Abstract
Purpose
To investigate sinovenous outflow restriction (SOR) in lateral sinus dural arteriovenous fistulas (LSDAVFs) after Gamma Knife radiosurgery (GKRS) and its association with complete obliteration.
Methods
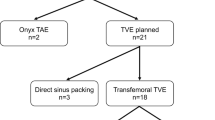
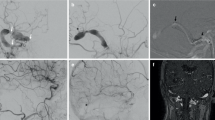
We retrospectively (1995–2019) enrolled 39 patients with LSDAVFs who had undergone GKRS alone and evaluated their angiography and magnetic resonance imaging (MRI) before and after GKRS. The LS conduits ipsilateral and contralateral to the DAVFs were scored using a 5-point scoring system, with scores ranging from 0 (total occlusion) to 4 (fully patent). SOR was defined by a conduit score < 2. Demographics, imaging features, and outcomes were compared between patients with and without ipsilateral SOR after GKRS. Logistic regression analysis was performed to estimate the odds ratio (OR) for obliteration with the imaging findings.
Results
After a median angiographic follow-up of 28 months for the 39 patients, the ipsilateral LS became more restrictive (median conduit score before and after GKRS: 2 vs. 1, p = .011). Twenty-one patients with ipsilateral SOR after GKRS had a significantly lower obliteration rate (52.4% vs. 94.4%, p = .005) than those without SOR. Follow-up SOR was independently associated with a lower obliteration rate (OR 0.05, p = .017) after adjustment for age, cortical venous reflux, and absent sinus flow void on MRI.
Conclusion
This study demonstrates a restrictive change of outflow in LSDAVFs after GKRS and a lower obliteration rate in patients with SOR. Follow-up imaging for SOR may help predict outcomes of these patients.





Similar content being viewed by others
Abbreviations
- SOR:
-
Sinovenous outflow restriction
- LSDAVF:
-
Lateral sinus dural arteriovenous fistula
- GKRS:
-
Gamma Knife radiosurgery
- OR:
-
Odds ratio
- CVR:
-
Cortical venous reflux
- DSA:
-
Quantitative digital subtraction angiography
- MRI:
-
Magnetic resonance imaging
- PPP:
-
Pseudo-phlebitic pattern
- ONS:
-
Optic nerve sheath
- RIC:
-
Radiation-induced change
References
Borden JA, Wu JK, Shucart WA (1995) A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg 82:166–179. https://doi.org/10.3171/jns.1995.82.2.0166
Canedo-Antelo M, Baleato-González S, Mosqueira AJ, Casas-Martínez J, Oleaga L, Vilanova JC, Luna-Alcalá A, García-Figueiras R (2019) Radiologic clues to cerebral venous thrombosis. Radiographics 39:1611–1628. https://doi.org/10.1148/rg.2019190015
Chen CJ, Lee CC, Ding D, Starke RM, Chivukula S, Yen CP, Moosa S, Xu Z, Pan DH, Sheehan JP (2015) Stereotactic radiosurgery for intracranial dural arteriovenous fistulas: a systematic review. J Neurosurg 122:353–362. https://doi.org/10.3171/2014.10.jns14871
Cifarelli CP, Kaptain G, Yen CP, Schlesinger D, Sheehan JP (2010) Gamma Knife radiosurgery for dural arteriovenous fistulas. Neurosurgery 67:1230–1235. https://doi.org/10.1227/NEU.0b013e3181eff6f7 (discussion 1235)
Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, Chiras J, Merland JJ (1995) Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology 194:671–680. https://doi.org/10.1148/radiology.194.3.7862961
Cognard C, Houdart E, Casasco A, Gabrillargues J, Chiras J, Merland JJ (1997) Long-term changes in intracranial dural arteriovenous fistulae leading to worsening in the type of venous drainage. Neuroradiology 39:59–66
Dmytriw AA, Schwartz ML, Cusimano MD, Mendes Pereira V, Krings T, Tymianski M, Radovanovic I, Agid R (2017) Gamma Knife radiosurgery for the treatment of intracranial dural arteriovenous fistulas. Interv Neuroradiol 23:211–220. https://doi.org/10.1177/1591019916683689
Gross BA, Albuquerque FC, Moon K, McDougall CG (2017) Evolution of treatment and a detailed analysis of occlusion, recurrence, and clinical outcomes in an endovascular library of 260 dural arteriovenous fistulas. J Neurosurg 126:1884–1893. https://doi.org/10.3171/2016.5.jns16331
