Abstract
Background
Previous studies have not evaluated the impact of illness severity and postrupture procedures in the cost of care for intracranial aneurysms. We hypothesize that the severity of aneurysm rupture and the aggressiveness of postrupture interventions play a role in cost.
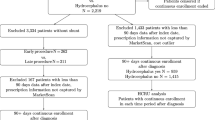
Methods
The Value Driven Outcomes database was used to assess direct patient cost during the treatment of ruptured intracranial aneurysm with clipping, coiling, and Pipeline flow diverters.
Results
One hundred ninety-eight patients (mean age 52.8 ± 14.1 years; 40.0% male) underwent craniotomy (64.6%), coiling (26.7%), or flow diversion (8.6%). Coiling was 1.4× more expensive than clipping (p = .005) and flow diversion was 1.7× more expensive than clipping (p < .001). More severe illness as measured by American Society of Anesthesia, Hunt/Hess, and Fisher scales incurred higher costs than less severe illness (p < .05). Use of a lumbar drain protocol to reduce subarachnoid hemorrhage and use of an external ventricular drain to manage intracranial pressure were associated with reduced (p = .05) and increased (p < .001) total costs, respectively. Patients with severe vasospasm (p < .005), those that received shunts (p < .001), and those who had complications (p < .001) had higher costs. Multivariate analysis showed that procedure type, length of stay, number of angiograms, vasospasm severity, disposition, and year of treatment were independent predictors of cost.
Conclusions
These results show for the first time that disease and vasospasm severity and intensity of treatment directly impact the cost of care for patients with aneurysms in the USA. Strategies to alter these variables may prove important for cost reduction.




Similar content being viewed by others
Abbreviations
- NIS:
-
National Inpatient Sample
- VDO:
-
Value Driven Outcome
- ASA:
-
American Society of Anesthesiologists
- LOS:
-
Length of stay
- EVD:
-
External ventricular drain
- SAH:
-
Subarachnoid hemorrhage
- PCA:
-
Posterior cerebral artery
- SCA:
-
Superior cerebellar artery
- PICA:
-
Posterior inferior cerebellar artery
- AICA:
-
Anterior inferior cerebellar artery
References
Akhigbe T, Zolnourian A, Saadi F (2018) Cost economics of endovascular coiling versus surgical clipping of an intracranial aneurysm: literature review and critical analysis. Int J Med Rev Case Rep 2:17–21. https://doi.org/10.5455/IJMRCR.endovascular-coiling-surgical-clipping-intracranial-aneurysm-economics
Bekelis K, Missios S, MacKenzie TA, Labropoulos N, Roberts DW (2016) A predictive model of hospitalization cost after cerebral aneurysm clipping. J Neurointerv Surg 8:316–322. https://doi.org/10.1136/neurintsurg-2014-011575
Bekelis K, Gottlieb D, Su Y, Labropoulos N, Bovis G, Lawton MT, MacKenzie TA (2017) Medicare expenditures for elderly patients undergoing surgical clipping or endovascular intervention for unruptured cerebral aneurysms. J Neurointerv Surg 9:324–328. https://doi.org/10.1136/neurintsurg-2016-012313
Chalouhi N, Hoh BL, Hasan D (2013) Review of cerebral aneurysm formation, growth, and rupture. Stroke 44:3613–3622. https://doi.org/10.1161/STROKEAHA.113.002390
Chiu AH, Nadarajah M, Wenderoth JD (2013) Cost analysis of intracranial aneurysmal repair by endovascular coiling versus flow diversion: at what size should we use which method? J Med Imaging Radiat Oncol 57:423–426. https://doi.org/10.1111/1754-9485.12040
Duan Y, Blackham K, Nelson J, Selman W, Bambakidis N (2015) Analysis of short-term total hospital costs and current primary cost drivers of coiling versus clipping for unruptured intracranial aneurysms. J Neurointerv Surg 7:614–618. https://doi.org/10.1136/neurintsurg-2014-011249
