Abstract
Background
Childhood thalamopeduncular gliomas arise at the interface of the thalamus and cerebral peduncle. The optimal treatment is total resection but not at the cost of neurological function. We present long-term clinical and oncological outcomes of maximal safe resection.
Methods
Retrospective review of prospectively collected data: demography, symptomatology, imaging, extent of resection, surgical complications, histology, functional and oncological outcome.
Results
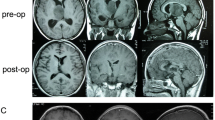
During 16-year period (2005–2020), 21 patients were treated at our institution. These were 13 girls and 8 boys (mean age 7.6 years). Presentation included progressive hemiparesis in 9 patients, raised intracranial pressure in 9 patients and cerebellar symptomatology in 3 patients. The tumour was confined to the thalamus in 6 cases. Extent of resection was judged on postoperative imaging as total (6), near-total (6) and less extensive (9). Surgical complications included progression of baseline neurological status in 6 patients, and 5 of these gradually improved to preoperative status. All tumours were classified as low-grade gliomas. Disease progression was observed in 9 patients (median progression-free survival 7.3 years). At last follow-up (median 6.1 years), all patients were alive, median Lansky score of 90. Seven patients were without evidence of disease, 6 had stable disease, 7 stable following progression and 1 had progressive disease managed expectantly.
Conclusion
Paediatric patients with low-grade thalamopeduncular gliomas have excellent long-term functional and oncological outcomes when gross total resection is not achievable. Surgery should aim at total resection; however, neurological function should not be endangered due to excellent chance for long-term survival.





Similar content being viewed by others
Availability of data and materials
Available from the corresponding author upon reasonable request.
Code availability
Not applicable.
Abbreviations
- cDNA:
-
Complementary deoxyribonucleic acid
- CST:
-
Cortico-spinal tract
- DNA:
-
Deoxyribonucleic acid
- EOR:
-
Extent of resection
- ETV:
-
Endoscopic third ventriculostomy
- FLAIR:
-
Fluid-attenuated inversion recovery
- GTR:
-
Gross total resection
- LGG:
-
Low-grade glioma
- MCS:
-
Milan Complexity Scale
- MRI:
-
Magnetic resonance imaging
- NTR:
-
Near total resection
- OS:
-
Overall survival
- PCR:
-
Polymerase chain reaction
- PFS:
-
Progression-free survival
- PR:
-
Partial resection
- RNA:
-
Ribonucleic acid
- RT PCR:
-
Reverse transcriptase polymerase chain reaction
- STR:
-
Subtotal resection
References
Bandopadhayay P, Bergthold G, London WB, Goumnerova LC, Morales La Madrid A, Marcus KJ, Guo D, Ullrich NJ, Robison NJ, Chi SN et al (2014) Long-term outcome of 4,040 children diagnosed with pediatric low-grade gliomas: an analysis of the Surveillance Epidemiology and End Results (SEER) database. Pediatr Blood Cancer 61:1173–1179. https://doi.org/10.1002/pbc.24958
Baroncini M, Vinchon M, Minéo JF, Pichon F, Francke JP, Dhellemmes P (2007) Surgical resection of thalamic tumors in children: approaches and clinical results. Childs Nerv Syst 23:753–760. https://doi.org/10.1007/s00381-007-0299-4
Bilginer B, Narin F, Işıkay I, Oguz KK, Söylemezoglu F, Akalan N (2014) Thalamic tumors in children. Childs Nerv Syst 30:1493–1498. https://doi.org/10.1007/s00381-014-2420-9
Broadway SJ, Ogg RJ, Scoggins MA, Sanford R, Patay Z, Boop FA (2011) Surgical management of tumors producing the thalamopeduncular syndrome of childhood. J Neurosurg Pediatr 7:589–595. https://doi.org/10.3171/2011.4.Peds119
Celtikci E, Celtikci P, Fernandes-Cabral DT, Ucar M, Fernandez-Miranda JC, Borcek AO (2017) High-definition fiber tractography in evaluation and surgical planning of thalamopeduncular pilocytic astrocytomas in pediatric population: case series and review of literature. World Neurosurg 98:463–469. https://doi.org/10.1016/j.wneu.2016.11.061
