Abstract
Background
Meningiomas have vascular supply from the tumor attachment on the dura mater. Gamma Knife radiosurgery (GKS) is known to have a vascular obliterating effect. This study aims to determine the benefits of high-dose irradiation to the tumor attachment compared to conventional dose planning in the long-term control of tumor growth with GKS.
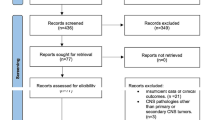
Methods
Two different dose plannings were retrospectively compared in 75 patients with meningioma treated with GKS as a primary treatment. Forty-three patients were irradiated over 20 Gy to the tumor attachment. The remaining 32 patients were treated with conventional-dose planning. Tumor growth control, reduction of enhancement on the gadolinium-enhanced magnetic resonance imaging (MRI), and neurological status were retrospectively assessed.
Results
The maximum dose on the tumor attachment was significantly higher in the high-dose group (23 Gy) than in the conventional group (16 Gy). The tumor margin was irradiated with the median of the 50% isodose line in both groups. The prescription doses resulted in 14 Gy and 12 Gy, respectively. The tumor control rate achieved 91% in both groups during the median follow-up period of 54 months. A decrease of enhancement on follow-up MRI was noted in one patient in each group. Kaplan–Meier analysis revealed no statistical difference in the progression-free survival between the two groups. The number of patients with improved neurological status showed no statistical difference.
Conclusions
No obvious benefit of high-dose irradiation to the tumor attachment and margin was found in tumor control and neurological status in the long term.



Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
References
Fabrikant JI, Lyman JT, Hosobuchi Y (1984) Stereotactic heavy-ion Bragg peak radiosurgery for intra-cranial vascular disorders: method for treatment of deep arteriovenous malformations. Br J Radiol 57:479–490. https://doi.org/10.1259/0007-1285-57-678-479
Hasegawa H, Yamamoto M, Shin M, Barfod BE (2019) Gamma Knife radiosurgery for brain vascular malformations: current evidence and future tasks. Ther Clin Risk Manag 15:1351–1367. https://doi.org/10.2147/tcrm.S200813
Hayashi M, Chernov M, Tamura N, Izawa M, Muragaki Y, Iseki H, Okada Y, Takakura K (2011) Gamma knife robotic microradiosurgery for benign skull base meningiomas: tumor shrinkage may depend on the amount of radiation energy delivered per lesion volume (unit energy). Stereotact Funct Neurosurg 89:6–16. https://doi.org/10.1159/000321184
Inoue HK (2006) Long-term results of Gamma Knife surgery for arteriovenous malformations: 10- to 15-year follow up in patients treated with lower doses. J Neurosurg 105(Suppl):64–68. https://doi.org/10.3171/sup.2006.105.7.64
Iwai Y, Yamanaka K, Ikeda H (2008) Gamma Knife radiosurgery for skull base meningioma: long-term results of low-dose treatment. J Neurosurg 109:804–810. https://doi.org/10.3171/jns/2008/109/11/0804
Jumah F, Narayan V, Samara A, Quinoa TR, Dossani RH, Gupta G, Nanda A (2020) Efficacy and safety of gamma knife radiosurgery for posterior cranial fossa meningioma: a systematic review. Neurosurg Rev 43:1089–1099. https://doi.org/10.1007/s10143-019-01144-x
Kim JW, Kim DG, Se YB, Kim SK, Chung HT, Paek SH, Jung HW (2017) Gamma knife radiosurgery for petroclival meningioma: long-term outcome and failure pattern. Stereotact Funct Neurosurg 95:209–215. https://doi.org/10.1159/000475763
Lunsford LD, Kondziolka D, Flickinger JC, Bissonette DJ, Jungreis CA, Maitz AH, Horton JA, Coffey RJ (1991) Stereotactic radiosurgery for arteriovenous malformations of the brain. J Neurosurg 75:512–524. https://doi.org/10.3171/jns.1991.75.4.0512
Major O, Szeifert GT, Kemeny AA (2007) Physiological and pathological observations on rat middle cerebral arteries and human AVM tissue cultures following single high-dose gamma irradiation. Prog Neurol Surg 20:375–387. https://doi.org/10.1159/000100179