El-Chalouhi N, Jabbour PM, Tjoumakaris SI, Starke RM, Dumont AS, Liu H, Rosenwasser R, El Moursi S, Gonzalez LF (2014) Treatment of large and giant intracranial aneurysms: cost comparison of flow diversion and traditional embolization strategies. World Neurosurg 82:696–701. https://doi.org/10.1016/j.wneu.2013.02.089
Familiari P, Maldaner N, Kursumovic A, Rath SA, Vajkoczy P, Raco A, Dengler J, Giant Intracranial Aneurysm Study G (2015) Cost comparison of surgical and endovascular treatment of unruptured giant intracranial aneurysms. Neurosurgery 77:733–741. https://doi.org/10.1227/NEU.0000000000000917
Finitsis S, Fahed R, Gaulin I, Roy D, Weill A (2018) Impact of coil price knowledge by the operator on the cost of aneurysm coiling. A single center study. J Neurointerv Surg 10:602–605. https://doi.org/10.1136/neurintsurg-2017-013323
Flahault A, Trystram D, Nataf F, Fouchard M, Knebelmann B, Grunfeld JP, Joly D (2018) Screening for intracranial aneurysms in autosomal dominant polycystic kidney disease is cost-effective. Kidney Int 93:716–726. https://doi.org/10.1016/j.kint.2017.08.016
Frontera JA, Moatti J, de los Reyes KM, McCullough S, Moyle H, Bederson JB, Patel A (2014) Safety and cost of stent-assisted coiling of unruptured intracranial aneurysms compared with coiling or clipping. J Neurointerv Surg 6:65–71. https://doi.org/10.1136/neurintsurg-2012-010544
Gandhoke GS, Pandya YK, Jadhav AP, Jovin T, Friedlander RM, Smith KJ, Jankowitz BT (2018) Cost of coils for intracranial aneurysms: clinical decision analysis for implementation of a capitation model. J Neurosurg 128:1792–1798. https://doi.org/10.3171/2017.3.JNS163149
Greving JP, Rinkel GJ, Buskens E, Algra A (2009) Cost-effectiveness of preventive treatment of intracranial aneurysms: new data and uncertainties. Neurology 73:258–265. https://doi.org/10.1212/01.wnl.0b013e3181a2a4ea
Gupta R, Griessenauer CJ, Adeeb N, Chua MH, Moore JM, Patel AS, Thomas AJ, Ogilvy CS (2016) Evaluating imaging follow-up strategies and costs of unruptured intracranial aneurysms treated with endovascular techniques: a survey of academic neurovascular centers in the United States. World Neurosurg 94:360–367. https://doi.org/10.1016/j.wneu.2016.07.030
Halkes PH, Wermer MJ, Rinkel GJ, Buskens E (2006) Direct costs of surgical clipping and endovascular coiling of unruptured intracranial aneurysms. Cerebrovasc Dis 22:40–45. https://doi.org/10.1159/000092336
Karsy M, Bowers CA, Scoville J, Kundu B, Atef M, Gee JM, Guan J, Couldwell WT (2018) Evaluation of complications and costs during overlapping transsphenoidal surgery in the treatment of pituitary adenoma. Neurosurgery 84:1104–1111. https://doi.org/10.1093/neuros/nyy269
Klimo P Jr, Kestle JR, MacDonald JD, Schmidt RH (2004) Marked reduction of cerebral vasospasm with lumbar drainage of cerebrospinal fluid after subarachnoid hemorrhage. J Neurosurg 100:215–224. https://doi.org/10.3171/jns.2004.100.2.0215
Moore JM, Adeeb N, Shallwani H, Gupta R, Patel AS, Griessenauer CJ, Youn R, Siddiqui A, Ogilvy CS, Thomas AJ (2017) A multicenter cohort comparison study of the safety, efficacy, and cost of ticagrelor compared to clopidogrel in aneurysm flow diverter procedures. Neurosurgery 81:665–671. https://doi.org/10.1093/neuros/nyx079
Qian C, Yu X, Chen J, Gu C, Wang L, Chen G, Dai Y (2016) Effect of the drainage of cerebrospinal fluid in patients with aneurismal subarachnoid hemorrhage: a meta-analysis. Medicine (Baltimore) 95:e5140. https://doi.org/10.1097/MD.0000000000005140
