Abstract
Background
Controlled hypotension is an important tool in the open treatment of complex intracranial aneurysms. Of the available methodologies, rapid ventricular pacing (RVP) provides titratable, sustained hypotension with a relatively safe profile.
Method
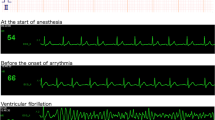
We report the case of a 63-year-old woman who underwent a combined subfrontal and subtemporal approach for clipping of anterior communicating artery and basilar apex aneurysms. RVP was used during initial dissection of the basilar apex aneurysm and perforators but caused uncontrolled ventricular tachycardia requiring synchronized defibrillation. After restoration of hemodynamic stability, the aneurysm was uneventfully clipped.
Conclusion
Preparation for unstable cardiac arrhythmias is needed with RVP.



Similar content being viewed by others
Data availability
All of the data are presented in the submitted paper.
Code availability
Not applicable.
References
Guinn NR, McDonagh DL, Borel CO, Wright DR, Zomorodi AR, Powers CJ, Warner DS, Lam AM, Britz GW (2011) Adenosine-induced transient asystole for intracranial aneurysm surgery: a retrospective review. J Neurosurg Anesthesiol 23:35–40. https://doi.org/10.1097/ANA.0b013e3181ef2b11
Hockley A, Tso MK, Almekhlafi MA, Lodha AK, Clegg R, Luntley J, Eesa M, Wong JH (2018) Rapid cardiac ventricular pacing to facilitate embolization of vein of Galen malformations: technical note. J Neurosurg Pediatr 23:86–91. https://doi.org/10.3171/2018.7.PEDS1852
Intarakhao P, Thiarawat P, Rezai Jahromi B, Kozyrev DA, Teo MK, Choque-Velasquez J, Luostarinen T, Hernesniemi J (2018) Adenosine-induced cardiac arrest as an alternative to temporary clipping during intracranial aneurysm surgery. J Neurosurg 129:684–690. https://doi.org/10.3171/2017.5.JNS162469
Konczalla J, Platz J, Fichtlscherer S, Mutlak H, Strouhal U, Seifert V (2018) Rapid ventricular pacing for clip reconstruction of complex unruptured intracranial aneurysms: results of an interdisciplinary prospective trial. J Neurosurg 128:1741–1752. https://doi.org/10.3171/2016.11.JNS161420
Lawton MT, Raudzens PA, Zabramski JM, Spetzler RF (1998) Hypothermic circulatory arrest in neurovascular surgery: evolving indications and predictors of patient outcome. Neurosurgery 43:10–20; discussion 20–21. https://doi.org/10.1097/00006123-199807000-00009
Meling TR, Lavé A (2019) What are the options for cardiac standstill during aneurysm surgery? A systematic review. Neurosurg Rev 42:843–852. https://doi.org/10.1007/s10143-019-01183-4
Saldien V, Menovsky T, Rommens M, Van der Steen G, Van Loock K, Vermeersch G, Mott C, Bosmans J, De Ridder D, Maas AI (2012) Rapid ventricular pacing for flow arrest during cerebrovascular surgery: revival of an old concept. Neurosurgery 70:270–275. https://doi.org/10.1227/NEU.0b013e318236d84a
Winkler EA, Lee A, Yue JK, Raygor KP, Rutledge WC, Rubio RR, Josephson SA, Berger MS, Raper DMS, Abla AA (2021) Endovascular embolization versus surgical clipping in a single surgeon series of basilar artery aneurysms: a complementary approach in the endovascular era. Acta Neurochir (Wien) 163:1527–1540. https://doi.org/10.1007/s00701-021-04803-5
Author information
Authors and Affiliations
Contributions
Henson: data curation, manuscript writing; Rennert: data curation, manuscript writing and editing; Budohoski: manuscript editing; Couldwell: conceptualization, manuscript writing and editing, project administration, and resources.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Ethics approval was waived by the Institutional Review Board of the University of Utah for reporting a single case.
Consent to participate
The patient’s family provided consent for participation in the case and video.
Consent for publication
The patient’s family provided consent for publication of the case and video.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
- Controlled hypotension can aid aneurysm dissection, assist with intraoperative rupture, and limit the need for temporary clips.
- Techniques for controlled hypotension include adenosine, RVP, and deep hypothermic circulatory arrest with cardiac bypass.
- Transvenous RVP can provide minutes of titratable hypotension.
- Previously reported rare cardiac complications with RVP for cerebral aneurysm surgery include transient troponin increases, supraventricular tachycardia requiring cardioversion, and self-resolving ventricular fibrillation.
- Other options for induced hypotension include adenosine (short window [< 1 min] and variable dose–response across patients), and deep hypothermic circulatory arrest with cardiac bypass (longest and most dramatic vascular collapse but significant morbidity).
- When using RVP, preoperative cardiac clearance and preparation for unstable rhythms with external defibrillator pads is important.
- Operative positioning should allow for chest compressions when RVP is planned.
- The use of RVP for longer than 100 s at a time should be avoided.
- In consultation with cardiology, use of alternative strategies to RVP may be considered in patients with conduction abnormalities.
- In addition to the known risks associated with aneurysm surgery, discussion of the small risk of cardiac arrest and ischemic brain injury with RVP should be held.
This article is part of the Topical Collection on Vascular Neurosurgery—Aneurysms
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 0:09 – Patient history0:16 – Preoperative imaging0:43 – Surgical plan1:01 – Patient positioning1:09 – Surgical procedure1:55 – Clipping of Acomm aneurysm3:13 – Episode of uncontrolled ventricular tachycardia with RVP3:51 – Clipping of basilar apex aneurysm4:52 – Postoperative imaging(MP4 483543 KB)
Rights and permissions
About this article
Cite this article
Henson, J.C., Rennert, R.C., Budohoski, K.P. et al. Unstable ventricular tachycardia requiring defibrillation from rapid ventricular pacing during basilar apex aneurysm clipping. Acta Neurochir 164, 537–541 (2022). https://doi.org/10.1007/s00701-022-05125-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05125-w