Abstract
Background
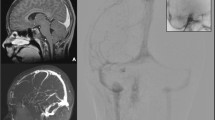
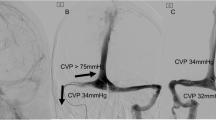
Acute occlusion of the posterior sagittal sinus may lead to dramatic increase in intracranial pressure (ICP), refractory to standard treatment. Hybrid vascular bypass of cranial venous outflow into the internal jugular vein (IJV) has seldom been described for this in recent neurosurgical literature.
Objective
To describe creation of a novel vascular bypass shunt from the superior sagittal sinus (SSS) to internal jugular vein (IJV) utilizing a covered stent-Dacron graft construct for control of refractory ICP.
Methods
We illustrate a patient with refractory ICP increases after acute sinus ligation that was performed to halt torrential bleeding from intraoperative injury. A temporary shunt was created that successfully controlled ICP. From the promising results of the temporary shunt, we utilized a prosthetic hybrid bypass graft to function as a shunt from the sagittal sinus to IJV. Yet the associated anticoagulation led to complications and a poor outcome.
Results
Rapid and sustained ICP reduction can be expected after sagittal sinus-to-jugular bypass shunt placement in acute sinus occlusion. Details of the surgical technique are described. Heparin anticoagulation, while imperative, is also associated with worrisome complications.
Conclusion
Acute occlusion of posterior third of sagittal sinus carries a very malignant clinical course. Intractable intracranial hypertension from acute sinus occlusion may be effectively treated with a SSS-IJV bypass shunt. A covered stent construct provides an effective vascular bypass conduit. However, the anticoagulation risk can lead to fatal outcomes. The neurosurgeon must always strive for primary repair of an injured sinus.








Similar content being viewed by others
References
Anaya-Ayala JE, Smolock CJ, Colvard BD et al (2011) Efficacy of covered stent placement for central venous occlusive disease in hemodialysis patients. J Vasc Surg 54(3):754–759
Bekken JA, Jongsma H, Fioole B (2018) The use of covered stents in aortoiliac obstructions: a systematic review and meta-analysis. J Cardiovasc Surg 59(1):14–25
Bonnal J, Brotchi J (1978) Surgery of the superior sagittal sinus in parasagittal meningiomas. J Neurosurg 48(6):935–945
Choi HC, Park SE, Choi DS et al (2018) Ruptured extracranial carotid artery: endovascular treatment with covered stent graft. J Neuroradiol 45(4):217–223
Colli BO, Carlotti CG Jr, Assirati JA Jr, Dos Santos MB, Neder L, Dos Santos AC (2006) Parasagittal meningiomas: follow-up review. Surg Neurol 66(3):S20–S28
Cooper KJ, Chick JF, Khaja MS et al (2018) Total endovascular iliocaval reconstruction using polytetrafluoroethylene stent-graft placement for the treatment of inferior vena cava resection. Cardiovasc Intervent Radiol 41(7):1116–1120
DiMeco F, Li KW, Casali C et al (2004) Meningiomas invading the superior sagittal sinus: surgical experience in 108 cases. Neurosurgery 55(6):1263–1274
Hajibandeh S, Hajibandeh S, Antoniou SA, Torella F, Antoniou GA (2016) Covered vs uncovered stents for aortoiliac and femoropopliteal arterial disease: a systematic review and meta-analysis. J Endovasc Ther 23(3):442–452
Hitchcock ER, Cowie RA (1981) Sino-jugular venous graft in otitic hydrocephalus. Acta Neurochir 59(3–4):187–193
Inaba K, Aksoy H, Seamon MJ et al (2016) Multicenter evaluation of temporary intravascular shunt use in vascular trauma. J Trauma Acute Care Surg 80(3):359–365
Meier U, Gärtner F, Knopf W, Klötzer R, Wolf O (1992) The traumatic dural sinus injury—a clinical study. Acta Neurochir (Wien) 119(1–4):91–93
Oh GS, Arnone GD, Abou-Al-Shaar H, Barks AL, Wong A, Charbel FT (2017) Surgical repair of iatrogenic transverse-sigmoid sinus laceration with a dural flap during skull base tumor surgery: a technical case report. World neurosurgery 106:1050-e7
Sindou M, Alvernia JE (2006) Results of attempted radical tumor removal and venous repair in 100 consecutive meningiomas involving the major dural sinuses. J Neurosurg 105(4):514–25
Sindou M, Mercier P, Bokor J, Brunon J (1980) Bilateral thrombosis of the transverse sinuses: microsurgical revascularization with venous bypass. Surg Neurol 13(3):215–220
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Medical University of South Carolina) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
Dr. Wooster was provided financial support in the form of an educational honorarium and is on the Speakers Bureau for Gore Medical (W.L. Gore & associates, Flagstaff, AZ). The sponsor had no role in the design or conduct of this research. All other authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Vascular Neurosurgery - Other
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sattur, M.G., Genovese, E.A., Weber, A. et al. Superior sagittal sinus-to-internal jugular vein bypass shunt with covered stent construct for intractable intracranial hypertension resulting from iatrogenic supratorcular sinus occlusion: technical note. Acta Neurochir 163, 2351–2357 (2021). https://doi.org/10.1007/s00701-021-04866-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-021-04866-4