Radovanovic I, Abou-Hamden A, Bacigaluppi S, Tymianski M (2014) A safety, length of stay, and cost analysis of minimally invasive microsurgery for anterior circulation aneurysms. Acta Neurochir 156:493–503. https://doi.org/10.1007/s00701-013-1980-x
Rigante L, Moudrous W, de Vries J, Grotenhuis AJ, Boogaarts HD (2017) Operating room waste: disposable supply utilization in neurointerventional procedures. Acta Neurochir 159:2337–2340. https://doi.org/10.1007/s00701-017-3366-y
Shankar JJ, Vandorpe R, Pickett G, Maloney W (2013) SILK flow diverter for treatment of intracranial aneurysms: initial experience and cost analysis. J Neurointerv Surg 5(Suppl 3):iii11–iii15. https://doi.org/10.1136/neurintsurg-2012-010590
Silva NA, Shao B, Sylvester MJ, Eloy JA, Gandhi CD (2018) Unruptured aneurysms in the elderly: perioperative outcomes and cost analysis of endovascular coiling and surgical clipping. Neurosurg Focus 44(5):E4. https://doi.org/10.3171/2018.1.FOCUS17714
Sonig A, Shallwani H, Natarajan SK, Shakir HJ, Hopkins LN, Snyder KV, Siddiqui AH, Levy EI (2018) Better outcomes and reduced hospitalization cost are associated with ultra-early treatment of ruptured intracranial aneurysms: a US Nationwide Data Sample Study. Neurosurgery 82:497–505. https://doi.org/10.1093/neuros/nyx241
Stetler WR Jr, Griauzde J, Saadeh Y, Wilson TJ, Al-Holou WN, Chaudhary N, Thompson BG, Pandey AS, Gemmete JJ (2017) Is intensive care monitoring necessary after coil embolization of unruptured intracranial aneurysms? J Neurointerv Surg 9:756–760. https://doi.org/10.1136/neurintsurg-2016-012511
Twitchell S, Abou-Al-Shaar H, Reese J, Karsy M, Eli IM, Guan J, Taussky P, Couldwell WT (2018) Analysis of cerebrovascular aneurysm treatment cost: retrospective cohort comparison of clipping, coiling, and flow diversion. Neurosurg Focus 44(5):E3. https://doi.org/10.3171/2018.1.FOCUS17775
Wang C, Ching EC, Hui FK (2016) Aneurysm coil embolization: cost per volumetric filling analysis and strategy for cost reduction. J Neurointerv Surg 8:541–543. https://doi.org/10.1136/neurintsurg-2015-011696
Withers K, Carolan-Rees G, Dale M (2013) Pipeline embolization device for the treatment of complex intracranial aneurysms: a NICE Medical Technology Guidance. Appl Health Econ Health Policy 11:5–13. https://doi.org/10.1007/s40258-012-0005-x
Zhang X, Li L, Hong B, Xu Y, Liu Y, Huang Q, Liu J (2018) A systematic review and meta-analysis on economic comparison between endovascular coiling versus neurosurgical clipping for ruptured intracranial aneurysms. World Neurosurg 113:269–275. https://doi.org/10.1016/j.wneu.2018.02.078
Zhang X, Tang H, Huang Q, Hong B, Xu Y, Liu J (2018) Total hospital costs and length of stay of endovascular coiling versus neurosurgical clipping for unruptured intracranial aneurysms: systematic review and meta-analysis. World Neurosurg 115:393–399. https://doi.org/10.1016/j.wneu.2018.04.028
Acknowledgments
We thank Kristin Kraus for editorial assistance and Jacob Kresser for assistance with the VDO database.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Taussky is a consultant for Medtronic, Stryker Neurovascular, and Cerenovus. Dr. Grandhi is a consultant for Medtronic Neurovascular, Cerenovus, and BALT Neurovascular. The other authors report no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Vascular Neurosurgery - Aneurysm
Rights and permissions
About this article
Cite this article
Wilde, H., Twitchell, S., Reese, J. et al. Evaluation of disease severity and treatment intensity as cost drivers for ruptured intracranial aneurysms. Acta Neurochir 162, 157–167 (2020). https://doi.org/10.1007/s00701-019-04153-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-04153-3