interbody fusion
- POD:
-
Postoperative day
- PROMIS-PF:
-
Patient-Reported Outcomes Measurement Information System Physical Function
- PROs:
-
Patient-reported outcomes
- RR:
-
Recovery ratio
- SD:
-
Standard deviations
- SF-12 PCS:
-
12-Item Short Form Physical Component Score
- TLIF:
-
Transforaminal lumbar interbody fusion
- VAS:
-
Visual Analog Scale
- WC:
-
Workers’ compensation
References
Brodke DS, Goz V, Voss MW, Lawrence BD, Spiker WR, Hung M (2017) PROMIS PF CAT outperforms the ODI and SF-36 Physical Function Domain in spine patients. Spine (Phila Pa 1976) 42(12):921–929
Chen DA, Vaishnav AS, Louie PK et al (2020) Patient reported outcomes in patients who stop following up: Are they doing better or worse than the patients that come back? Spine (Phila Pa 1976) 45(20):1435–1442
Costa MA, Silva PS, Vaz R, Pereira P (2021) Correlation between clinical outcomes and spinopelvic parameters in patients with lumbar stenosis undergoing decompression surgery. Eur Spine J 30(4):928–935
Fujibayashi S, Neo M, Takemoto M, Ota M, Nakamura T (2010) Paraspinal-approach transforaminal lumbar interbody fusion for the treatment of lumbar foraminal stenosis. J Neurosurg Spine 13(4):500–508
Haws BE, Khechen B, Guntin JA, Cardinal KL, Bohl DD, Singh K (2018) Validity of PROMIS in minimally invasive transforaminal lumbar interbody fusion: a preliminary evaluation. J Neurosurg Spine 29(1):28–33
Hsieh PC, Koski TR, O’Shaughnessy BA et al (2007) Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine 7(4):379–386
Inamasu J, Guiot BH (2006) Vascular injury and complication in neurosurgical spine surgery. Acta Neurochir (Wien) 148(4):375–387
Jenkins NW, Parrish JM, Cha EDK et al (2020) Validation of PROMIS physical function in MIS TLIF: 2-year follow-up. Spine 45(22):E1516–E1522
Jiang SD, Chen JW, Jiang LS (2012) Which procedure is better for lumbar interbody fusion: anterior lumbar interbody fusion or transforaminal lumbar interbody fusion? Arch Orthop Trauma Surg 132(9):1259–1266
Kim JS, Lee KY, Lee SH, Lee HY (2010) Which lumbar interbody fusion technique is better in terms of level for the treatment of unstable isthmic spondylolisthesis?: clinical article. J Neurosurg Spine 12(2):171–177
Kim YH, Ha KY, Rhyu KW et al (2020) Lumbar interbody fusion: techniques, pearls and pitfalls. Asian Spine J 14(5):730–741
Kumar A, Merrill RK, Overley SC et al (2019) Radiation exposure in minimally invasive transforaminal lumbar interbody fusion: the effect of the learning curve. Int J Spine Surg 13(1):39–45
Middleton K, Fish DE (2009) Lumbar spondylosis: clinical presentation and treatment approaches. Curr Rev Musculoskelet Med 2(2):94–104
Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ (2015) Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP LLIF and ALIF. J Spine Surg 1(1):2–18
Patel DV, Bawa MS, Haws BE et al (2019) PROMIS physical function for prediction of postoperative pain, narcotics consumption, and patient-reported outcomes following minimally invasive transforaminal lumbar interbody fusion. J Neurosurg Spine 30(4):476–482
Sim EM, Claydon MH, Parker RM, Malham GM (2015) Brief intraoperative heparinization and blood loss in anterior lumbar spine surgery. J Neurosurg Spine 23(3):309–313
Simon J, Longis PM, Passuti N (2017) Correlation between radiographic parameters and functional scores in degenerative lumbar and thoracolumbar scoliosis. Orthop Traumatol Surg Res 103(2):285–290
Russo F, De Salvatore S, Ambrosio L et al (2021) Does workers’ compensation status affect outcomes after lumbar spine surgery? A systematic review and meta-analysis. Int J Environ Res Public Health 18(11):6165
Nie JW, Hartman TJ, Pawlowski H, et al (2022) Impact of ambulatory setting for workers’ compensation patients undergoing one-level minimally invasive transforaminal lumbar interbody fusion and review of the literature. World Neurosurg. Published online August 7. https://doi.org/10.1016/j.wneu.2022.07.136
Author information
Authors and Affiliations
Contributions
James W. Nie: conceptualization, methodology, visualization, formal analysis, software, investigation, writing—original draft, and writing—review and editing. Timothy J. Hartman: conceptualization, methodology, visualization, formal analysis, software, investigation, writing—original draft, and writing—review and editing. Omolabake O. Oyetayo: project administration, data curation, investigation, and writing—review and editing. Keith R. MacGregor: project administration, data curation, investigation, and writing—review and editing. Eileen Zheng: project administration, data curation, investigation, and writing—review and editing. Dustin H. Massel: conceptualization, methodology, visualization, and writing—review and editing. Kern Singh: conceptualization, methodology, supervision, resources, investigation, and writing—review and editing.
Corresponding author
Ethics declarations
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Review Board (IRB) of Rush University Medical Center (ORA #14051301).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
Kern Singh, MD receives royalties from Zimmer Biomet, Stryker, RTI Surgical, Lippincott Williams and Wilkins, Thieme, Jaypee Publishing, and Slack Publishing. Kern Singh, MD owns stock in Avaz Surgical LLC and Vital 5 LLC. Kern Singh, MD holds a consulting position with Zimmer Biomet and K2M. Kern Singh, MD holds board membership with Vital 5 LLC. Kern Singh, MD is on the editorial board of Contemporary Spine Surgery. Kern Singh, MD received a research grant from the Cervical Spine Research Society. Kern Singh, MD holds board membership with TDi LLC and Minimally Invasive Spine Study Group and receives no compensation as a board member. Kern Singh, MD is on the editorial board of Orthopedics Today and Vertebral Columns and receives no compensation as a member of the editorial board. Kern Singh, MD is on the board of directors of the Cervical Spine Research Society, International Society for the Advancements of Spine Surgery, and American Academy of Orthopaedic Surgeons and receives no compensation as a member of the board of directors.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Spine - Other
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nie, J.W., Hartman, T.J., Oyetayo, O.O. et al. Recovery ratios and minimum clinically important difference for clinical outcomes in workers’ compensation recipients undergoing MIS-TLIF versus ALIF. Acta Neurochir 165, 315–323 (2023). https://doi.org/10.1007/s00701-022-05468-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05468-4