Abstract
Background
Stereotactic radiosurgery such as Gamma Knife radiosurgery (GKRS) has been shown to have a good treatment effect for orbital cavernous venous malformation (CVM). However, radiation-induced retinopathy or optic neuropathy is a vision-threatening complication of orbital irradiation. Predicting the post-treatment visual outcome is critical.
Methods
Clinical and radiological outcomes were investigated in 30 patients who underwent GKRS for orbital CVM between July 2005 and February 2020. Measurement of peripapillary retinal nerve fiber layer (pRNFL) thickness using optical coherence tomography (OCT) was obtained in 14 patients.
Results
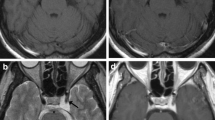
The median clinical and radiological follow-up periods were 46.6 months (range, 15.9–105.8) and 27.5 months (range, 15.4–105.8), respectively. Twenty-eight patients underwent multisession (4 fractions) GKRS. The median cumulative marginal dose was 20 Gy (range, 16–24). Two patients underwent single-session GKRS. Marginal doses were 15 Gy and 10.5 Gy in each patient. The volume of CVM decreased in 29 (97%) patients. Visual acuity was improved in 6 (20%) patients and was stable in 22 (73%) patients. Visual field defect and exophthalmos were improved in all patients. Serial investigation of OCT showed no statistically significant difference in pRNFL thickness after GKRS. Patients with normal average pRNFL thickness showed better visual recovery than patients with thin average pRNFL thickness.
Conclusions
GKRS is an effective and safe treatment option for orbital CVM. The pRNFL thickness before GKRS can be a prognostic indicator for visual recovery in orbital CVM after GKRS.


Similar content being viewed by others
Data availability
Not applicable.
References
Ares WJ, Flickinger JC, Lunsford LD (2019) Leksell radiosurgery for orbital, uveal, and choroidal tumors. Prog Neurol Surg 34:298–305
Arnett ALH, Reynolds MM, Pulido JS, Parney IF, Laack NN (2017) Gamma Knife stereotactic radiosurgery for the treatment of primary and metastatic ocular malignancies. Stereotact Funct Neurosurg 95:363–368
Bagheri A, Jafari R, Salour H, Aletaha M, Yazdani S, Baghi S (2018) A new surgical technique for excision of orbital cavernous hemangioma: a 15-year experience. Orbit 37:429–437
Bekdemir S, Gunduz AK, Ersoz CC (2020) Orbital cavernous hemangioma presenting with a dome-shaped maculopathy-like appearance on swept-source optical tomography imaging. Case Rep Ophthalmol Med 2020:5354609
Budenz DL, Anderson DR, Varma R, Schuman J, Cantor L, Savell J, Greenfield DS, Patella VM, Quigley HA, Tielsch J (2007) Determinants of normal retinal nerve fiber layer thickness measured by Stratus OCT. Ophthalmology 114:1046–1052
Calandriello L, Grimaldi G, Petrone G, Rigante M, Petroni S, Riso M, Savino G (2017) Cavernous venous malformation (cavernous hemangioma) of the orbit: current concepts and a review of the literature. Surv Ophthalmol 62:393–403
Chung KS, Chang WS, Chang JH, Lee SC, Chang JW, Park YG, Jung HH (2020) Gamma Knife radiosurgery for choroidal hemangioma: a single-institute series. World Neurosurg 133:e129–e134
Colletti G, Biglioli F, Poli T, Dessy M, Cucurullo M, Petrillo M, Tombris S, Waner M, Sesenna E (2019) Vascular malformations of the orbit (lymphatic, venous, arteriovenous): diagnosis, management and results. J Craniomaxillofac Surg 47:726–740
Danesh-Meyer HV, Papchenko T, Savino PJ, Law A, Evans J, Gamble GD (2008) In vivo retinal nerve fiber layer thickness measured by optical coherence tomography predicts visual recovery after surgery for parachiasmal tumors. Invest Ophthalmol Vis Sci 49:1879–1885
Dsouza S, Kandula P, Kamath G, Kamath M (2017) Clinical profile of unilateral proptosis in a tertiary care centre. J Ophthalmol 2017:8546458
Goh ASC, Kim YD, Woo KI, Lee JI (2013) Benign orbital apex tumors treated with multisession Gamma Knife radiosurgery. Ophthalmology 120:635–641
Haas A, Pinter O, Papaefthymiou G, Weger M, Berghold A, Schrottner O, Mullner K, Pendl G, Langmann G (2002) Incidence of radiation retinopathy after high-dosage single-fraction Gamma Knife radiosurgery for choroidal melanoma. Ophthalmology 109:909–913
Hamed-Azzam S, Verity DH, Rose GE (2018) Lateral canthotomy orbitotomy: a rapid approach to the orbit. Eye (Lond) 32:333–337
Iorga RE, Moraru A, Ozturk MR, Costin D (2018) The role of optical coherence tomography in optic neuropathies. Rom J Ophthalmol 62:3–14
