Abstract
Background
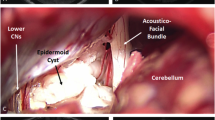
Although many reports state that only the lateral suboccipital retrosigmoid approach (LSO) should be used for removal of cerebellopontine angle (CPA) epidermoid cysts, it is preferable to use various surgical approaches as appropriate for each patient, for radical resection with an optimal operative field under direct visualization, and for the preservation of cranial nerve (CN) functions. In the present study, we hence focused on the importance of surgical approach selection for removal of CPA epidermoid cysts and analyzed the results of CPA epidermoid cysts after surgery in our series.
Methods
Fifty-four patients who underwent surgery for CPA epidermoid cysts were retrospectively analyzed, regarding their surgical approaches, removal rates, preservation rates of CN function 1 year after surgery, and recurrence. Surgical approaches were selected for patients according to the size and extension of the tumor.
Results
Surgical approaches consisted of LSO (20 cases), anterior transpetrosal approach (ATP; 3 cases), combined transpetrosal approach (27 cases), and ATP + LSO (4 cases). Mean tumor content removal and capsule removal rates were 97.4% and 78.3%, respectively. Preservation rates of facial nerve function and useful hearing were 94.4% and 90.7%, respectively. The mean postoperative follow-up time was 62.8 months, and there were two cases of recurrence requiring reoperation about 10 years after surgery.
Conclusions
For CPA epidermoid cyst surgeries, selection of the appropriate surgical approach for each patient and radical resection with an optimal operative field under direct visualization enable tumor removal without the need for reoperation for a long time, with preservation of CN functions.





Similar content being viewed by others
Abbreviations
- AAO-HNS:
-
American Academy of Otolaryngology–Head and Neck Surgery
- ABR:
-
Auditory brainstem response
- ATP:
-
Anterior transpetrosal approach
- CN:
-
Cranial nerve
- CPA:
-
Cerebellopontine angle
- CTP:
-
Combined transpetrosal approach
- GTR:
-
Gross total removal
- H-B:
-
House–Brackmann
- LSO:
-
Lateral suboccipital retrosigmoid approach
- SS:
-
Sigmoid sinus
- ST:
-
Subtemporal approach
- STR:
-
Subtotal removal
References
Aboud E, Abolfotoh M, Pravdenkova S, Gokoglu A, Gokden M, Al-Mefty O (2015) Giant intracranial epidermoids: is total removal feasible? J Neurosurg 122:743–756
Akar Z, Tanriover N, Tuzgen S, Kafadar AM, Kuday C (2003) Surgical treatment of intracranial epidermoid tumors. Neurol Med Chir (Tokyo) 43(6):275–281
Altschuler E, Jungreis C, Sekhar LN, Jannetta P, Sheptak P (1990) Operative treatment of intracranial epidermoid cysts and cholesterol granulomas: report of 21 cases. Neurosurg 26(4):606–614
Alvord ECJ (1977) Growth rates of epidermoid tumors. Ann Neurol 2(5):367–370
Baumann CH, Bucy PC (1956) Paratrigeminal epidermoid tumors. J Neurosurg 13:455–468
Berger MS, Wilson CB (1985) Epidermoid cysts of the posterior fossa. J Neurosurg 62(2):214–219
Chandler WF, Farhat SM, Pauli FJ (1975) Intrathalamic epidermoid tumor. J Neurosurg 43(5):614–617
Chowdhury F, Haque M, Sarker M (2013) Intracranial epidermoid tumor; microneurosurgical management: an experience of 23 cases. Surg 8(1):21–28
Czernicki T, Kunert P, Nowak A, Wojciechowski J, Marchel A (2016) Epidermoid cysts of the cerebellopontine angle: clinical features and treatment outcomes. Neurol Neurochir Pol 50(2):75–82
Darrouzet V, Franco-Vidal V, Hilton M, Nguyen DQ, Lacher-Fougere S, Guerin J, Bebear JP (2004) Surgery of cerebellopontine angle epidermoid cysts: role of the widened retrolabyrinthine approach combined with endoscopy. Otolaryngol Head Neck Surg 131(1):120–125
DeSouza CE, DeSouza R, Da Costa S, Sperling N, Yoon TH, Abdelhamid MM, Sharma RR, Goel A (1989) Cerebellopontine angle epidermoid cysts: a report on 30 cases. J Neurol Neurosurg Psychiatry 52(8):986–990
Farhoud A, Khedr W, Aboul-Enein H (2018) Surgical resection of cerebellopontine epidermoid cysts: limitations and outcome. J Neurol Surg Part B Skull Base 79(2):167–172
Goel A, Muzumdar D, Desai K (2006) Anterior tentorium-based epidermoid tumours: results of radical surgical treatment in 96 cases. Br J Neurosurg 20(3):139–145
Gopalakrishnan CV, Ansari KA, Nair S, Menon G (2014) Long term outcome in surgically treated posterior fossa epidermoids. Clin Neurol Neurosurg 117:93–99
Grahnke K, Burkett D, Li D, Szujewski C, Leonetti JP, Anderson DE (2018) Cranial nerve preservation following surgical treatment for epidermoid cysts of the posterior and middle fossae. J Neurol Surg Part B Skull Base 79(5):445–450
Guidetti B, Gagliardi FM (1977) Epidermoid and dermoid cysts. Clinical evaluation and late surgical results. J Neurosurg 47(1):12–18