Pan DH, Guo WY, Chung WY, Shiau CY, Chang YC, Wang LW (2000) Gamma knife radiosurgery as a single treatment modality for large cerebral arteriovenous malformations. J Neurosurg 93(Suppl 3):113–119. https://doi.org/10.3171/jns.2000.93.supplement
Park KJ, Kano H, Iyer A, Liu X, Tonetti DA, Lehocky C, Faramand A, Niranjan A, Flickinger JC, Kondziolka D, Lunsford LD (2018) Gamma Knife stereotactic radiosurgery for cavernous sinus meningioma: long-term follow-up in 200 patients. Journal of neurosurgery:1–10. https://doi.org/10.3171/2018.2.Jns172361
Pechlivanis I, Wawrzyniak S, Engelhardt M, Schmieder K (2011) Evidence level in the treatment of meningioma with focus on the comparison between surgery versus radiotherapy. A review Journal of neurosurgical sciences 55:319–328
Sadik ZHA, Lie ST, Leenstra S, Hanssens PEJ (2018) Volumetric changes and clinical outcome for petroclival meningiomas after primary treatment with Gamma Knife radiosurgery. J Neurosurg 129:1623–1629. https://doi.org/10.3171/2017.7.Jns17380
Shin M, Maruyama K, Kurita H, Kawamoto S, Tago M, Terahara A, Morita A, Ueki K, Takakura K, Kirino T (2004) Analysis of nidus obliteration rates after gamma knife surgery for arteriovenous malformations based on long-term follow-up data: the University of Tokyo experience. J Neurosurg 101:18–24. https://doi.org/10.3171/jns.2004.101.1.0018
Snell JW, Sheehan J, Stroila M, Steiner L (2006) Assessment of imaging studies used with radiosurgery: a volumetric algorithm and an estimation of its error. Technical note. J Neurosurg 104:157–162. https://doi.org/10.3171/jns.2006.104.1.157
Starke RM, Przybylowski CJ, Sugoto M, Fezeu F, Awad AJ, Ding D, Nguyen JH, Sheehan JP (2015) Gamma Knife radiosurgery of large skull base meningiomas. J Neurosurg 122:363–372. https://doi.org/10.3171/2014.10.Jns14198
Steiner L, Leksell L, Greitz T, Forster DM, Backlund EO (1972) Stereotaxic radiosurgery for cerebral arteriovenous malformations. Report of a case. Acta Chir Scand 138:459–464
Wu HM, Pan DH, Chung WY, Guo WY, Liu KD, Shiau CY, Wang LW, Chen SJ (2006) Gamma Knife surgery for the management of intracranial dural arteriovenous fistulas. J Neurosurg 105(Suppl):43–51. https://doi.org/10.3171/sup.2006.105.7.43
Yamamoto Y, Coffey RJ, Nichols DA, Shaw EG (1995) Interim report on the radiosurgical treatment of cerebral arteriovenous malformations. The influence of size, dose, time, and technical factors on obliteration rate. J Neurosurg 83:832–837. https://doi.org/10.3171/jns.1995.83.5.0832
Acknowledgements
We thank Ms. Satomi Fujimura and Ms. Yasuko Noda for the assistance with data collection.
Author information
Authors and Affiliations
Contributions
Conception and design: Inoue. Drafting of the article: Inoue and Goto. Treating the patients: Inoue, Shima, and Hirai. Analyzing the data: Inoue, Shima, and Shitara. Figures: Inoue and Shima. Critically revising the article: Matsuda and Suzuki.
Corresponding author
Ethics declarations
Statement of Ethics
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional committee and national research committee. This study is in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from all individual participants in this study. All data identifying the patients were anonymized. This study protocol was reviewed and approved by the ethics committee of Koto Memorial Hospital (Shiga, Japan), approval number 2012–12.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Tumor.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Inoue, T., Goto, Y., Shima, A. et al. Effect of high-dose delivery on the attachment of meningiomas in Gamma Knife surgery: a retrospective study. Acta Neurochir 164, 2465–2471 (2022). https://doi.org/10.1007/s00701-022-05291-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05291-x