Guo WY, Lee CJ, Lin CJ, Yang HC, Wu HM, Wu CC, Chung WY, Liu KD (2017) Quantifying the cerebral hemodynamics of dural arteriovenous fistula in transverse sigmoid sinus complicated by sinus stenosis: a retrospective cohort study. AJNR Am J Neuroradiol 38:132–138. https://doi.org/10.3174/ajnr.A4960
Hanakita S, Koga T, Shin M, Shojima M, Igaki H, Saito N (2012) Role of Gamma Knife surgery in the treatment of intracranial dural arteriovenous fistulas. J Neurosurg 117(Suppl):158–163. https://doi.org/10.3171/2012.7.gks12967
Hendriks EJ, Lynch J, Swaminathan SK, Nicholson P, Agid R, Radovanovic I, Pereira VM, terBrugge K, Krings T (2021) Embolization strategies for intracranial dural arteriovenous fistulas with an isolated sinus: a single-center experience in 20 patients. J Neurointerv Surg:neurintsurg-2021–017652. https://doi.org/10.1136/neurintsurg-2021-017652
Hiramatsu M, Sugiu K, Hishikawa T, Nishihiro S, Kidani N, Takahashi Y, Murai S, Date I, Kuwayama N, Satow T, Iihara K, Sakai N (2019) Results of 1940 embolizations for dural arteriovenous fistulas: Japanese Registry of Neuroendovascular Therapy (JR-NET3). J Neurosurg 1–8. https://doi.org/10.3171/2019.4.jns183458
Hu YS, Guo WY, Lin CJ, Wu HM, Luo CB, Wu CA, Lee CC, Yang HC, Liu KD, Chung WY (2020) Magnetic resonance imaging as a single diagnostic tool for verifying radiosurgery outcomes of cavernous sinus dural arteriovenous fistula. Eur J Radiol 125:108866. https://doi.org/10.1016/j.ejrad.2020.108866
Hu YS, Lin CJ, Wu HM, Guo WY, Luo CB, Wu CC, Chung WY, Liu KD, Yang HC, Lee CC (2017) Lateral sinus dural arteriovenous fistulas: sinovenous outflow restriction outweighs cortical venous reflux as a parameter associated with hemorrhage. Radiology 285:528–535. https://doi.org/10.1148/radiol.2017162594
Hung YC, Mohammed N, Kearns KN, Chen CJ, Starke RM, Kano H, Lee J, Mathieu D, Kaufmann AM, Wang WG, Grills IS, Cifarelli CP, Vargo J, Chytka T, Janouskova L, Feliciano CE, Rodriguez-Mercado R, Lunsford LD, Sheehan JP (2020) Stereotactic radiosurgery for cavernous sinus versus noncavernous sinus dural arteriovenous fistulas: outcomes and outcome predictors. Neurosurgery 86:676–684. https://doi.org/10.1093/neuros/nyz260
Kedra A, Lahlouh M, Shotar E, Chenoune Y, Boistard L, Boussac A, Shor N, Savatovsky J, Hage R, Touitou V, Nicholson P, Clarençon F, Piotin M, Blanc R, Lenck S (2021) Global collapse of the dural sinuses after venous stenting in idiopathic intracranial hypertension. J Neurol Neurosurg Psychiatry. https://doi.org/10.1136/jnnp-2020-325717
Kim BG, Yoon SM, Bae HG, Yun IG (2010) Spontaneous intracranial epidural hematoma originating from dural metastasis of hepatocellular carcinoma. J Korean Neurosurg Soc 48:166–169. https://doi.org/10.3340/jkns.2010.48.2.166
Kiyosue H, Hori Y, Okahara M, Tanoue S, Sagara Y, Matsumoto S, Nagatomi H, Mori H (2004) Treatment of intracranial dural arteriovenous fistulas: current strategies based on location and hemodynamics, and alternative techniques of transcatheter embolization. Radiographics 24:1637–1653. https://doi.org/10.1148/rg.246045026
Paddick I (2000) A simple scoring ratio to index the conformity of radiosurgical treatment plans. Technical note J Neurosurg 93(Suppl 3):219–222. https://doi.org/10.3171/jns.2000.93.supplement
Paddick I, Lippitz B (2006) A simple dose gradient measurement tool to complement the conformity index. J Neurosurg 105(Suppl):194–201. https://doi.org/10.3171/sup.2006.105.7.194
Pan DH, Lee CC, Wu HM, Chung WY, Yang HC, Lin CJ (2013) Gamma Knife radiosurgery for the management of intracranial dural arteriovenous fistulas. Acta Neurochir Suppl 116:113–119. https://doi.org/10.1007/978-3-7091-1376-9_18
Reynolds MR, Lanzino G, Zipfel GJ (2017) Intracranial dural arteriovenous fistulae. Stroke 48:1424–1431. https://doi.org/10.1161/strokeaha.116.012784
Satomi J, van Dijk JM, Terbrugge KG, Willinsky RA, Wallace MC (2002) Benign cranial dural arteriovenous fistulas: outcome of conservative management based on the natural history of the lesion. J Neurosurg 97:767–770. https://doi.org/10.3171/jns.2002.97.4.0767
