Abstract
Background
Outcomes for octogenarians and nonagenarians after an aneurysmal subarachnoid hemorrhage (aSAH) are particularly ominous, with mortality rates well above 50%. The present analysis examines the neurologic outcomes of patients ≥ 80 years of age treated for aSAH.
Method
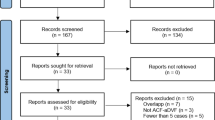
A retrospective review was performed of all aSAH patients treated at Barrow Neurological Institute from January 1, 2003, to July 31, 2019. Patients were placed in 2 groups by age, < 80 vs ≥ 80 years. The ≥ 80-year-old group of octogenarians and nonagenarians was subsequently analyzed to compare treatment modalities. Poor neurologic outcome was defined as a modified Rankin Scale (mRS) score of > 2.
Results
During the study period, 1418 patients were treated for aSAH. The mean (standard deviation) age was 55.1 (13.6) years, the mean follow-up was 24.6 (40.0) months, and the rate of functional independence (mRS 0–2) at follow-up was 54% (751/1395). Logistic regression analysis found increasing age strongly associated with declining functional independence (R2 = 0.929, p < 0.001). Forty-three patients ≥ 80 years old were significantly more likely to be managed endovascularly than with open microsurgery (67% [n = 29] vs 33% [n = 14], p < 0.001). Compared with younger patients, those ≥ 80 years old had an increased risk of mortality and poor neurologic outcomes at follow-up. In the ≥ 80-year-old group, only 4 patients had good outcomes; none of the 4 had preexisting comorbidities, and all 4 were treated endovascularly.
Conclusions
Age is a significant prognostic indicator of functional outcomes and mortality after aSAH. Most octogenarians and nonagenarians with aSAH will become severely disabled or die.

Similar content being viewed by others
Abbreviations
- aSAH:
-
Aneurysmal subarachnoid hemorrhage
- BRAT:
-
Barrow Ruptured Aneurysm Trial
- CCI:
-
Charlson Comorbidity Index
- DCI:
-
Delayed cerebral ischemia
- HH:
-
Hunt and Hess
- mRS:
-
Modified Rankin Scale
- PBRAT:
-
Post-Barrow Ruptured Aneurysm Trial
References
Alleyne CH Jr (2010) Aneurysmal subarachnoid hemorrhage: have outcomes really improved? Neurology 74:1486–1487
Boecher-Schwarz HG, Ungersboeck K, Ulrich P, Fries G, Wild A, Perneczky A (1994) Transcranial Doppler diagnosis of cerebral vasospasm following subarachnoid haemorrhage: correlation and analysis of results in relation to the age of patients. Acta Neurochir (Wien) 127:32–36
Catapano JS, Fredrickson VL, Fujii T, Cole TS, Koester SW, Baranoski JF, Cavalcanti DD, Wilkinson DA, Majmundar N, Lang MJ, Lawton MT, Ducruet AF, Albuquerque FC (2020) Complications of femoral versus radial access in neuroendovascular procedures with propensity adjustment. J Neurointerv Surg 12:611–615
Catapano JS, Louie CE, Lang MJ, DiDomenico JD, Whiting AC, Labib MA, Cole TS, Fredrickson VL, Cavalcanti DD, Lawton MT (2020) Outcomes in a case series of elderly patients with aneurysmal subarachnoid hemorrhages in the Barrow Ruptured Aneurysm Trial (BRAT). World Neurosurg 139:e406–e411
Charpentier C, Audibert G, Guillemin F, Civit T, Ducrocq X, Bracard S, Hepner H, Picard L, Laxenaire MC (1999) Multivariate analysis of predictors of cerebral vasospasm occurrence after aneurysmal subarachnoid hemorrhage. Stroke 30:1402–1408
D’Souza S (2015) Aneurysmal subarachnoid hemorrhage. J Neurosurg Anesthesiol 27:222–240
