Abstract
Purpose
Observation is the first management option in asymptomatic meningiomas, but when an enlargement or mass effect is observed, surgery is indicated. This study is aimed at exploring risk factors for complications and recurrence after surgery for asymptomatic meningioma. We also examined the impact of preoperative tumor embolization, which is considered controversial.
Methods
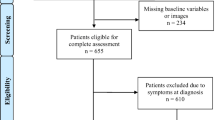
We retrospectively reviewed 109 patients with primary asymptomatic meningiomas surgically treated at our institute between April 2007 and March 2021. Patients who only had headaches as a nonspecific complaint were included in the asymptomatic group. Complications, time to recurrence, and Glasgow Outcome Scale (GOS) score were the endpoints of the study. Risk factors for complications and recurrence were explored. Moreover, the effect of the resection on nonspecific headaches was also explored.
Results
The permanent postoperative complication rate related to the surgical procedure was 1.8%. Of the total, 107 patients (98.2%) with asymptomatic meningiomas who were surgically treated achieved a GOS score of 5 1 year after the operation. Preoperative headache was present in 31 patients and improved postoperatively in 21 patients. Multivariate analysis using the Cox proportional hazard model showed that preoperative tumor embolization with > 80% resolution of tumor staining (p < 0.001) was negatively related to recurrence, whereas age (p = 0.046) and Simpson grade IV resection (p = 0.041) were positively related to recurrence.
Conclusion
Although surgery for asymptomatic meningiomas can, in many cases, be safe, it is not free of complications Thus, surgical intervention for asymptomatic meningiomas should be considered cautiously. However, more than half the patients with headaches showed improvement. Simpson grade IV resection cases should be assessed for recurrence, and preoperative tumor embolization might be effective in controlling recurrence.
Similar content being viewed by others
References
Akimoto T, Ohtake M, Miyake S, Suzuki R, Iida Y, Shimohigoshi W, Higashijima T, Nakamura T, Shimizu N, Kawasaki T, Sakata K, Yamamoto T (2022) Preoperative tumor embolization prolongs time to recurrence of meningiomas: a retrospective propensity-matched analysis. J Neurointerv Surg. https://doi.org/10.1136/neurintsurg-2022-019080
Chamoun R, Krisht KM, Couldwell WT (2011) Incidental meningiomas. Neurosurg Focus 31:E19
Clark VE, Erson-Omay EZ, Serin A, Yin J, Cotney J, Ozduman K, Avsar T, Li J, Murray PB, Henegariu O, Yilmaz S, Gunel JM, Carrion-Grant G, Yilmaz B, Grady C, Tanrikulu B, Bakircioglu M, Kaymakcalan H, Caglayan AO, Sencar L, Ceyhun E, Atik AF, Bayri Y, Bai H, Kolb LE, Hebert RM, Omay SB, Mishra-Gorur K, Choi M, Overton JD, Holland EC, Mane S, State MW, Bilguvar K, Baehring JM, Gutin PH, Piepmeier JM, Vortmeyer A, Brennan CW, Pamir MN, Kilic T, Lifton RP, Noonan JP, Yasuno K, Gunel M (2013) Genomic analysis of non-NF2 meningiomas reveals mutations in TRAF7, KLF4, AKT1, and SMO. Science 339:1077–1080
Cohen-Inbar O, Tata A, Moosa S, Lee CC, Sheehan JP (2018) Stereotactic radiosurgery in the treatment of parasellar meningiomas: long-term volumetric evaluation. J Neurosurg 128:362–372
Goldbrunner R, Stavrinou P, Jenkinson MD, Sahm F, Mawrin C, Weber DC, Preusser M, Minniti G, Lund-Johansen M, Lefranc F, Houdart E, Sallabanda K, Le Rhun E, Nieuwenhuizen D, Tabatabai G, Soffietti R, Weller M (2021) EANO guideline on the diagnosis and management of meningiomas. Neuro Oncol 23:1821–1834
Guenther F, Swozil F, Heber S, Buchfelder M, Messlinger K, Fischer MJ (2019) Pre- and postoperative headache in patients with meningioma. Cephalalgia 39:533–543
Gupta A, Xu Z, Cohen-Inbar O, Snyder MH, Hobbs LK, Li C, Nguyen QT, Sheehan JP (2019) Treatment of asymptomatic meningioma with gamma knife radiosurgery: long-term follow-up with volumetric assessment and clinical outcome. Neurosurgery 85:E889–E899
Haberg AK, Hammer TA, Kvistad KA, Rydland J, Muller TB, Eikenes L, Garseth M, Stovner LJ (2016) Incidental intracranial findings and their clinical impact; the HUNT MRI study in a general population of 1006 participants between 50–66 years. PLoS One 11:e0151080
Hashiba T, Hashimoto N, Izumoto S, Suzuki T, Kagawa N, Maruno M, Kato A, Yoshimine T (2009) Serial volumetric assessment of the natural history and growth pattern of incidentally discovered meningiomas. J Neurosurg 110:675–684
Jo KW, Kim CH, Kong DS, Seol HJ, Nam DH, Park K, Kim JH, Lee JI (2011) Treatment modalities and outcomes for asymptomatic meningiomas. Acta Neurochir (Wien) 153:62–67 (discussion 67)
Kasuya H, Kubo O, Tanaka M, Amano K, Kato K, Hori T (2006) Clinical and radiological features related to the growth potential of meningioma. Neurosurg Rev 29:293–296 (discussion 296-297)
Landriel Ibanez FA, Hem S, Ajler P, Vecchi E, Ciraolo C, Baccanelli M, Tramontano R, Knezevich F, Carrizo A (2011) A new classification of complications in neurosurgery. World Neurosurg 75:709–715 (discussion 604-711)
