Abstract
Background
Temporary transition from the half-seated position (HSP) to the lying position (LyP) is often associated with an increase in intracranial pressure (ICP) during management of patients with severe traumatic brain injury (TBI). This study was designed to assess the impact of the temporary LyP on cerebral perfusion and oxygenation in cases of severe TBI.
Method
Patients with a severe blunt TBI with indication of ICP monitoring were prospectively included. Patients underwent standardized management according to the international guidelines to minimize secondary insults. For each patient, a maneuver to a LyP for 30 min was performed daily during the first 7 days of hospitalization. ICP, cerebral perfusion pressure (CPP), mean velocity (Vm), pulsatility index (PI), regional cerebral oxygen saturation (rScO2), jugular venous oxygen saturation (SvjO2)) were compared in the HSP and the LyP.
Results
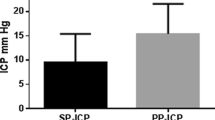
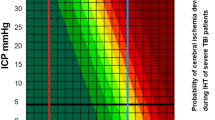
Twenty-four 24 patients were included. The median Glasgow coma scale score was 6 (interquartile range (IQR), 3–8), the median injury severity score was 32 (IQR, 25–48), and the mean age was 39 ± 16 years. On day 1, ICP (+ 6 mmHg (IQR, 4–7 mmHg)) and CPP (+ 10 mmHg (IQR, 5–14 mmHg) were significantly increased in the LyP compared with the HSP. Vm increased significantly in the LyP on the mainly injured side (+ 6 cm/s (IQR, + 0–11 cm/s); P = 0.01) and on the less injured side (+ 4 cm/s (IQR, + 1–8 cm/s); P < 0.01). rScO2 behaved similarly (+ 2 points (IQR, + 2–4 points) and + 3 points (IQR, + 2–5 points), respectively; P < 0.001). Mixed models highlighted the significant association between the position and CPP, Vm, rScO2, with more favorable conditions in the lying position.
Conclusions
Within the first week of management, the temporary LyP in cases of severe TBI was associated with a moderate increase in CPP, Vm, and rScO2despite a moderate increase in ICP.



Similar content being viewed by others
Change history
16 February 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00701-023-05528-3
References
Alperin N, Lee SH, Sivaramakrishnan A, Hushek SG (2005) Quantifying the effect of posture on intracranial physiology in humans by MRI flow studies. J Magn Reson Imaging 22(5):591–596
Bouma GJ, Muizelaar JP (1990) Relationship between cardiac output and cerebral blood flow in patients with intact and with impaired autoregulation. J Neurosurg 73(3):368–374
Bouma GJ, Muizelaar JP, Bandoh K, Marmarou A (1992) Blood pressure and intracranial pressure-volume dynamics in severe head injury: relationship with cerebral blood flow. J Neurosurg 77(1):15–19
Boyd CR, Tolson MA, Copes WS (1987) Evaluating trauma care: the TRISS method. Trauma Score and the Injury Severity Score. J Trauma 27(4):370–8.
Butler GC, Xing HC, Hughson RL (1990) Cardiovascular response to 4 hours of 6 degrees head-down tilt or of 30 degrees head-up tilt bed rest. Aviat Space Environ Med 61(3):240–246
Carney N, Totten AM, O’Reilly C, et al (2017) Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurg 80(1):6–15
Consonni F, Abate MG, Galli D, Citerio G (2009) Feasibility of a continuous computerized monitoring of cerebral autoregulation in neurointensive care. Neurocrit Care 10(2):232–240
Czosnyka M, Smielewski P, Kirkpatrick P, Menon DK, Pickard JD (1996) Monitoring of cerebral autoregulation in head-injured patients. Stroke 27(10):1829–1834
Czosnyka M, Smielewski P, Kirkpatrick P, Laing RJ, Menon D, Pickard JD (1997) Continuous assessment of the cerebral vasomotor reactivity in head injury. Neurosurg 41(1):11–17; discussion 17–19.
