Abstract
Background
The function-based resection using trans-cortical approach for removing insular diffuse glioma shares a positive benefit-to-risk ratio with a low rate of permanent morbidity.
Method
The technique requires intraoperative functional brain mapping to be performed under awake condition using direct electrical stimulations at both cortical and subcortical levels to identify brain connectivity supporting neurocognition.
Conclusion
The trans-cortical approach is a safe and efficient technique to remove insular diffuse glioma. Intraoperative functional brain mapping under awake condition allows preserving brain connectivity and tailoring the resection. Great care must be taken in preventing vascular damages, and particularly the lenticulostriate arteries.



Similar content being viewed by others
References
Benet A, Hervey-Jumper SL, Sánchez JJG, Lawton MT, Berger MS (2016) Surgical assessment of the insula. Part 1: surgical anatomy and morphometric analysis of the transsylvian and transcortical approaches to the insula. J Neurosurg 124(2):469–481
De Witt Hamer PC, Robles SG, Zwinderman AH, Duffau H, Berger MS (2012) Impact of intraoperative stimulation brain mapping on glioma surgery outcome: a meta-analysis. J Clin Oncol Off J Am Soc Clin Oncol 30(20):2559–2565
Di Carlo DT, Cagnazzo F, Anania Y, Duffau H, Benedetto N, Morganti R, Perrini P (2020) Post-operative morbidity ensuing surgery for insular gliomas: a systematic review and meta-analysis. Neurosurg Rev 43(3):987–997
Duffau H (2009) A personal consecutive series of surgically treated 51 cases of insular WHO Grade II glioma: advances and limitations. J Neurosurg 110(4):696–708
Murrone D, Maduri R, Afif A, Chirchiglia D, Pelissou-Guyotat I, Guyotat J, Signorelli F (2019) Insular gliomas: a surgical reappraisal based on a systematic review of the literature. J Neurosurg Sci 63(5):566–580
Pallud J, Dezamis E (2017) Functional and oncological outcomes following awake surgical resection using intraoperative cortico-subcortical functional mapping for supratentorial gliomas located in eloquent areas. Neurochirurgie 63(3):208–218
Pallud J, Mandonnet E, Corns R, Dezamis E, Parraga E, Zanello M, Spena G (2017) Technical principles of direct bipolar electrostimulation for cortical and subcortical mapping in awake craniotomy. Neurochirurgie. https://doi.org/10.1016/j.neuchi.2016.12.004
Przybylowski CJ, Baranoski JF, So VM, Wilson J, Sanai N (2019) Surgical morbidity of transsylvian versus transcortical approaches to insular gliomas. J Neurosurg:1–8
Türe U, Yaşargil DC, Al-Mefty O, Yaşargil MG (1999) Topographic anatomy of the insular region. J Neurosurg 90(4):720–733
Yaşargil MG, von Ammon K, Cavazos E, Doczi T, Reeves JD, Roth P (1992) Tumours of the limbic and paralimbic systems. Acta Neurochir 118(1–2):40–52
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Patient consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Key points
- Awake condition optimizes the benefit-to-risk ratio.
- Preoperative neurocognitive evaluation and patient’s preparation are keys to successful awake surgery.
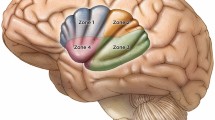
- The positive cortical mapping tailors the trans-cortical approach.
- The positive subcortical mapping tailors the deep limits of resection.
- Subpial dissection avoids damaging the sylvian vascularization, and vascular boundaries have to be respected.
- Transient postoperative neurological and neurocognitive worsening requires rehabilitation.
- Permanent postoperative neurological deficit related to vascular injury occurs < 5%.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Brain Tumors
The manuscript has not been previously published in whole or in part or submitted elsewhere for review.
Electronic supplementary material
Video 1
Illustration of the key steps of a function-based resection under awake condition of an insular diffuse glioma using the trans-cortical approach (MOV 36979 kb)
Rights and permissions
About this article
Cite this article
Roux, A., Dezamis, E., Trancart, B. et al. How I do it: trans-cortical approach for insular diffuse glioma. Acta Neurochir 162, 3025–3030 (2020). https://doi.org/10.1007/s00701-020-04553-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-020-04553-w