Law-ye B, Clarencon F, Sourour NA, Di Maria F, Jean B, Bonneville F, Biondi A, Iosif C, Navarro S, Cornu P, Chiras J (2013) Risks of presurgical embolization of feeding arteries in 137 intracranial meningeal tumors. Acta Neurochir (Wien) 155:707–714
Lee EJ, Kim JH, Park ES, Kim YH, Lee JK, Hong SH, Cho YH, Kim CJ (2017) A novel weighted scoring system for estimating the risk of rapid growth in untreated intracranial meningiomas. J Neurosurg 127:971–980
Meling TR, Da Broi M, Scheie D, Helseth E (2019) Meningiomas: skull base versus non-skull base. Neurosurg Rev 42:163–173
Miao Y, Lu X, Qiu Y, Jiang J, Lin Y (2010) A multivariate analysis of prognostic factors for health-related quality of life in patients with surgically managed meningioma. J Clin Neurosci 17:446–449
Nakasu S, Fukami T, Jito J, Nozaki K (2009) Recurrence and regrowth of benign meningiomas. Brain Tumor Pathol 26:69–72
Nicholson RA, Houle TT, Rhudy JL, Norton PJ (2007) Psychological risk factors in headache. Headache 47:413–426
Oya S, Kim SH, Sade B, Lee JH (2011) The natural history of intracranial meningiomas. J Neurosurg 114:1250–1256
Oya S, Kawai K, Nakatomi H, Saito N (2012) Significance of Simpson grading system in modern meningioma surgery: integration of the grade with MIB-1 labeling index as a key to predict the recurrence of WHO Grade I meningiomas. J Neurosurg 117:121–128
Raper DM, Starke RM, Henderson F Jr, Ding D, Simon S, Evans AJ, Jane JA Sr, Liu KC (2014) Preoperative embolization of intracranial meningiomas: efficacy, technical considerations, and complications. AJNR Am J Neuroradiol 35:1798–1804
Reinert M, Babey M, Curschmann J, Vajtai I, Seiler RW, Mariani L (2006) Morbidity in 201 patients with small sized meningioma treated by microsurgery. Acta Neurochir (Wien) 148:1257–1265 (discussion 1266)
Sanai N, Sughrue ME, Shangari G, Chung K, Berger MS, McDermott MW (2010) Risk profile associated with convexity meningioma resection in the modern neurosurgical era. J Neurosurg 112:913–919
Simpson D (1957) The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry 20:22–39
Singla A, Deshaies EM, Melnyk V, Toshkezi G, Swarnkar A, Choi H, Chin LS (2013) Controversies in the role of preoperative embolization in meningioma management. Neurosurg Focus 35:E17
Shah AH, Patel N, Raper DM, Bregy A, Ashour R, Elhammady MS, Aziz-Sultan MA, Morcos JJ, Heros RC, Komotar RJ (2013) The role of preoperative embolization for intracranial meningiomas. J Neurosurg 119:364–372
Sughrue ME, Rutkowski MJ, Aranda D, Barani IJ, McDermott MW, Parsa AT (2010) Treatment decision making based on the published natural history and growth rate of small meningiomas. J Neurosurg 113:1036–1042
Yoon N, Shah A, Couldwell WT, Kalani MYS, Park MS (2018) Preoperative embolization of skull base meningiomas: current indications, techniques, and pearls for complication avoidance. Neurosurg Focus 44:E5
Yano S, Kuratsu J, Kumamoto Brain Tumor Research G (2006) Indications for surgery in patients with asymptomatic meningiomas based on an extensive experience. J Neurosurg 105:538–543
Zeng L, Wang L, Ye F, Chen J, Lei T, Chen J (2015) Clinical characteristics of patients with asymptomatic intracranial meningiomas and results of their surgical management. Neurosurg Rev 38:481–488 (discussion 488)
Acknowledgements
We wish to thank all the staff at the participating institutions for their support in meningioma treatment, as well as the study participants and their families. We thank the staff of the Department of Biostatistics for their advice on the statistical analysis.
Author information
Authors and Affiliations
Contributions
T.A. and K.S. contributed to the conception and design of the study, acquisition of data, and analysis and interpretation of data. T.A., H.Y., S.F., R.T., T.N., M.O., T.K., and K.S. collected clinical data. T.A. wrote the draft and conducted the statistical analysis. K.S. and T.Y. supervised all aspects of this study. All the authors have read the final manuscript and approved its submission for publication. All authors attested to meeting the four ICMJE authorship criteria.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Yokohama City University Medical Center (approval number B190200012).
Consent to participate
Due to the retrospective study design, the Ethics Committee of Yokohama City University Medical Center waived the requirement for written informed consent, offering participants an opt-out option, as per the Personal Information Protection Law and National Research Ethics Guidelines in Japan.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Tumor—Meningioma
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Akimoto, T., Yoshikawa, H., Fushimi, S. et al. Surgical complications and recurrence factors for asymptomatic meningiomas: a single-center retrospective study. Acta Neurochir 165, 1345–1353 (2023). https://doi.org/10.1007/s00701-022-05420-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05420-6