Cheek WR, Taveras JM (1966) Thalamic tumors. J Neurosurg 24:505–513. https://doi.org/10.3171/jns.1966.24.2.0505
Cinalli G, Aguirre DT, Mirone G, Ruggiero C, Cascone D, Quaglietta L, Aliberti F, Santi SD, Buonocore MC, Nastro A et al (2018) Surgical treatment of thalamic tumors in children. J Neurosurg Pediatr 21:247–257. https://doi.org/10.3171/2017.7.Peds16463
Cuccia V, Monges J (1997) Thalamic tumors in children. Childs Nerv Syst 13: 514–520; discussion 521 https://doi.org/10.1007/s003810050128
Douw L, Klein M, Fagel SS, van den Heuvel J, Taphoorn MJ, Aaronson NK, Postma TJ, Vandertop WP, Mooij JJ, Boerman RH et al (2009) Cognitive and radiological effects of radiotherapy in patients with low-grade glioma: long-term follow-up. Lancet Neurol 8:810–818. https://doi.org/10.1016/s1474-4422(09)70204-2
Fangusaro J, Witt O, Hernáiz Driever P, Bag AK, de Blank P, Kadom N, Kilburn L, Lober RM, Robison NJ, Fisher MJ et al (2020) Response assessment in paediatric low-grade glioma: recommendations from the Response Assessment in Pediatric Neuro-Oncology (RAPNO) working group. Lancet Oncol 21:e305–e316. https://doi.org/10.1016/s1470-2045(20)30064-4
Fedorov A, Beichel R, Kalpathy-Cramer J, Finet J, Fillion-Robin JC, Pujol S, Bauer C, Jennings D, Fennessy F, Sonka M et al (2012) 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn Reson Imaging 30:1323–1341. https://doi.org/10.1016/j.mri.2012.05.001
Ferroli P, Broggi M, Schiavolin S, Acerbi F, Bettamio V, Caldiroli D, Cusin A, La Corte E, Leonardi M, Raggi A et al (2015) Predicting functional impairment in brain tumor surgery: the Big Five and the Milan Complexity Scale. Neurosurg Focus 39:E14. https://doi.org/10.3171/2015.9.Focus15339
Gunny RS, Hayward RD, Phipps KP, Harding BN, Saunders DE (2005) Spontaneous regression of residual low-grade cerebellar pilocytic astrocytomas in children. Pediatr Radiol 35:1086–1091. https://doi.org/10.1007/s00247-005-1546-z
Hirose G, Lombroso CT, Eisenberg H (1975) Thalamic tumors in childhood. Clinical, laboratory, and therapeutic considerations. Arch Neurol 32:740–744. https://doi.org/10.1001/archneur.1975.00490530062005
Hoffman HJ, Soloniuk DS, Humphreys RP, Drake JM, Becker LE, De Lima BO, Piatt JH Jr (1993) Management and outcome of low-grade astrocytomas of the midline in children: a retrospective review. Neurosurgery 33:964–971. https://doi.org/10.1227/00006123-199312000-00002
Johnson DR, Brown PD, Galanis E, Hammack JE (2012) Pilocytic astrocytoma survival in adults: analysis of the Surveillance, Epidemiology, and End Results Program of the National Cancer Institute. J Neurooncol 108:187–193. https://doi.org/10.1007/s11060-012-0829-0
Karschnia P, Vogelbaum MA, van den Bent M, Cahill DP, Bello L, Narita Y, Berger MS, Weller M, Tonn JC (2021) Evidence-based recommendations on categories for extent of resection in diffuse glioma. Eur J Cancer 149:23–33. https://doi.org/10.1016/j.ejca.2021.03.002
Lansky SB, List MA, Lansky LL, Ritter-Sterr C, Miller DR (1987) The measurement of performance in childhood cancer patients. Cancer 60:1651–1656. https://doi.org/10.1002/1097-0142(19871001)60:7%3c1651::aid-cncr2820600738%3e3.0.co;2-j
Lassaletta A, Zapotocky M, Mistry M, Ramaswamy V, Honnorat M, Krishnatry R, Guerreiro Stucklin A, Zhukova N, Arnoldo A, Ryall S et al (2017) Therapeutic and prognostic implications of BRAF V600E in pediatric low-grade gliomas. J Clin Oncol 35:2934–2941. https://doi.org/10.1200/jco.2016.71.8726
Lee RP, Foster KA, Lillard JC, Klimo P Jr, Ellison DW, Orr B, Boop FA (2017) Surgical and molecular considerations in the treatment of pediatric thalamopeduncular tumors. J Neurosurg Pediatr 20:247–255. https://doi.org/10.3171/2017.4.Peds16668
Mistry M, Zhukova N, Merico D, Rakopoulos P, Krishnatry R, Shago M, Stavropoulos J, Alon N, Pole JD, Ray PN et al (2015) BRAF mutation and CDKN2A deletion define a clinically distinct subgroup of childhood secondary high-grade glioma. J Clin Oncol 33:1015–1022. https://doi.org/10.1200/jco.2014.58.3922
