Abstract
Background
The optimal management of pediatric craniopharyngiomas remains controversial. This study aimed to characterize long-term outcomes in a contemporary cohort of children undergoing surgery for craniopharyngiomas.
Methods
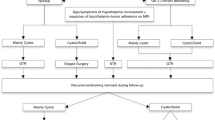
This was a retrospective review of 37 consecutive children who underwent surgery for craniopharyngioma with a median follow-up duration of 79 months (range 5–127 months). Patients were stratified by extent of resection (EOR) and need for adjuvant radiation therapy (RT). Imaging studies were reviewed to grade extent of hypothalamic involvement. Data on functional outcomes, pituitary function, and obesity were analyzed.
Results
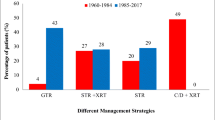
Gross total resection was achieved in 16 patients (43.2%), near total resection in six patients (16.2%), and subtotal resection (STR) in 15 patients (40.5%). The recurrence-free survival rate was 81.1% and 70.3% at 5- and 10-year follow-up, respectively. Survival analysis showed superior disease control in patients undergoing STR + RT (p = 0.008). Functional outcomes were independent of EOR, postoperative RT or recurrence. Diabetes insipidus was present in 75% and 44.4% of patients required >2 hormone replacements at last follow-up. Obesity was present in 36.1% patients after treatment, and was associated with preoperative obesity (p = 0.019), preoperative hypothalamic involvement (p = 0.047) and STR + RT (p = 0.011).
Conclusions
Gross or near total resection may be achieved safely in almost 60% of cases; however, radical surgery does not eliminate the risk of recurrence. Over long-term follow-up, STR + RT offers the best disease control rates. Patients with preoperative hypothalamic involvement, obesity, and those with tumors not amenable to radical resection are at risk for developing obesity on long-term follow-up.




Similar content being viewed by others
Abbreviations
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- EOR:
-
Extent of resection
- GTR:
-
Gross total resection
- MRI:
-
Magnetic resonance imaging
- NTR:
-
Near total resection
- OR:
-
Odds ratio
- RT:
-
Radiation therapy
- STR:
-
Subtotal resection
References
Albright AL, Hadjipanayis CG, Lunsford LD, Kondziolka D, Pollack IF, Adelson PD (2005) Individualized treatment of pediatric craniopharyngiomas. Childs Nerv Syst 21:649–654
Ali ZS, Bailey RL, Daniels LB, Vakhshori V, Lewis DJ, Hossain AT, Sitterley KY, Lee JY, Storm PB, Heuer GG (2014) Comparative effectiveness of treatment options for pediatric craniopharyngiomas. J Neurosurg Pediatr 13:178–188
Al-Mefty O, Hassounah M, Weaver P, Sakati N, Jinkins JR, Fox JL (1985) Microsurgery for giant craniopharyngiomas in children. Neurosurgery 17:585–595
Asirvatham JR, Deepti AN, Chyne R, Prasad M, Chacko AG, Rajshekhar V, Chacko G (2011) Pediatric tumors of the central nervous system: a retrospective study of 1,043 cases from a tertiary care center in South India. Childs Nerv Syst 27:1257–1263
Ciric IS, Cozzens JW (1980) Craniopharyngiomas: transsphenoidal method of approach—for the virtuoso only? Neurosurgery 27:169–187
Clark AJ, Cage TA, Aranda D, Parsa AT, Auguste KI, Gupta N (2012) Treatment-related morbidity and the management of pediatric craniopharyngioma: a systematic review. J Neurosurg Pediatr 10:293–301
Clark AJ, Cage TA, Aranda D, Parsa AT, Sun PP, Auguste KI, Gupta N (2013) A systematic review of the results of surgery and radiotherapy on tumor control for pediatric craniopharyngioma. Childs Nerv Syst 29:231–238
De Vile CJ, Grant DB, Kendall BE, Neville BG, Stanhope R, Watkins KE, Hayward RD (1996) Management of childhood craniopharyngioma: can the morbidity of radical surgery be predicted? J Neurosurg 85:73–81
Elliott RE, Hsieh K, Hochm T, Belitskaya-Levy I, Wisoff J, Wisoff JH (2010) Efficacy and safety of radical resection of primary and recurrent craniopharyngiomas in 86 children. J Neurosurg Pediatr 5:30–48
Elliott RE, Wisoff JH (2009) Successful surgical treatment of craniopharyngioma in very young children. J Neurosurg Pediatr 3:397–406
Elowe-Gruau E, Beltrand J, Brauner R, Pinto G, Samara-Boustani D, Thalassinos C, Busiah K, Laborde K, Boddaert N, Zerah M (2013) Childhood craniopharyngioma: hypothalamus-sparing surgery decreases the risk of obesity. J Clin Endocrinol Metab 98:2376–2382
Fahlbusch R, Honegger J, Paulus W, Huk W, Buchfelder M (1999) Surgical treatment of craniopharyngiomas: experience with 168 patients. J Neurosurg 90:237–250
