Abstract
Background
In idiopathic normal pressure hydrocephalus (iNPH), gait and balance impairment is the most frequent symptom, and it is often associated with a higher fall risk. In a prior study, the anterior callosal angle (ACA) was validated as a reliable marker to discriminate iNPH from Alzheimer’s disease and healthy controls. However, the potential correlation between the ACA with clinical symptoms and functional outcomes has not been assessed. The objective of this study is to determine the utility of the ACA in predicting gait improvement after ventriculoperitoneal (VP) shunting.
Methods
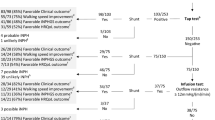
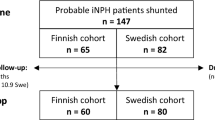
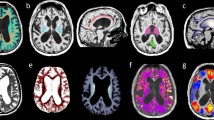
Patients with probable iNPH who underwent shunt placement at a single institution were prospectively enrolled from May 2015 to May 2019. Patients were assessed preoperatively and at 6 months postoperatively following a standard clinical and MRI protocol. Callosal angle (CA) and ACA were calculated from 3 T MRI preoperatively and at 6 months postoperatively. CA and ACA were tested for correlation with clinical scores.
Results
Forty-seven patients with probable INPH who completed 6-month postoperative follow-up were enrolled in the study. Baseline ACA was significantly correlated with preoperative fall risk, gait, and balance impairment assessed with Tinetti POMA scale. Additionally, baseline ACA differentiated patients who experienced improvement at Tinetti POMA scale after surgery.
Conclusions
The baseline ACA is a useful neuroradiological marker to differentiate patients by fall risk and has significant correlation with the improvement in gait and balance impairment following surgery. This study demonstrated that the ACA may be a complementary tool to the CA in predicting shunt responsiveness in iNPH.


Similar content being viewed by others
References
Adams RD, Fisher CM, Hakim S, Ojemann RG, Sweet WH (1965) Symptomatic occult hydrocephalus with “normal” cerebrospinal-fluid pressure. A Treatable Syndrome. N Engl J Med 273:117–126
Agerskov S, Hellström P, Andrén K, Kollén L, Wikkelsö C, Tullberg M (2018) The phenotype of idiopathic normal pressure hydrocephalus-a single center study of 429 patients. J Neurol Sci 391:54–60
Aruga S, Kuwana N, Shiroki Y, Takahashi S, Samejima N, Watanabe A, Seki Y, Igawa Y, Homma Y (2018) Effect of cerebrospinal fluid shunt surgery on lower urinary tract dysfunction in idiopathic normal pressure hydrocephalus. Neurourol Urodyn 37(3):1053–1059
Bonita R, Beaglehole R (1998) Recovery of motor function after stroke. Stroke 19(12):1497–1500
Cagnin A, Simioni M, Tagliapietra M, Citton V, Pompanin S, Della Puppa A, Ermani M, Manara R (2015) A simplified callosal angle measure best differentiates idiopathic-normal pressure hydrocephalus from neurodegenerative Dementia. J Alzheimers Dis 46(4):1033–1038
Faber MJ, Bosscher RJ, van Wieringen PC (2006) Clinimetric properties of the performance-oriented mobility assessment. Phys Ther 86(7):944–954
Feick D, Sickmond J, Liu L, Metellus P, Williams M, Rigamonti D, Hill-Briggs F (2008) Sensitivity and predictive value of occupational and physical therapy assessments in the functional evaluation of patients with suspected normal pressure hydrocephalus. J Rehabil Med 40(9):715–720
Giannini G, Palandri G, Ferrari A, Oppi F, Milletti D, Albini-Riccioli L, Mantovani P, Magnoni S, Chiari L, Cortelli P, Cevoli S, BOLOGNA PRO-HYDRO Study Group (2019) A prospective evaluation of clinical and instrumental features before and after ventriculo-peritoneal shunt in patients with idiopathic normal pressure hydrocephalus: the Bologna PRO-Hydro study. Parkinsonism Relat Disord 66:117–124
Grahnke K, Jusue-Torres I, Szujewski C, Joyce C, Schneck M, Prabhu VC, Anderson DE (2018) The quest for predicting sustained shunt response in normal-pressure hydrocephalus: an analysis of the callosal angle’s utility. World Neurosurg 115:717–722
Ishii K, Kanda T, Harada A, Miyamoto N, Kawaguchi T, Shimada K, Ohkawa S, Uemura T, Yoshikawa T, Mori E (2008) Clinical impact of the callosal angle in the diagnosis of idiopathic normal pressure hydrocephalus. Eur Radiol 18(11):2678–2683
Isik AT, Kaya D, Ates Bulut E, Dokuzlar O, Soysal P (2019) The outcomes of serial cerebrospinal fluid removal in elderly patients with idiopathic normal pressure hydrocephalus. Clin Interv 14:2063–2069
Junkkari A, Sintonen H, Nerg O, Koivisto AM, Roine RP, Viinamäki H, Soininen H, Jääskeläinen JE, Leinonen V (2015) Health-related quality of life in patients with idiopathic normal pressure hydrocephalus. Eur J Neurol 22(10):1391–1399