Schneider BF, Eberhard DA, Steiner LE (1997) Histopathology of arteriovenous malformations after gamma knife radiosurgery. J Neurosurg 87:352–357. https://doi.org/10.3171/jns.1997.87.3.0352
Schuchardt F, Hennemuth A, Schroeder L, Meckel S, Markl M, Wehrum T, Harloff A (2017) Acute cerebral venous thrombosis: three-dimensional visualization and quantification of hemodynamic alterations using 4-dimensional flow magnetic resonance imaging. Stroke 48:671–677. https://doi.org/10.1161/strokeaha.116.015102
Starke RM, McCarthy DJ, Chen CJ, Kano H, McShane B, Lee J, Mathieu D, Vasas LT, Kaufmann AM, Wang WG, Grills IS, Patibandla MR, Cifarelli CP, Paisan G, Vargo JA, Chytka T, Janouskova L, Feliciano CE, Rodriguez-Mercado R, Tonetti DA, Lunsford LD, Sheehan JP (2019) Evaluation of stereotactic radiosurgery for cerebral dural arteriovenous fistulas in a multicenter international consortium. J Neurosurg 132:114–121. https://doi.org/10.3171/2018.8.jns181467
Starke RM, McCarthy DJ, Chen CJ, Kano H, McShane BJ, Lee J, Patibandla MR, Mathieu D, Vasas LT, Kaufmann AM, Wang WG, Grills IS, Cifarelli CP, Paisan G, Vargo J, Chytka T, Janouskova L, Feliciano CE, Sujijantarat N, Matouk C, Chiang V, Hess J, Rodriguez-Mercado R, Tonetti DA, Lunsford LD, Sheehan JP (2019) Hemorrhage risk of cerebral dural arteriovenous fistulas following Gamma Knife radiosurgery in a multicenter international consortium. J Neurosurg:1–9. https://doi.org/10.3171/2018.12.jns182208
Stolz E, Gerriets T, Bödeker RH, Hügens-Penzel M, Kaps M (2002) Intracranial venous hemodynamics is a factor related to a favorable outcome in cerebral venous thrombosis. Stroke 33:1645–1650. https://doi.org/10.1161/01.str.0000016507.94646.e6
Uranishi R, Nakase H, Sakaki T (1999) Expression of angiogenic growth factors in dural arteriovenous fistula. J Neurosurg 91:781–786. https://doi.org/10.3171/jns.1999.91.5.0781
Wu CA, Yang HC, Hu YS, Wu HM, Lin CJ, Luo CB, Guo WY, Lee CC, Liu KD, Chung WY (2020) Venous outflow restriction as a predictor of cavernous sinus dural arteriovenous fistula obliteration after Gamma Knife surgery. J Neurosurg 132:132–139. https://doi.org/10.3171/2018.9.jns182040
Wu HM, Pan DH, Chung WY, Guo WY, Liu KD, Shiau CY, Wang LW, Chen SJ (2006) Gamma Knife surgery for the management of intracranial dural arteriovenous fistulas. J Neurosurg 105(Suppl):43–51. https://doi.org/10.3171/sup.2006.105.7.43
Zhu Y, Lawton MT, Du R, Shwe Y, Chen Y, Shen F, Young WL, Yang GY (2006) Expression of hypoxia-inducible factor-1 and vascular endothelial growth factor in response to venous hypertension. Neurosurgery 59:687–696. https://doi.org/10.1227/01.neu.0000228962.68204.cf (discussion 687-696)
Acknowledgements
The authors would like to thank Hsin-Yi Huang (Biostatistics Task Force, Taipei Veterans General Hospital) for providing statistical analysis assistance. This manuscript was edited by Wallace Academic Editing.
Funding
This study was funded by Taipei Veterans General Hospital (grant number: V110C-056) and Taiwan’s Ministry of Science and Technology (grant number: MOST-109–2628-B-010–014-MY2).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures in studies involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee (Department of Research Programs Walter Reed National Military Medical Center Institutional Review Board) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent was not required.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Vascular Neurosurgery
Rights and permissions
About this article
Cite this article
Hu, YS., Lee, CC., Wu, CA. et al. Sinovenous outflow in lateral sinus dural arteriovenous fistulas after stereotactic radiosurgery: a retrospective longitudinal imaging study. Acta Neurochir 164, 2409–2418 (2022). https://doi.org/10.1007/s00701-022-05310-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05310-x