Habrand JL, Ganry O, Couanet D, Rouxel V, Levy-Piedbois C, Pierre-Kahn A, Kalifa C (1999) The role of radiation therapy in the management of craniopharyngioma: a 25-year experience and review of the literature. Int J Radiat Oncol Biol Phys 44:255–263
Hoffman HJ, De Silva M, Humphreys RP, Drake JM, Smith ML, Blaser SI (1992) Aggressive surgical management of craniopharyngiomas in children. J Neurosurg 76:47–52
Karavitaki N, Brufani C, Warner J, Adams C, Richards P, Ansorge O, Shine B, Turner H, Wass J (2005) Craniopharyngiomas in children and adults: systematic analysis of 121 cases with long-term follow-up. Clin Endocrinol (Oxf) 62:397–409
Kim S-K, Wang K-C, Shin S-H, Choe G, Chi JG, Cho B-K (2001) Radical excision of pediatric craniopharyngioma: recurrence pattern and prognostic factors. Childs Nerv Syst 17:531–536
Koutourousiou M, Gardner PA, Fernandez-Miranda JC, Tyler-Kabara EC, Wang EW, Snyderman CH (2013) Endoscopic endonasal surgery for craniopharyngiomas: surgical outcome in 64 patients. J Neurosurg 119:1194–1207
Lin LL, El Naqa I, Leonard JR, Park TS, Hollander AS, Michalski JM, Mansur DB (2008) Long-term outcome in children treated for craniopharyngioma with and without radiotherapy. J Neurosurg Pediatr 1:126–130
Madsen PJ, Buch VP, Douglas JE, Parasher AK, Lerner DK, Alexander E, Workman AD, Palmer JN, Lang S-S, Kennedy BC (2019) Endoscopic endonasal resection versus open surgery for pediatric craniopharyngioma: comparison of outcomes and complications. J Neurosurg Pediatr 24:236–245
Marcus HJ, Rasul FT, Hussein Z, Baldeweg SE, Spoudeas HA, Hayward R, Thompson D, Grieve JP, Dorward NL, Aquilina K (2019) Craniopharyngioma in children: trends from a third consecutive single-center cohort study. J Neurosurg Pediatr 1:1–9. https://doi.org/10.3171/2019.10.PEDS19147
Mazzatenta D, Zoli M, Guaraldi F, Ambrosi F, Fustini MF, Pasquini E, Asioli S, Zucchelli M (2020) Outcome of endoscopic endonasal surgery in pediatric craniopharyngiomas. World Neurosurg 134:e277–e288
Merchant TE, Kiehna EN, Kun LE, Mulhern RK, Li C, Xiong X, Boop FA, Sanford RA (2006) Phase II trial of conformal radiation therapy for pediatric patients with craniopharyngioma and correlation of surgical factors and radiation dosimetry with change in cognitive function. J Neurosurg Pediatr 104:94–102
Merchant TE, Kiehna EN, Sanford RA, Mulhern RK, Thompson SJ, Wilson MW, Lustig RH, Kun LE (2002) Craniopharyngioma: the St. Jude children’s research hospital experience 1984–2001. Int J Radiat Oncol Biol Phys 53:533–542
Moon SH, Kim IH, Park SW, Kim I, Hong S, Park CI, Wang KC, Cho BK (2005) Early adjuvant radiotherapy toward long-term survival and better quality of life for craniopharyngiomas—a study in single institute. Childs Nerv Syst 21:799–807
Mortini P, Losa M, Pozzobon G, Barzaghi R, Riva M, Acerno S, Angius D, Weber G, Chiumello G, Giovanelli M (2011) Neurosurgical treatment of craniopharyngioma in adults and children: early and long-term results in a large case series. J Neurosurg 114:1350–1359
Müller HL, Emser A, Faldum A, Bruhnken G, Etavard-Gorris N, Gebhardt U, Oeverink R, Kolb R, Sörensen N (2004) Longitudinal study on growth and body mass index before and after diagnosis of childhood craniopharyngioma. J Clin Endocrinol Metab 89:3298–3305
Pierre-Kahn A, Recassens C, Pinto G, Thalassinos C, Chokron S, Soubervielle J, Brauner R, Zerah M, Sainte Rose C (2005) Social and psycho-intellectual outcome following radical removal of craniopharyngiomas in childhood. Childs Nerv Syst 21:817–824
Pratheesh R, Swallow DM, Joseph M, Natesan D, Rajaratnam S, Jacob K, Chacko AG (2015) Evaluation of a protocol-based treatment strategy for postoperative diabetes insipidus in craniopharyngioma. Neurology India 63:712
Pratheesh R, Swallow DMA, Rajaratnam S, Jacob K, Chacko G, Joseph M, Chacko AG (2013) Incidence, predictors and early post-operative course of diabetes insipidus in paediatric craniopharygioma: a comparison with adults. Childs Nerv Syst 29:941–949
Puget S, Garnett M, Wray A, Grill J, Habrand J-L, Bodaert N, Zerah M, Bezerra M, Renier D, Pierre-Kahn A (2007) Pediatric craniopharyngiomas: classification and treatment according to the degree of hypothalamic involvement. J Neurosurg Pediatr 106:3–12
Rosenfeld A, Arrington D, Miller J, Olson M, Gieseking A, Etzl M, Harel B, Schembri A, Kaplan A (2014) A review of childhood and adolescent craniopharyngiomas with particular attention to hypothalamic obesity. Pediatr Neurol 50:4–10
Sainte-Rose C, Puget S, Wray A, Zerah M, Grill J, Brauner R, Boddaert N, Pierre-Kahn A (2005) Craniopharyngioma: the pendulum of surgical management. Childs Nerv Syst 21:691–695
