Abstract
Background
Idiopathic normal-pressure hydrocephalus (NPH) is a condition of the elderly treated by ventriculoperitoneal shunt (VP) insertion. A subset of NPH patients respond only temporarily to shunt insertion despite low valve opening pressure. This study aims to describe our experience of patients who benefit from further CSF drainage by adding adjustable antigravity valves and draining CSF at ultra-low pressure.
Methods
Single-centre retrospective case series of patients undergoing shunt valve revision from an adjustable differential pressure valve with fixed antigravity unit to a system incorporating an adjustable gravitational valve (Miethke proSA). Patients were screened from a database of NPH patients undergoing CSF diversion over 10 consecutive years (April 2008–April 2018). Clinical records were retrospectively reviewed for interventions and clinical outcomes.
Results
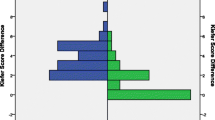
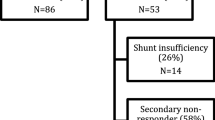
Nineteen (10F:9M) patients underwent elective VP shunt revision to a system incorporating an adjustable gravitational valve. Mean age 77.1 ± 7.1 years (mean ± SD). Eleven patients (58%) showed significant improvement in walking speed following shunt revision. Fourteen patients/carers (74%) reported subjective improvements in symptoms following shunt revision.
Conclusions
Patients presenting symptoms relapse following VP shunting may represent a group of patients with ultra-low-pressure hydrocephalus, for whom further CSF drainage may lead to an improvement in symptoms. These cases may benefit from shunt revision with an adjustable gravitational valve, adjustment of which can lead to controlled siphoning of CSF and drain CSF despite ultra-low CSF pressure.


Similar content being viewed by others
Abbreviations
- CSF:
-
Cerebrospinal fluid
- NPH:
-
Normal-pressure hydrocephalus
- VP:
-
Ventriculoperitoneal
References
Benveniste RJ, Sur S (2018) Delayed symptom progression after ventriculoperitoneal shunt placement for normal pressure hydrocephalus. J Neurol Sci 393:105–109
Chari A, Dasgupta D, Smedley A, Craven C, Dyson E, Matloob S, Thompson S, Thorne L, Toma AK, Watkins L (2017) Intraparenchymal intracranial pressure monitoring for hydrocephalus and cerebrospinal fluid disorders. Acta Neurochir 159(10):1967–1978
Craven CL, Ramkumar R, D’Antona L, Thompson SD, Thorne L, Watkins LD, Toma AK (2019) Natural history of ventriculomegaly in adults: a cluster analysis. J Neurosurg:1–8. https://doi.org/10.3171/2018.8.JNS18119
D’Antona L, Blamey SC, Craven CL et al (2019) Early postoperative outcomes of normal pressure hydrocephalus: results of a service evaluation. J Neurosurg Anesthesiol. https://doi.org/10.1097/ANA.0000000000000668
Eide PK, Sorteberg W (2010) Diagnostic intracranial pressure monitoring and surgical management in idiopathic normal pressure hydrocephalus: a 6-year review of 214 patients. Neurosurgery 66(1):80–91
Eide PK, Sorteberg W (2016) Outcome of surgery for idiopathic normal pressure hydrocephalus: role of preoperative static and pulsatile intracranial pressure. World Neurosurg 86:186–193.e1
Ferrari A, Milletti D, Giannini G et al (2020) The effects of cerebrospinal fluid tap-test on idiopathic normal pressure hydrocephalus: an inertial sensors based assessment. J Neuroeng Rehabil 17(1):7
Gasslander J, Sundström N, Eklund A, Koskinen L-OD, Malm J (2020) Risk factors for developing subdural hematoma: a registry-based study in 1457 patients with shunted idiopathic normal pressure hydrocephalus. J Neurosurg:1–10. https://doi.org/10.3171/2019.10.JNS191223
Gutowski P, Rot S, Fritsch M, Meier U, Gölz L, Lemcke J (2020) Secondary deterioration in patients with normal pressure hydrocephalus after ventriculoperitoneal shunt placement: a proposed algorithm of treatment. Fluids Barriers CNS 17(1):18
Kameda M, Yamada S, Atsuchi M, Kimura T, Kazui H, Miyajima M, Mori E, Ishikawa M, Date I (2017) Cost-effectiveness analysis of shunt surgery for idiopathic normal pressure hydrocephalus based on the SINPHONI and SINPHONI-2 trials. Acta Neurochir 159(6):995–1003
Kehler U, Kiefer M, Eymann R et al (2015) PROSAIKA: a prospective multicenter registry with the first programmable gravitational device for hydrocephalus shunting. Clin Neurol Neurosurg 137:132–136
Khan QUA, Wharen RE, Grewal SS, Thomas CS, Deen HGJ, Reimer R, Van Gerpen JA, Crook JE, Graff-Radford NR (2013) Overdrainage shunt complications in idiopathic normal-pressure hydrocephalus and lumbar puncture opening pressure. J Neurosurg 119(6):1498–1502
Lesniak MS, Clatterbuck RE, Rigamonti D, Williams MA (2002) Low pressure hydrocephalus and ventriculomegaly: hysteresis, non-linear dynamics, and the benefits of CSF diversion. Br J Neurosurg 16(6):555–561