Moshel YA, Link MJ, Kelly PJ (2007) Stereotactic volumetric resection of thalamic pilocytic astrocytomas. Neurosurgery 61: 66–75; discussion 75 Doi https://doi.org/10.1227/01.neu.0000279725.13521.a3
Nobre L, Zapotocky M, Ramaswamy V, Ryall S, Bennett J, Alderete D, Balaguer Guill J, Baroni L, Bartels U, Bavle Aet al (2020) Outcomes of BRAF V600E pediatric gliomas treated with targeted BRAF inhibition. JCO Precis Oncol 4https://doi.org/10.1200/po.19.00298
Ozek MM, Türe U (2002) Surgical approach to thalamic tumors. Childs Nerv Syst 18:450–456. https://doi.org/10.1007/s00381-002-0608-x
Puget S, Crimmins DW, Garnett MR, Grill J, Oliveira R, Boddaert N, Wray A, Lelouch-Tubiana A, Roujeau T, Di Rocco F et al (2007) Thalamic tumors in children: a reappraisal. J Neurosurg 106:354–362. https://doi.org/10.3171/ped.2007.106.5.354
Ramaswamy V, Hielscher T, Mack SC, Lassaletta A, Lin T, Pajtler KW, Jones DT, Luu B, Cavalli FM, Aldape K et al (2016) Therapeutic impact of cytoreductive surgery and irradiation of posterior fossa ependymoma in the molecular era: a retrospective multicohort analysis. J Clin Oncol 34:2468–2477. https://doi.org/10.1200/jco.2015.65.7825
Rangel-Castilla L, Spetzler RF (2015) The 6 thalamic regions: surgical approaches to thalamic cavernous malformations, operative results, and clinical outcomes. J Neurosurg 123:676–685. https://doi.org/10.3171/2014.11.Jns14381
Rees J, Watt H, Jäger HR, Benton C, Tozer D, Tofts P, Waldman A (2009) Volumes and growth rates of untreated adult low-grade gliomas indicate risk of early malignant transformation. Eur J Radiol 72:54–64. https://doi.org/10.1016/j.ejrad.2008.06.013
Renedo D, Ferraro F, Johnson AR, Argañaraz R, Giovannini S, Zabala JP, Zemma E, Mantese B (2021) Thalamic tumors in children: case series from our institution and literature review. Childs Nerv Syst 37:457–463. https://doi.org/10.1007/s00381-020-04830-0
Renzi S, Michaeli O, Ramaswamy V, Huang A, Stephens D, Maguire B, Tabori U, Bouffet E, Bartels U (2020) Causes of death in pediatric neuro-oncology: the sickkids experience from 2000 to 2017. J Neurooncol 149:181–189. https://doi.org/10.1007/s11060-020-03590-w
Rozen WM, Joseph S, Lo PA (2008) Spontaneous regression of low-grade gliomas in pediatric patients without neurofibromatosis. Pediatr Neurosurg 44:324–328. https://doi.org/10.1159/000134925
Ryall S, Zapotocky M, Fukuoka K, Nobre L, Guerreiro Stucklin A, Bennett J, Siddaway R, Li C, Pajovic S, Arnoldo A et al (2020) Integrated molecular and clinical analysis of 1,000 pediatric low-grade gliomas. Cancer Cell 37:569-583.e565. https://doi.org/10.1016/j.ccell.2020.03.011
Ryu HH, Jung TY, Lee GJ, Lee KH, Jung SH, Jung S, Baek HJ (2015) Differences in the clinical courses of pediatric and adult pilocytic astrocytomas with progression: a single-institution study. Childs Nerv Syst 31:2063–2069. https://doi.org/10.1007/s00381-015-2887-z
Serra C, Türe H, Yaltırık CK, Harput MV, Türe U (2020) Microneurosurgical removal of thalamic lesions: surgical results and considerations from a large, single-surgeon consecutive series. J Neurosurg: 1-11 https://doi.org/10.3171/2020.6.Jns20524
Smrčka M, Brichtová E, Mackerle Z, Juráň V, Přibáň V (2015) Surgical approaches to thalamic tumors. Cesk Slov Neurol N 78:172–180
Steinbok P, Gopalakrishnan CV, Hengel AR, Vitali AM, Poskitt K, Hawkins C, Drake J, Lamberti-Pasculli M, Ajani O, Hader W et al (2016) Pediatric thalamic tumors in the MRI era: a Canadian perspective. Childs Nerv Syst 32:269–280. https://doi.org/10.1007/s00381-015-2968-z
Tian Y, Rich BE, Vena N, Craig JM, Macconaill LE, Rajaram V, Goldman S, Taha H, Mahmoud M, Ozek M et al (2011) Detection of KIAA1549-BRAF fusion transcripts in formalin-fixed paraffin-embedded pediatric low-grade gliomas. J Mol Diagn 13:669–677. https://doi.org/10.1016/j.jmoldx.2011.07.002
Upadhyaya SA, Koschmann C, Muraszko K, Venneti S, Garton HJ, Hamstra DA, Maher CO, Betz BL, Brown NA, Wahl D et al (2017) Brainstem low-grade gliomas in children-excellent outcomes with multimodality therapy. J Child Neurol 32:194–203. https://doi.org/10.1177/0883073816675547