Guo Z, Ouyang H, Cheng Z (2011) Surgical treatment of parapontine epidermoid cysts presenting with trigeminal neuralgia. J Clin Neurosci 18(3):344–346
Hasegawa M, Inamasu J, Yoshida K, Nagahisa S, Nouri M, Adachi K, Hirose Y, Fujisawa H (2016) Cerebellopontine angle epidermoid cysts: clinical presentations and surgical outcome. Neurosurg Rev 39(2):259–267
Hu Z, Guan F, Kang T, Huang H, Dai B, Zhu G, Mao B, Kang Z (2016) Whole course neuroendoscopic resection of cerebellopontine angle epidermoid cysts. J Neurol Surg Part A Cent Eur Neurosurg 77:381–388
Kato K, Ujiie H, Higa T, Hayashi M, Kubo O, Okada Y, Hori T (2010) Clinical presentation of intracranial epidermoids: a surgical series of 20 initial and four recurred cases. Surg 5(1):32–40
Kobata H, Kondo A, Iwasaki K (2002) Cerebellopontine angle epidermoids presenting with cranial nerve hyperactive dysfunction: pathogenesis and long-term surgical results in 30 patients. Neurosurg 50(2):276–286
Lunardi P, Missori P, Innocenzi G, Gagliardi FM, Fortuna A (1990) Long-term results of surgical treatment of cerebello-pontine angle epidermoids. Acta Neurochir 103:105–108
Lynch JC, Aversa A, Pereira C, Nogueira J, Gonçalves M, Lopes H (2014) Surgical strategy for intracranial dermoid and epidermoid tumors: an experience with 33 patients. Surg Neurol Int. https://doi.org/10.4103/2152-7806.145764
Mallucci CL, Ward V, Carney AS, O’Donoghue GM, Robertson I (1999) Clinical features and outcomes in patients with non-acoustic cerebellopontine angle tumours. J Neurol Neurosurg Psychiatry 66(6):768–771
Matsushima K, Kohno M, Nakajima N, Ichimasu N (2019) Combined transpetrosal approach with preservation of superior petrosal vein drainage for a cerebellopontine angle epidermoid cyst extending into Meckel’s Cave: 3-dimensional operative video. Oper Neurosurg 16(6):E172–E173
Meng L, Yuguang L, Feng L, Wandong S, Shugan Z, Chengyuan W (2005) Cerebellopontine angle epidermoids presenting with trigeminal neuralgia. J Clin Neurosci 12(7):784–786
Mohanty A, Venkatrama SK, Rao BR, Chandramouli BA, Jayakumar PN, Das BS (1997) Experience with cerebellopontine angle epidermoids. Neurosurg 40(1):24–30
Nagasawa D, Yew A, Safaee M, Fong B, Gopen Q, Parsa AT, Yang I (2011) Clinical characteristics and diagnostic imaging of epidermoid tumors. J Clin Neurosci 18(9):1158–1162
Obrador S, Lopez-Zafra JJ (1969) Clinical features of the epidermoids of the basal cisterns of the brain. J Neurol Neurosurg Psychiatry 32(5):450–454
Peng Y, Yu L, Li Y, Fan J, Qiu M, Qi S (2014) Pure endoscopic removal of epidermoid tumors of the cerebellopontine angle. Childs Nerv Syst 30(7):1261–1267
Rubin G, Scienza R, Pasqualin A, Rosta L, Da Pian R (1989) Craniocerebral epidermoids and dermoids. Acta Neurochir 97:1–16
Sabin HI, Bordi LT, Symon L (1987) Epidermoid cysts and cholesterol granulomas centered on the posterior fossa: twenty years of diagnosis and management. Neurosurg 21(6):798–805
Safavi-Abbasi S, Di Rocco F, Bambakidis N, Talley MC, Gharabaghi A, Luedemann W, Samii M, Samii A (2008) Has management of epidermoid tumors of the cerebellopontine angel improved? A surgical synopsis of the past and present. Skull Base 18(2):85–98
Samii M, Tatagiba M, Piquer J, Carvalho GA (1996) Surgical treatment of epidermoid cysts of the cerebellopontine angle. J Neurosurg 84(1):14–19
Schiefer TK, Link MJ (2008) Epidermoids of the cerebellopontine angle: a 20-year experience. Surg Neurol 70(6):584–590
Schroeder HWS, Oertel J, Gaab MR (2004) Endoscope-assisted microsurgical resection of epidermoid tumors of the cerebellopontine angle. J Neurosurg 101(2):227–232
Shear BM, Jin L, Zhang Y, David WB, Fomchenko EI, Erson-Omay EZ, Huttner A, Fulbright RK, Moliterno J (2019) Extent of resection of epidermoid tumors and risk of recurrence: case report and meta-analysis. J Neurosurg 1–11. https://doi.org/10.3171/2019.4.JNS19598
Singh I, Rohilla S, Kumar P, Krishana D (2018) Combined microsurgical and endoscopic technique for removal of extensive intracranial epidermoids. Surg Neurol Int. https://doi.org/10.4103/sni.sni
Talacchi A, Sala F, Alessandrini F, Turazzi S, Bricolo A (1998) Assessment and surgical management of posterior fossa epidermoid tumors: Report of 28 cases. Neurosurg 42(2):242–252
Tancredi A, Fiume D, Gazzeri G, Knosp E, Isamat F (2003) Epidermoid cysts of the fourth ventricle: very long follow up in 9 cases and review of the literature. Acta Neurochir 145(10):905–911
Tuchman A, Platt A, Winer J, Pham M, Giannotta S, Zada G (2014) Endoscopic-assisted resection of intracranial epidermoid tumors. World Neurosurg 82(3):450–454
Vinchon M, Pertuzon B, Lejeune J-P, Assaker R, Pruvo J-P, Christiaens J-L (1995) Intradural epidermoid cysts of the cerebellopontine angle: diagnosis and surgery. Neurosurg 36(1):52–57