De Deyne C, Vandekerckhove T, Decruyenaere J, Colardyn F (1996) Analysis of abnormal jugular bulb oxygen saturation data in patients with severe head injury. Acta Neurochir (Wien) 138(12):1409–1415
Durward QJ, Amacher AL, Del Maestro RF, Sibbald WJ (1983) Cerebral and cardiovascular responses to changes in head elevation in patients with intracranial hypertension. J Neurosurg 59(6):938–944
Fan J-Y (2004) Effect of backrest position on intracranial pressure and cerebral perfusion pressure in individuals with brain injury: a systematic review. J Neurosci Nurs 36(5):278–288
Feldman Z, Kanter MJ, Robertson CS et al (1992) Effect of head elevation on intracranial pressure, cerebral perfusion pressure, and cerebral blood flow in head-injured patients. J Neurosurg 76(2):207–211
Greenspan L, McLellan BA, Greig H (1985) Abbreviated Injury Scale and Injury Severity Score: a scoring chart. J Trauma 25(1):60–64
Hlatky R, Furuya Y, Valadka AB et al (2002) Dynamic autoregulatory response after severe head injury. J Neurosurg 97(5):1054–1061
Howells T, Elf K, Jones PA et al (2005) Pressure reactivity as a guide in the treatment of cerebral perfusion pressure in patients with brain trauma. J Neurosurg 102(2):311–317
Jennett B, Bond M (1975) Assessment of outcome after severe brain damage. Lancet 1(7905):480–484
Jourdan C, Bayen E, Pradat-Diehl P, et al (2016) A comprehensive picture of 4-year outcome of severe brain injuries. Results from the PariS-TBI study. Ann Phys Rehabil Med 59(2):100–6
Kenning JA, Toutant SM, Saunders RL (1981) Upright patient positioning in the management of intracranial hypertension. Surg Neurol 15(2):148–152
Kosty JA, Leroux PD, Levine J et al (2013) Brief report: a comparison of clinical and research practices in measuring cerebral perfusion pressure: a literature review and practitioner survey. Anesth Analg 117(3):694–698
Lassen NA (1959) Cerebral blood flow and oxygen consumption in man. Physiol Rev 39(2):183–238
Ledwith MB, Bloom S, Maloney-Wilensky E, Coyle B, Polomano RC, Le Roux PD (2010) Effect of body position on cerebral oxygenation and physiologic parameters in patients with acute neurological conditions. J Neurosci Nurs 42(5):280–287
Meixensberger J, Baunach S, Amschler J, Dings J, Roosen K (1997) Influence of body position on tissue-pO2, cerebral perfusion pressure and intracranial pressure in patients with acute brain injury. Neurol Res 19(3):249–253
Miyamoto Y, Tamura T, Hiura T, Nakamura T, Higuchi J, Mikami T (1982) The dynamic response of the cardiopulmonary parameters to passive head-up tilt. Jpn J Physiol 32(2):245–258
Murkin JM, Arango M (2009) Near-infrared spectroscopy as an index of brain and tissue oxygenation. Br J Anaesth 103 Suppl 1:i3–13
Norager NH, Olsen MH, Riedel CS, Juhler M (2020) Changes in intracranial pressure and pulse wave amplitude during postural shifts
Olavarría VV, Arima H, Anderson CS et al (2014) Head position and cerebral blood flow velocity in acute ischemic stroke: a systematic review and meta-analysis. Cerebrovasc Dis 37(6):401–408
Peeters W, van den Brande R, Polinder S et al (2015) Epidemiology of traumatic brain injury in Europe. Acta Neurochir (Wien) 157(10):1683–1696
Rao V, Klepstad P, Losvik OK, Solheim O (2013) Confusion with cerebral perfusion pressure in a literature review of current guidelines and survey of clinical practice. Scand J Trauma Resusc Emerg Med 21:78
Reinstrup P, Unnerbäck M, Marklund N, Schalen W, Arrocha JC, Bloomfield EL, Sadegh V, Hesselgard K (2019) Best zero level for external ICP transducer. Acta Neurochir (Wien) 161(4):635–642
Robertson C (1993) Desaturation episodes after severe head injury: influence on outcome. Acta Neurochir Suppl (Wien) 59:98–101
Roozenbeek B, Maas AIR, Menon DK (2013) Changing patterns in the epidemiology of traumatic brain injury. Nat Rev Neurol 9(4):231–236
Rosner MJ, Coley IB (1986) Cerebral perfusion pressure, intracranial pressure, and head elevation. J Neurosurg 65(5):636–641
Schwarz S, Georgiadis D, Aschoff A, Schwab S (2002) Effects of body position on intracranial pressure and cerebral perfusion in patients with large hemispheric stroke. Stroke 33(2):497–501
Sorrentino E, Diedler J, Kasprowicz M et al (2012) Critical thresholds for cerebrovascular reactivity after traumatic brain injury. Neurocrit Care 16(2):258–266
Sviri GE, Aaslid R, Douville CM, Moore A, Newell DW (2009) Time course for autoregulation recovery following severe traumatic brain injury. J Neurosurg 111(4):695–700
Winkelman C (2000) Effect of backrest position on intracranial and cerebral perfusion pressures in traumatically brain-injured adults. Am J Crit Care 9(6):373–380
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the French institutional research committee (ID RCB 2014-A00708-39), the French data protection authority (CNIL) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Trial registration
ClinicalTrials.gov Identifier: NCT02832908
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Brain trauma
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dagod, G., Roustan, JP., Bringuier-Branchereau, S. et al. Effect of a temporary lying position on cerebral hemodynamic and cerebral oxygenation parameters in patients with severe brain trauma. Acta Neurochir 163, 2595–2602 (2021). https://doi.org/10.1007/s00701-021-04851-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-021-04851-x