Dandapat S, Mendez-Ruiz A, Martinez-Galdamez M, Macho J, Derakhshani S, Foa Torres G, Pereira VM, Arat A, Wakhloo AK, Ortega-Gutierrez S (2021) Review of current intracranial aneurysm flow diversion technology and clinical use. J Neurointerv Surg 13:54–62
Dasenbrock H, Gormley WB, Lee Y, Mor V, Mitchell SL, Fehnel CR (2018) Long-term outcomes among octogenarians with aneurysmal subarachnoid hemorrhage. J Neurosurg 131:426–434
Golnari P, Nazari P, Garcia RM, Weiss H, Shaibani A, Hurley MC, Ansari SA, Potts MB, Jahromi BS (2020) Volumes, outcomes, and complications after surgical versus endovascular treatment of aneurysms in the United States (1993–2015): continued evolution versus steady-state after more than 2 decades of practice. J Neurosurg 134(3):848–861
Hajdu MA, Heistad DD, Siems JE, Baumbach GL (1990) Effects of aging on mechanics and composition of cerebral arterioles in rats. Circ Res 66:1747–1754
Hegedus K, Molnar P (1989) Age-related changes in reticulin fibers and other connective tissue elements in the intima of the major intracranial arteries. Clin Neuropathol 8:92–97
Klassen AC, Sung JH, Stadlan EM (1968) Histological changes in cerebral arteries with increasing age. J Neuropathol Exp Neurol 27:607–623
le Roux AA, Wallace MC (2010) Outcome and cost of aneurysmal subarachnoid hemorrhage. Neurosurg Clin N Am 21:235–246
Lin HL, Soo KM, Chen CW, Lin YK, Lin TY, Kuo LC, Lee WC, Huang SL (2014) Incidence, national trend, and outcome of nontraumatic subarachnoid haemorrhage in Taiwan: initial lower mortality, poor long-term outcome. Biomed Res Int 2014:274572
Magge SN, Chen HI, Ramakrishna R, Cen L, Chen Z, Elliott JP, Winn HR, Le Roux PD (2010) Association of a younger age with an increased risk of angiographic and symptomatic vasospasms following subarachnoid hemorrhage. J Neurosurg 112:1208–1215
McDougall CG, Spetzler RF, Zabramski JM, Partovi S, Hills NK, Nakaji P, Albuquerque FC (2012) The Barrow Ruptured Aneurysm Trial. J Neurosurg 116:135–144
Ohkuma H, Shimamura N, Naraoka M, Katagai T (2017) Aneurysmal subarachnoid hemorrhage in the elderly over age 75: a systematic review. Neurol Med Chir (Tokyo) 57:575–583
Pierot L, Szikora I, Barreau X, Holtmannspoetter M, Spelle L, Herbreteau D, Fiehler J, Costalat V, Klisch J, Januel AC, Weber W, Liebig T, Stockx L, Berkefeld J, Moret J, Molyneux A, Byrne J (2021) Aneurysm treatment with WEB in the cumulative population of two prospective, multicenter series: 3-year follow-up. J Neurointerv Surg 13:363–368
Rabb CH, Tang G, Chin LS, Giannotta SL (1994) A statistical analysis of factors related to symptomatic cerebral vasospasm. Acta Neurochir (Wien) 127:27–31
Rose MJ (2011) Aneurysmal subarachnoid hemorrhage: an update on the medical complications and treatments strategies seen in these patients. Curr Opin Anaesthesiol 24:500–507
Topple A, Fifkova E, Cullen-Dockstader K (1990) Effect of age on blood vessels and neurovascular appositions in the rat dentate fascia. Neurobiol Aging 11:371–380
Torbey MT, Hauser TK, Bhardwaj A, Williams MA, Ulatowski JA, Mirski MA, Razumovsky AY (2001) Effect of age on cerebral blood flow velocity and incidence of vasospasm after aneurysmal subarachnoid hemorrhage. Stroke 32:2005–2011
Wang AS, Campos JK, Colby GP, Coon AL, Lin LM (2020) Cerebral aneurysm treatment trends in National Inpatient Sample 2007–2016: endovascular therapies favored over surgery. J Neurointerv Surg 12:957–963
Acknowledgements
We thank the staff of Neuroscience Publications at Barrow Neurological Institute for assistance with manuscript preparation.