Villarejo F, Amaya C, Pérez Díaz C, Pascual A, Alvarez Sastre C, Goyenechea F (1994) Radical surgery of thalamic tumors in children. Childs Nerv Syst 10:111–114. https://doi.org/10.1007/bf00302774
Wisoff JH, Sanford RA, Heier LA, Sposto R, Burger PC, Yates AJ, Holmes EJ, Kun LE (2011) Primary neurosurgery for pediatric low-grade gliomas: a prospective multi-institutional study from the Children’s Oncology Group. Neurosurgery 68: 1548–1554; discussion 1554–1545 Doi https://doi.org/10.1227/NEU.0b013e318214a66e
Youland RS, Brown PD, Giannini C, Parney IF, Uhm JH, Laack NN (2013) Adult low-grade glioma: 19-year experience at a single institution. Am J Clin Oncol 36:612–619. https://doi.org/10.1097/COC.0b013e31825d580a
Zapotocky M, Beera K, Adamski J, Laperierre N, Guger S, Janzen L, Lassaletta A, Figueiredo Nobre L, Bartels U, Tabori U et al (2019) Survival and functional outcomes of molecularly defined childhood posterior fossa ependymoma: cure at a cost. Cancer 125:1867–1876. https://doi.org/10.1002/cncr.31995
Zattra CM, Broggi M, Schiavolin S, Schiariti M, Acerbi F, Esposito S, de Laurentis C, Broggi G, Ferroli P (2021) Surgical outcome and indicators of postoperative worsening in intra-axial thalamic and posterior fossa pediatric tumors: preliminary results from a single tertiary referral center cohort. Interdisciplinary Neurosurgery 24:101054. https://doi.org/10.1016/j.inat.2020.101054
Zhang J, Wu G, Miller CP, Tatevossian RG, Dalton JD, Tang B, Orisme W, Punchihewa C, Parker M, Qaddoumi I et al (2013) Whole-genome sequencing identifies genetic alterations in pediatric low-grade gliomas. Nat Genet 45:602–612. https://doi.org/10.1038/ng.2611
Funding
This work was supported by the Grant Agency of Charles University, Prague PRIMUS/19/MED/06 and Research Project of the Ministry of Health of the Czech Republic No 00064203.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Vladimir Beneš 3rd, Michal Zápotocký, Petr Libý, Jakub Táborský, Jana Blažková Jr., Jana Blažková Sr., David Sumerauer, Adéla Mišove, Ivana Perníková, Martin Kynčl, Lenka Krsková, Miroslav Koblížek, Josef Zámečník, Ondřej Bradáč and Michal Tichý. The first draft of the manuscript was written by Vladimír Beneš 3rd and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was waived by the local Ethics Committee of Second Faculty of Medicine, Charles University and Motol University Hospital in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Comments
This manuscript describes a series of 21 children with thalamic and thalamopeduncular low grade gliomas treated between 2005 and 2020. The authors provide a good description of their patients and their surgical technique, emphasising their choice of operative approach, their use of adjunctive methods to maximise surgical safety and the fact that a good long term neurological and oncological outcome does not necessarily require a complete resection of the tumour. The authors have addressed comments from the initial reviewers. Although other similar series have been described, these are rare tumours and a relatively large well-described and well-managed series such as this one is still a useful addition to the literature. Within the current paradigms of chemotherapy and targeted therapy for low grade gliomas, their emphasis on surgical safety rather than complete resection is important. This is not always clarified in surgical series.
Kristian Aquilina
London, UK
QueryPrevious presentation: Accepted in part as an ePoster presentation for EANS 2021 Virtual Congress, October 03–07, 2021
This article is part of the Topical Collection on Pediatric Neurosurgery
Rights and permissions
About this article
Cite this article
Beneš, V., Zápotocký, M., Libý, P. et al. Survival and functional outcomes in paediatric thalamic and thalamopeduncular low grade gliomas. Acta Neurochir 164, 1459–1472 (2022). https://doi.org/10.1007/s00701-021-05106-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-021-05106-5