Abstract
Background
Giant middle cerebral artery aneurysms are frequently anatomically complicated. Trapping may yield poor outcome, and bypass revascularization is often necessary as an adjunctive treatment to preserve flow.
Method
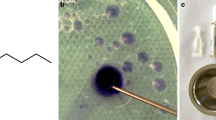
The technical nuances of superficial temporal artery to middle cerebral artery bypass are described in the setting of clip reconstruction of giant middle cerebral artery (MCA) aneurysm. In addition to an operative video, the anatomy and surgical technique are demonstrated in virtual reality to enhance the didactic clarity.
Conclusion
Meticulous technique is paramount for successful superficial temporal artery MCA bypass. Along with clip reconstruction, it is a critical part of the treatment of complex, giant MCA aneurysms.



Similar content being viewed by others
Abbreviations
- ICG:
-
Indocyanine green
- MCA:
-
Middle cerebral artery
- STA:
-
Superficial temporal artery
- VR:
-
Virtual reality
References
Amin-Hanjani S, Alaraj A, Charbel FT (2010) Flow replacement bypass for aneurysms: decision-making using intraoperative blood flow measurements. Acta Neurochir. https://doi.org/10.1007/s00701-010-0635-4
Benashvili GM, Alexander LF, Zubkov YN (1992) Thrombosis of a giant aneurysm after extracranial-intracranial bypass. Neurosurgery. https://doi.org/10.1227/00006123-199208000-00025
Cantore G, Santoro A, Da Pian R (1999) Spontaneous occlusion of supraclinoid aneurysms after the creation of extra-intracranial bypasses using long grafts: report of two cases. Neurosurgery. https://doi.org/10.1097/00006123-199901000-00132
Kalani YSM, Zabramski JM, Hu YC, Spetzler RF (2013) Extracranial-intracranial bypass and vessel occlusion for the treatment of unclippable giant middle cerebral artery aneurysms. Neurosurgery. https://doi.org/10.1227/NEU.0b013e3182804381
Rinne J, Hernesniemi J, Niskanen M, Vapalahti M (1996) Analysis of 561 patients with 690 middle cerebral artery aneurysms: anatomic and clinical features as correlated to management outcome. Neurosurgery. https://doi.org/10.1097/00006123-199601000-00002
da Silva HB, Messina-Lopez M, Sekhar LN (2014) Bypasses and reconstruction for complex brain aneurysms. Methodist Debakey Cardiovasc J. https://doi.org/10.14797/mdcj-10-4-224
Xu F, Xu B, Huang L, Xiong J, Gu Y, Lawton MT (2018) Surgical treatment of large or giant fusiform middle cerebral artery aneurysms: a case series. World Neurosurg. https://doi.org/10.1016/j.wneu.2018.04.031
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent statement
The patient has consented to submission of this How I Do It to the Acta Neurochirurgica.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
1. Detailed review of preoperative anatomy is crucial for identification of the inflow-outflow of the aneurysm and potential recipients of the bypass graft.
2. Donor vessels must be harvested patiently with sufficient length to avoid tension at the anastomosis.
3. Fish-mouthing the donor vessel aids in increasing surface area for blood flow.
4. Although interrupted suture requires more time, it keeps the operative less cluttered and has a lower risk of constricting the anastomosis.
5. A wide fissure dissection helps with aneurysm exposure, identification of parent artery, critical perforators, and recipient vessels. This allows for safer trapping of the aneurysm.
6. De-magnetized instruments and technical proficiency in microsurgical anastomosis are paramount to successful revascularization.
7. Intraoperative flow assessment, including ICG, Doppler, and angiogram, should be liberally used to assess patency of the bypass and critical branches. Adjustments of the clip reconstruction are often necessary based on this assessment.
8. Confirming immaculate hemostasis and patency of the graft minimizes postoperative complications.
9. Postoperative strict blood pressure control, hydration, and the use of heparin/aspirin can mitigate postoperative complications.
10. Preoperative examination in virtual reality may prove useful to clarify the anatomy and plan for the configuration of the necessary clips and for the bypass.
This article is part of the Topical Collection on Vascular Neurosurgery - Aneurysm
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Jean, W.C., Felbaum, D.R. & Ngo, H.M. How I do it: superficial temporal artery to middle cerebral artery bypass for treatment of giant middle cerebral artery aneurysm. Acta Neurochir 162, 593–596 (2020). https://doi.org/10.1007/s00701-019-04202-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-04202-x