Author information
Authors and Affiliations
Contributions
Joshua S. Catapano, MD—manuscript writing; Kavelin Rumalla, MD—stats; Visish M. Srinivasan, MD—edits; Mohamed A. Labib, MD, CM—edits; Candice L. Nguyen, BS—data collection; Jacob F. Baranoski, MD—edits; Tyler S. Cole, MD—stats; Caleb Rutledge, MD—edits; Redi Rahmani, MD—edits; Joseph M. Zabramski, MD—final edits; Ashutosh P. Jadhav, MD—final edits; Andrew F. Ducruet, MD—final edits; Felipe C. Albuquerque, MD—final edits; and Michael T. Lawton, MD—final edits and approval.
Corresponding author
Ethics declarations
Ethics approval
The St. Joseph’s Hospital and Medical Center Institutional Review Board approved this observational study.
Informed consent
The need for informed consent was waived by the institutional review board due to the retrospective nature of the study and the minimal risk of patient identification.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Comments
The authors present a retrospective analysis of octo- and nonagenarians presenting with aneurysmal subarachnoid hemorrhage treated at the Barrow Neurological Institute from 2003 to 2019. A total of 1418 patients presented with aneurysmal subarachnoid hemorrhage during the study period, with 43 patients ≥ 80 years old. Logistic regression analysis demonstrated that increasing age was significantly associated with declining functional independence as measured by modified Rankin scores (mRS) at last follow-up. Increased age likely acts as a surrogate for the presence of comorbidities, worse baseline mRS, and diminished capacity for recovery after subarachnoid hemorrhage.
In addition, patients in the elderly age group were significantly more likely to undergo endovascular treatment, had lower rates of angiographic vasospasm, and similar rates of delayed cerebral ischemia as compared to younger patients. 91% of the elderly patients were not functionally independent, compared to 36% of the non-elderly patients at their final follow-up. It is unclear why elderly patients, other than their age, were more likely to undergo endovascular treatment since there were no significant differences in comorbidities, Hunt and Hess (HH) grades, and Fisher grades between elderly patients receiving endovascular or microsurgical treatments. The mRS scores and long-term mortality were not significantly different between the treatment types in elderly patients. The inclusion of patients from 2003 to 2007 that were enrolled in the Barrow Ruptured Aneurysm Trial (BRAT) in this current study may not fully reflect practice patterns based on clinical and patient factors since patients as a part of BRAT were randomized to microsurgical or endovascular treatments. It is unclear how much that may have altered the overall proportions of the respective treatment groups in this study.
Only 4 patients in the elderly cohort (9%) demonstrated functional independence at their final follow-up. Interestingly, these 4 patients all were treated endovascularly, had no significant comorbidities, no symptomatic vasospasm, no hydrocephalus, and had lower mean HH and Fisher grades compared to those with worse outcomes. As acknowledged by the authors, the small sample size of elderly patients with positive functional outcomes prevents statistical analysis in order to adequately evaluate variables that may result in functional recovery. These findings suggest that the presence of comorbidities, HH and Fisher grades remain important prognostic factors in elderly patients.
In this study, an overwhelming number of patients ≥ 80 years old with aneurysmal subarachnoid hemorrhage were unable to achieve functional independence regardless of treatment modality. This is a difficult group to study due to their small population, but future studies in conjunction with this data will help provide a valuable framework for discussions with families and patients regarding the prognosis of elderly patients with aneurysmal subarachnoid hemorrhage.
Eric T. Quach,
Christopher M. Loftus
Philadelphia, Pennsylvania, USA
This article is part of the Topical Collection on Vascular Neurosurgery—Aneurysm
Rights and permissions
About this article
Cite this article
Catapano, J.S., Rumalla, K., Srinivasan, V.M. et al. Treatment of octogenarians and nonagenarians with aneurysmal subarachnoid hemorrhage: a 17-year institutional analysis. Acta Neurochir 163, 2941–2946 (2021). https://doi.org/10.1007/s00701-021-04985-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-021-04985-y