Sands SA, Milner JS, Goldberg J, Mukhi V, Moliterno JA, Maxfield C, Wisoff JH (2005) Quality of life and behavioral follow-up study of pediatric survivors of craniopharyngioma. J Neurosurg Pediatr 103:302–311
Schubert T, Trippel M, Tacke U, Van Velthoven V, Gumpp V, Bartelt S, Ostertag C, Nikkhah G (2009) Neurosurgical treatment strategies in childhood craniopharyngiomas: is less more? Childs Nerv Syst 25:1419
Steinbok P, Hukin J (2010) Intracystic treatments for craniopharyngioma. Neurosurg Focus 28:E13
Stripp DC, Maity A, Janss AJ, Belasco JB, Tochner ZA, Goldwein JW, Moshang T, Rorke LB, Phillips PC, Sutton LN (2004) Surgery with or without radiation therapy in the management of craniopharyngiomas in children and young adults. Int J Radiat Oncol Biol Phys 58:714–720
Thompson D, Phipps K, Hayward R (2005) Craniopharyngioma in childhood: our evidence-based approach to management. Childs Nerv Syst 21:660–668
Tomei G, Bello L, Sganzerla E, Ambrosi B, Re T, Barilari MG, Villani R (1997) Long-term results of treatment for craniopharyngioma in children. Childs Nerv Syst 13:397–405
Van Effenterre R, Boch A-L (2002) Craniopharyngioma in adults and children: a study of 122 surgical cases. J Neurosurg 97:3–11
Vinchon M, Dhellemmes P (2008) Craniopharyngiomas in children: recurrence, reoperation and outcome. Childs Nerv Syst 24:211–217
Vinchon M, Weill J, Delestret I, Dhellemmes P (2009) Craniopharyngioma and hypothalamic obesity in children. Childs Nerv Syst 25:347
Visser J, Hukin J, Sargent M, Steinbok P, Goddard K, Fryer C (2010) Late mortality in pediatric patients with craniopharyngioma. J Neurooncol 100:105–111
Wang KC, Kim SK, Choe G, Chi JG, Cho B-K (2002) Growth patterns of craniopharyngioma in children: role of the diaphragm sellae and its surgical implication. Surg Neurol 57:25–33
Wen BC, Hussey DH, Staples J, Hitchon PW, Jani SK, Vigliotti AP, Doornbos JF (1989) A comparison of the roles of surgery and radiation therapy in the management of craniopharyngiomas. Int J Radiat Oncol Biol Phys 16:17–24
Yano S, Kudo M, Hide T, Shinojima N, Makino K, Nakamura H, Kuratsu J-i (2016) Quality of life and clinical features of long-term survivors surgically treated for pediatric craniopharyngioma. World Neurosurg 85:153–162
Yaşargil MG, Curcic M, Kis M, Siegenthaler G, Teddy PJ, Roth P (1990) Total removal of craniopharyngiomas: approaches and long-term results in 144 patients. J Neurosurg 73:3–11
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Sauradeep Sarkar and Shireen Chacko. The first draft of the manuscript was written by Sauradeep Sarkar, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (name of institute/committee) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study formal consent is not required.
Additional information
Comments
The authors present a single-surgeon cohort of paediatric craniopharyngioma managed along a single, clear and uniform pathway. They describe 37 patients, with a mean age of ten, followed up for a median of 79 months, including 27 patients for five years and over; none of the patients were lost to follow up, although two died within two years. 16 underwent gross total resection, 6 near total and 15 subtotal resection; almost all surgery was transcranial. Complication rates are within the expected range; 75% had diabetes insipidus on long-term follow up. Recurrence free survival rates were 81% at five years and 70.3% at ten years. The authors make a number of conclusions; most importantly they demonstrate that radical surgery does not eliminate the risk of long-term recurrence, that the combination of subtotal resection and radiotherapy leads to the best disease control rates, and that surgical complications were independent of the extent of resection.This is not new territory, and the problems and controversies related to the holistic management of paediatric craniopharyngioma have been extensively presented in the literature over the past ten years. The value of this study lies in the robust and consistent management paradigm, describing a paediatric population that has been followed up closely.
Kristen Aquilina
London, UK
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pediatric Neurosurgery
Rights and permissions
About this article
Cite this article
Sarkar, S., Chacko, S.R., Korula, S. et al. Long-term outcomes following maximal safe resection in a contemporary series of childhood craniopharyngiomas. Acta Neurochir 163, 499–509 (2021). https://doi.org/10.1007/s00701-020-04591-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-020-04591-4