Lutz BR, Venkataraman P, Browd SR (2013) New and improved ways to treat hydrocephalus: pursuit of a smart shunt. Surg Neurol Int 4(Suppl 1):S38–S50
Malem DN, Shand Smith JD, Toma AK, Sethi H, Kitchen ND, Watkins LD (2015) An investigation into the clinical impacts of lowering shunt opening pressure in idiopathic normal pressure hydrocephalus: A case series. Br J Neurosurg 29(1):18–22
Månsson PK, Hansen TS, Juhler M (2018) The applicability of fixed and adjustable gravitational shunt valves in two different clinical settings. Acta Neurochir 160(7):1415–1423
Michael AP, Elkouzi A, Elble RJ (2017) Pearls & Oy-sters: Low-pressure hydrocephalus and inadequate shunting. Neurology 88(17):e174–e177
Momjian S, Owler BK, Czosnyka Z, Czosnyka M, Pena A, Pickard JD (2004) Pattern of white matter regional cerebral blood flow and autoregulation in normal pressure hydrocephalus. Brain 127(Pt 5):965–972
Mori E, Ishikawa M, Kato T et al (2012) Guidelines for management of idiopathic normal pressure hydrocephalus: second edition. Neurol Med Chir (Tokyo) 52(11):775–809
Pang D, Altschuler E (1994) Low-pressure hydrocephalic state and viscoelastic alterations in the brain. Neurosurgery 35(4):643–646
Petersen J, Hellström P, Wikkelsø C, Lundgren-Nilsson A (2014) Improvement in social function and health-related quality of life after shunt surgery for idiopathic normal-pressure hydrocephalus. J Neurosurg 121(4):776–784
Pujari S, Kharkar S, Metellus P, Shuck J, Williams MA, Rigamonti D (2008) Normal pressure hydrocephalus: long-term outcome after shunt surgery. J Neurol Neurosurg Psychiatry 79(11):1282–1286
Relkin N, Marmarou A, Klinge P, Bergsneider M, Black PM (2005) Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery 57(3 Suppl):S4–S16 discussion ii-v
Salma A (2014) Normal pressure hydrocephalus as a failure of ICP homeostasis mechanism: the hidden role of Monro-Kellie doctrine in the genesis of NPH. Child’s Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 30(5):825–830
Sundström N, Lagebrant M, Eklund A, Koskinen L-OD, Malm J (2018) Subdural hematomas in 1846 patients with shunted idiopathic normal pressure hydrocephalus: treatment and long-term survival. J Neurosurg 129(3):797–804
Tanaka A, Kimura M, Nakayama Y, Yoshinaga S, Tomonaga M (1997) Cerebral blood flow and autoregulation in normal pressure hydrocephalus. Neurosurgery 40(6):1161–1167
Toma AK, Tarnaris A, Kitchen ND, Watkins LD (2011) Use of the proGAV shunt valve in normal-pressure hydrocephalus. Neurosurgery 68(2 Suppl Operative):245–249
Toma AK, Papadopoulos MC, Stapleton S, Kitchen ND, Watkins LD (2013) Systematic review of the outcome of shunt surgery in idiopathic normal-pressure hydrocephalus. Acta Neurochir 155(10):1977–1980
Trinh VT, Duckworth EAM (2013) Revision to an adjustable non-siphon control valve in low pressure hydrocephalus: therapeutic siphoning and a new perspective on NPH: series of 3 cases and review of the literature. Clin Neurol Neurosurg 115(2):175–178
Tschan CA, Antes S, Huthmann A, Vulcu S, Oertel J, Wagner W (2014) Overcoming CSF overdrainage with the adjustable gravitational valve proSA. Acta Neurochir 156(4):767–776 discussion 776
Williams MA, Malm J (2016) Diagnosis and treatment of idiopathic normal pressure hydrocephalus. Continuum (Minneap Minn) 22(2 Dementia):579–599
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Jonathan Funnell, Linda D’Antona and Claudia Craven. The first draft of the manuscript was written by Jonathan Funnell and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No funding was received for the conduction of this study. LD’s research fellowship is sponsored by B.Braun. LDW has received honoraria from and served on advisory boards for Medtronic, B. Braun and Codman. AKT research time was supported by the National Institute for Health Research University College London Hospitals Biomedical Research Centre. The other authors have no disclosures to report.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required. Informed consent was given by all patients for procedures described as part of their routine clinical management.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on CSF Circulation
Rights and permissions
About this article
Cite this article
Funnell, J.P., D’Antona, L., Craven, C.L. et al. Ultra-low-pressure hydrocephalic state in NPH: benefits of therapeutic siphoning with adjustable antigravity valves. Acta Neurochir 162, 2967–2974 (2020). https://doi.org/10.1007/s00701-020-04596-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-020-04596-z