Yamakawa K, Shitara N, Genka S, Manaka S, Takakura K (1989) Clinical course and surgical prognosis of 33 cases of intracranial epidermoid tumors. Neurosurg 24(4):568–573
Yasargil M, Abernathey C, Sarioglu A (1989) Microneurosurgical treatment of intracranial dermoid and epidermoid tumors. Neurosurg 24(4):561–567
Yawn RJ, Patel NS, Driscoll CL, Link MJ, Haynes DS, Wanna GB, Thompson RC, Carlson ML (2016) Primary epidermoid tumors of the cerebellopontine angle: a review of 47 cases. Otol Neurotol 37:951–955
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Contributions
The authors are indebted to Helena Akiko Popiel, Department of International Medical Communications of Tokyo Medical University, for her review of the English manuscript. Also, we thank Mrs. Asa Otonari for her assistance in preparing this manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Tokyo Medical University and Tokyo Metropolitan Police Hospital) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Conflict of interest
The authors declare that they have no conflict of interest and no personal or institutional financial interest regarding any of the drugs, materials, or devices described in this article.
Additional information
Comments:
In this series of 54 epidermoid cysts of the cerebellopontine area (CPA) and surrounding compartments, the authors achieved good results tailoring the surgical approaches into retrosigmoid, anterior petrosal and transpetrosal approaches to remove the CPA epidermoid cysts. In fact, epidermoid cysts do not respect the subarachnoidal compartments and may invade distant areas. The classical retrosigmoid approach may be insufficient to address to all these compartments in giant epidermoid cysts due to limited angle of view provided by this approach. In order to achieve maximal resection of the lesion and protect the cranial nerves one must sometimes include additional approaches such as those described in this paper. However, transpetrosal approaches are more demanding and involve higher risks of CSF leak and hearing loss. These disadvantaged must be taken into consideration when choosing the approaches. The additional use of endoscopes with different angulations (30°, 45°, 70°) may incredibly enhance the possibilities of the retrosigmoid approach, so that far lesions located "around the corner" can be addressed as well. Finding a good balance between radically removing the beging cyst while increasing potential risks to cranial nerves and vessels, or risking recurrence that might be very difficult to treat with use of less invasive approaches, is the real challenge in these cases and demands large experience in dealing with these lesions.
Marcos Tatagiba
Tübingen, Germany
Comment
There are several issues of discussion in the surgical treatment of epidermoid cysts in the cerebellopontine angle, including surgical indication, selection of appropriate approach, decision-making of how radically the capsule should be removed considering function preservation before and during the surgery, evaluation of residual capsule during and after the operation, analysis of long-term follow-up results relating to the surgical radicality and growth rate of recurrence, and timing of reoperation for recurrent tumor, etc. In this paper, the authors intended to perform radical capsule resection via a wide exposure by selecting approaches like suboccipital approach, anterior transpetrosal approach and combined transpetrosal approach, which was tailored to the individual case. The retrospective review in 54 patients showed excellent surgical outcomes as compared to those in the literature. Nevertheless, there still exists the same issues of discussion as described above. In the surgery of epidermoid cysts, unlike meningiomas, coagulation of feeding arteries at the deeper part of the petro-clival area is not required, and there is a risk of complication due to the overexposure of the skull base. Careful consideration should be given when using an invasive transpetrosal approach for a highly benign disease like this. Further studies are needed on the combined use of suboccipital and endoscopic surgery. Surgery for epidermoid cysts, which requires long-term follow-up after surgery, often needs further resolution.
Kenji Ohata
Osaka, Japan
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Tumor
Rights and permissions
About this article
Cite this article
Sakamoto, H., Kohno, M., Matsushima, K. et al. Importance of appropriate surgical approach selection for radical resection of cerebellopontine angle epidermoid cysts with preservation of cranial nerve functions: our experience of 54 cases . Acta Neurochir 163, 2465–2474 (2021). https://doi.org/10.1007/s00701-021-04840-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-021-04840-0