Kockum K, Lilja-Lund O, Larsson EM, Rosell M, Söderström L, Virhammar J, Laurell K (2018) The idiopathic normal-pressure hydrocephalus Radscale: a radiological scale for structured evaluation. Eur J Neurol 25(3):569–576
Kubo Y, Kazui H, Yoshida T, Kito Y, Kimura N, Tokunaga H, Ogino A, Miyake H, Ishikawa M, Takeda M (2008) Validation of grading scale for evaluating symptoms of idiopathic normal-pressure hydrocephalus. Dement Geriatr Cogn Disord 25(1):37–45
Lewis C (1993) Balance, gait test proves simple but useful. P. T. Bulletin 8(6):9–40
Mantovani P, Albini-Riccioli L, Giannini G, Milletti D, Sorenson TJ, Stanzani-Maserati M, Oppi F, Elder BD, Cevoli S, Cortelli P, Palandri G, BOLOGNA PRO-HYDRO Study Group (2020) Anterior callosal angle: a new marker of idiopathic normal pressure hydrocephalus? World Neurosurg 139:e548–e552. https://doi.org/10.1016/j.wneu.2020.04.085
Mataró M, Poca MA, Salgado-Pineda P, Castell-Conesa J, Sahuquillo J, Díez-Castro MJ, Aguadé-Bruix S, Vendrell P, del Mar Matarín M, Junqué C (2003) Postsurgical cerebral perfusion changes in idiopathic normal pressure hydrocephalus: a statistical parametric mapping study of SPECT images. J Nucl Med 44(12):1884–1889
Miyoshi N, Kazui H, Ogino A, Ishikawa M, Miyake H, Tokunaga H, Ikejiri Y, Takeda M (2015) Association between cognitive impairment and gait disturbance in patients with idiopathic normal pressure hydrocephalus. Dement Geriatr Cogn Disord 20(2–3):71–76
Momjian S, Owler BK, Czosnyka Z, Czosnyka M, Pena A, Pickard JD (2004) Pattern of white matter regional cerebral blood flow and autoregulation in normal pressure hydrocephalus. Brain 127(5):965–972
Nikaido Y, Urakami H, Akisue T, Okada Y, Katsuta N, Kawami Y, Ikeji T, Kuroda K, Hinoshita T, Ohno H, Kajimoto Y, Saura R (2019) Associations among falls, gait variability, and balance function in idiopathic normal pressure hydrocephalus. Clin Neurol Neurosurg 83:1053–1085
Relkin N, Marmarou A, Klinge P, Bergsneider M, Black PM (2005) Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery 57(3):4–16
Sakakibara R, Uchida Y, Ishii K, Kazui H, Hashimoto M, Ishikawa M, Yuasa T, Kishi M, Ogawa E, Tateno F, Uchiyama T, Yamamoto T, Yamanishi T, Terada H, SINPHONI (2012) Correlation of right frontal hypoperfusion and urinary dysfunction in iNPH: a SPECT study. Neurourol Urodyn 31(1):50–55
Shore WS, deLateur BJ, Kuhlemeier KV, Imteyaz H, Rose G, Williams MA (2005) A comparison of gait assessment methods: Tinetti and GAITRite electronic walkway. J Am Geriatr Soc 53(11):2044–2045
Skalický P, Mládek A, Vlasák A, De Lacy P, Beneš V, Bradáč O (2019) Normal pressure hydrocephalus-an overview of pathophysiological mechanisms and diagnostic procedures. Neurosurg Rev. https://doi.org/10.1007/s10143-019-01201-5
Tinetti ME (1986) Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc 34(2):119–126
Virhammar J, Laurell K, Cesarini KG, Larsson EM (2014) The callosal angle measured on MRI as a predictor of outcome in idiopathic normal-pressure hydrocephalus. J Neurosurg 120(1):178–184
Virhammar J, Laurell K, Cesarini KG, Larsson EM (2014) Preoperative prognostic value of MRI findings in 108 patients with idiopathic normal pressure hydrocephalus. Am J Neuroradiol 35:2311–2318
Virhammar J, Laurell K, Cesarini KG, Larsson EM (2018) Increase in callosal angle and decrease in ventricular volume after shunt surgery in patients with idiopathic normal pressure hydrocephalus. J Neurosurg 130(1):130–135
Williams MA, Malm J (2016) Diagnosis and treatment of idiopathic normal pressure hydrocephalus. Continuum 22(2):579–599
Wu EM, El Ahmadieh TY, Kafka B, Caruso JP, Neeley OJ, Plitt AR, Aoun SG, Olson D, Ruchinskas RA, Cullum CM, Welch BG, Batjer HH, White JA (2019) Clinical outcomes of normal pressure hydrocephalus in 116 patients: objective versus subjective assessment. J Neurosurg 12:1–7
Zadikoff C, Lang AE (2005) Apraxia in movement disorders. Brain 128(7):1480–1497
Acknowledgments
PRO-HYDRO Study Group: Raffaele Agati1, Raffaele Aspide1, Giovanna Calandra-Buonaura1,2, Sabina Capellari1,2, Lorenzo Chiari3, Alberto Ferrari3, Elena Magelli1, Margherita Merola1, Federico Oppi1, Piero Parchi1,4, Alessandro Pirina1, Vito Antonio Piserchia1, Luisa Sambati1.
1IRCCS Istituto Scienze Neurologiche di Bologna, Bologna, Italia.
2DIBINEM, University of Bologna, Bologna, Italy.
3CIRI-SDV, University of Bologna, Bologna, Italy.
4DIMES, University of Bologna, Bologna, Italy.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurosurgery general
Rights and permissions
About this article
Cite this article
Mantovani, P., Giannini, G., Milletti, D. et al. Anterior callosal angle correlates with gait impairment and fall risk in iNPH patients. Acta Neurochir 163, 759–766 (2021). https://doi.org/10.1007/s00701-020-04699-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-020-04699-7