Jayaram A, Cohen LM, Lissner GS, Karagianis AG (2017) A retrospective review of cases preoperatively diagnosed by radiologic imaging as cavernous venous malformations. Orbit 36:128–134
Jeon C, Park KA, Hong SD, Choi JW, Seol HJ, Nam DH, Lee JI, Shin HJ, Kong DS (2019) Clinical efficacy of optical coherence tomography to predict the visual outcome after endoscopic endonasal surgery for suprasellar tumors. World Neurosurg 132:e722–e731
Jo KI, Im YS, Kong DS, Seol HJ, Nam DH, Kim YD, Lee JI (2012) Multisession Gamma Knife surgery for benign orbital tumors. J Neurosurg 117(Suppl):102–107
Johnson S, Niranjan A, Kano H, Lunsford LD (2019) Leksell radiosurgery for the 3 H tumors: hemangiomas, hemangioblastomas, and hemangiopericytomas. Prog Neurol Surg 34:223–231
Jones B, Dale RG, Deehan C, Hopkins KI, Morgan DA (2001) The role of biologically effective dose (BED) in clinical oncology. Clin Oncol (R Coll Radiol) 13:71–81
Jung S, Bosch A, Ott C, Kannenkeril D, Dienemann T, Harazny JM, Michelson G, Schmieder RE (2020) Retinal neurodegeneration in patients with end-stage renal disease assessed by spectral-domain optical coherence tomography. Sci Rep 10:5255
Khan AA, Niranjan A, Kano H, Kondziolka D, Flickinger JC, Lunsford LD (2009) Stereotactic radiosurgery for cavernous sinus or orbital hemangiomas. Neurosurgery 65:914–918 discussion 918
Khan SN, Sepahdari AR (2012) Orbital masses: CT and MRI of common vascular lesions, benign tumors, and malignancies. Saudi J Ophthalmol 26:373–383
Kim BS, Im YS, Woo KI, Kim YD, Lee JI (2015) Multisession Gamma Knife radiosurgery for orbital apex tumors. World Neurosurg 84:1005–1013
Kim CY, Lee SY (2012) Orbital paraganglioma: Gamma Knife surgery as a therapeutic option. J Craniofac Surg 23:1127–1128
Kim MS, Park K, Kim JH, Kim YD, Lee JI (2008) Gamma Knife radiosurgery for orbital tumors. Clin Neurol Neurosurg 110:1003–1007
Kim YT, Kang SW, Lee JI (2011) Gamma Knife radiosurgery for choroidal hemangioma. Int J Radiat Oncol Biol Phys 81:1399–1404
Liu D, Li Y, Zhang Y, Zhang Z, Song G, Xu D (2018) Volume-staged Gamma Knife radiosurgery for orbital venous malformations. J Neurosurg 129:26–30
Liu X, Xu D, Zhang Y, Liu D, Song G (2010) Gamma Knife surgery in patients harboring orbital cavernous hemangiomas that were diagnosed on the basis of imaging findings. J Neurosurg 113(Suppl):39–43
Loo JL, Tian J, Miller NR, Subramanian PS (2013) Use of optical coherence tomography in predicting post-treatment visual outcome in anterior visual pathway meningiomas. Br J Ophthalmol 97:1455–1458
Maberley DA, Hollands H, Chuo J, Tam G, Konkal J, Roesch M, Veselinovic A, Witzigmann M, Bassett K (2006) The prevalence of low vision and blindness in Canada. Eye (Lond) 20:341–346
Milano MT, Grimm J, Soltys SG, Yorke E, Moiseenko V, Tome WA, Sahgal A, Xue J, Ma L, Solberg TD, Kirkpatrick JP, Constine LS, Flickinger JC, Marks LB, El Naqa I (2018) Single- and multi-fraction stereotactic radiosurgery dose tolerances of the optic pathways. Int J Radiat Oncol Biol Phys. https://doi.org/10.1016/j.ijrobp.2018.01.053
Millar WT, Hopewell JW, Paddick I, Lindquist C, Nordstron H, Lidberg P, Garding J (2015) The role of the concept of biologically effective dose (BED) in treatment planning in radiosurgery. Phys Med 31:627–633
Modorati GM, Dagan R, Mikkelsen LH, Andreasen S, Ferlito A, Bandello F (2020) Gamma Knife radiosurgery for uveal melanoma: a retrospective review of clinical complications in a tertiary referral center. Ocul Oncol Pathol 6:115–122
Niyazi M, Brada M, Chalmers AJ, Combs SE, Erridge SC, Fiorentino A, Grosu AL, Lagerwaard FJ, Minniti G, Mirimanoff RO, Ricardi U, Short SC, Weber DC, Belka C (2016) ESTRO-ACROP guideline “target delineation of glioblastomas”. Radiother Oncol 118:35–42
Paddick I, Lippitz B (2006) A simple dose gradient measurement tool to complement the conformity index. J Neurosurg 105(Suppl):194–201
Ratnayake GS, McNab AA, Dally MJ, Zajarski C, Senthi S, Ruben JD (2019) Fractionated stereotactic radiotherapy for cavernous venous malformations of the orbital apex. Ophthalmic Plast Reconstr Surg 35:322–325
Scheuerle AF, Steiner HH, Kolling G, Kunze S, Aschoff A (2004) Treatment and long-term outcome of patients with orbital cavernomas. Am J Ophthalmol 138:237–244
Schmidt P, Kempin R, Langner S, Beule A, Kindler S, Koppe T, Volzke H, Ittermann T, Jurgens C, Tost F (2019) Association of anthropometric markers with globe position: a population-based MRI study. PLoS One 14:e0211817
Seibel I, Cordini D, Hager A, Tillner J, Riechardt AI, Heufelder J, Davids AM, Rehak M, Joussen AM (2016) Predictive risk factors for radiation retinopathy and optic neuropathy after proton beam therapy for uveal melanoma. Graefes Arch Clin Exp Ophthalmol 254:1787–1792
Shchurova IN, Pronin IN, Mel’nikova-Pitskhelauri TV, Serova NK, Grigor'eva NN, Fadeeva LM, Shishkina LV (2018) Orbital hemangiomas: capabilities of modern neuroradiological diagnostics. Zh Vopr Neirokhir Im N N Burdenko 82:57–69
Singh D, Pushker N, Bajaj MS, Saxena R, Sharma S, Ghose S (2012) Visual function alterations in orbital tumors and factors predicting visual outcome after surgery. Eye (Lond) 26:448–453
Tailor TD, Gupta D, Dalley RW, Keene CD, Anzai Y (2013) Orbital neoplasms in adults: clinical, radiologic, and pathologic review. Radiographics 33:1739–1758
Tanaka A, Mihara F, Yoshiura T, Togao O, Kuwabara Y, Natori Y, Sasaki T, Honda H (2004) Differentiation of cavernous hemangioma from schwannoma of the orbit: a dynamic MRI study. AJR Am J Roentgenol 183:1799–1804
Tata A, Cohen-Inbar O, Sheehan JP (2016) Treatment of orbital solitary fibrous tumour with Gamma Knife radiosurgery and systematic review of literature. BMJ Case Rep 2016. https://doi.org/10.1136/bcr-2016-217114
Thompson TP, Lunsford LD, Flickinger JC (2000) Radiosurgery for hemangiomas of the cavernous sinus and orbit: technical case report. Neurosurgery 47:778–783
Xu D, Liu D, Zhang Z, Zhang Y, Li Y, Liu X, Jia Q, Zheng L, Song G (2010) Gamma Knife surgery in the management of orbital tumors. J Neurosurg 113(Suppl):34–38
Xu D, Liu D, Zhang Z, Zhang Y, Song G (2011) Gamma Knife radiosurgery for primary orbital varices: a preliminary report. Br J Ophthalmol 95:1264–1267
Young SM, Kim KH, Kim YD, Lang SS, Park JW, Woo KI, Lee JI (2019) Orbital apex venous cavernous malformation with optic neuropathy: treatment with multisession Gamma Knife radiosurgery. Br J Ophthalmol 103:1453–1459
Young SM, Kim YD, Lee JH, Woo KI (2018) Radiological analysis of orbital cavernous hemangiomas: a review and comparison between computed tomography and magnetic resonance imaging. J Craniofac Surg 29:712–716
Zamber RW, Kinyoun JL (1992) Radiation retinopathy. West J Med 157:530–533
Acknowledgments
The authors thank Hee Yae An, R.N., and Yong-Seok Im, PhD., of the Department of Neurosurgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, who assisted with data collection and technical support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Samsung Medical Center Institutional Review Board) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Code availability
Not applicable.
Additional information
Comments
Won Jae Lee et al have investigated clinical and radiological outcome in 30 patients who underwent GKRS for orbital cavernous venous malformations. This unique series is demonstrating GKRS to be an effective and very safe alternative to resection surgery. Very interestingly the authors have used optical coherence tomography (OCT) in 14 patients in order to study the predictive value of peripapillary retinal nerve fiber layer (pRNFL) thickness. They found no post-radiosurgery change in pRNFL. More importantly they have shown that patients with normal average pRNFL thickness were demonstrating a better visual recovery. However, it is a retrospective heterogeneous series. All the patients were not treated using the same protocol (single versus hypofractionation) not all the patients were investigated with OCT. Their use of the linear quadratic formula and BED for single dose is nowadays not consensual. The absence of eye ball fixation during imaging and SRS is also a potential matter of debate.
Anyway, this is a very convincing paper which may affect, in the future the management of these patients.
Jean Marie Regis
Marseille, France
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Presentation at a conference
None.
This article is part of the Topical Collection on Tumor - Other
Rights and permissions
About this article
Cite this article
Lee, W.J., Cho, KR., Choi, JW. et al. Stereotactic radiosurgery for orbital cavernous venous malformation: a single center’s experience for 15 years. Acta Neurochir 163, 357–364 (2021). https://doi.org/10.1007/s00701-020-04575-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-020-04575-4