Abstract
Background
Microsurgical clipping is a viable option for managing high-riding basilar apex aneurysms (BAXs) using a transsylvian approach. Cutting the posterior communicating artery (PCoA) at the perforator-free zone provides sufficient exposure of BAX, although it is not always safe. The aim was to qualitatively predict sectioning of the interfering PCoA by using preoperative computed tomographic angiography (CTA).
Methods
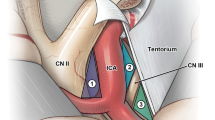
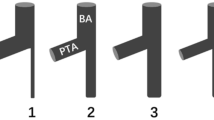
A virtual trajectory from the lesser sphenoid wing to the neck of the aneurysm was simulated on CTA in 19 consecutive patients operated on BAX aneurysms from 2013 to 2018. The angles on CTA resembled the typical view through the extended pterional craniotomy. Next, the ipsilateral PCoA was tracked from the internal carotid to its end at the posterior cerebral artery in the trajectory.
Results
The opticocarotid and carotid-oculomotor window served as the corridors for entering the interpeduncular fossa in 16 patients (84.2%) and in 3 patients (15.8%), respectively. The PCoA was intentionally cut during nine surgeries and preserved in 10 of them. The PCoA was cut more often when positioned toward the cranial base and more medially in the corridor; both the Kernel density analysis and the data points representing the position of the PCoA supported this finding (p < 0.01). The CTA-based position of either ends of the PCoA in the trajectory did not differ between cut and not-cut groups (p = 0.19–0.96). Aneurysm projection, rupture, size, PCoA diameter, length, and other distances on CTA were not related to the sectioning of PCoA (p > 0.05).
Conclusions
The probability of PCoA sectioning is higher when the PCoA is positioned medially and closer to the cranial base. If the anatomical course of the PCoA is recognized beforehand, it can contraindicate surgery. Preoperative CTA-based planning facilitates the surgery of BAX aneurysms. Therefore, CTA can make microsurgical clipping planning more predictable for the neurosurgeon and safer for the patient.







Similar content being viewed by others
References
Abecassis IJ, Sen RD, Barber J, Shetty R, Kelly CM, Ghodke BV, Hallam DK, Levitt MR, Kim LJ, Sekhar LN (2019) Predictors of recurrence, progression, and retreatment in basilar tip aneurysms: a location-controlled analysis. Oper Neurosurg 16(4):435–444
Beumer D, Delwel E-J, Kleinrensink G-J, Akouri S, Torres A, Krisht AF (2007) The perforator-free zone of the posterior communicating artery and its relevance in approaches to the interpeduncular cistern, especially the transcavernous approach: an anatomic study. Oper Neurosurg 61(5 Suppl 2):187–192
Brisman JL, Song JK, Newell DW (2006) Cerebral aneurysms. N Engl J Med 355(9):928–939
Drake CG, Peerless SJ, Hernesniemi JA (1996) Surgery of vertebrobasilar aneurysms. https://doi.org/10.1007/978-3-7091-9409-6
Dzierżanowski J, Szarmach A, Słoniewski P, Czapiewski P, Piskunowicz M, Bandurski T, Szmuda T (2014) The posterior communicating artery: morphometric study in 3D angio-computed tomography reconstruction. The proof of the mathematical definition of the hypoplasia. Folia Morphol (Warsz) 73(3):286–291
Henkes H, Fischer S, Mariushi W, Weber W, Liebig T, Miloslavski E, Brew S, Kühne D (2005) Angiographic and clinical results in 316 coil-treated basilar artery bifurcation aneurysms. J Neurosurg 103(6):990–999
Hernesniemi J, Ishii K, Niemelä M, Kivipelto L, Fujiki M, Shen H (2005) Subtemporal approach to basilar bifurcation aneurysms: advanced technique and clinical experience. Acta Neurochir Suppl 94:31–38
Higa T, Ujiie H, Kato K, Kamiyama H, Hori T (2009) Basilar artery trunk saccular aneurysms: morphological characteristics and management. Neurosurg Rev 32(2):181–191
Inao S, Kuchiwaki H, Hirai N, Gonda T, Furuse M (1996) Posterior communicating artery section during surgery for basilar tip aneurysm. Acta Neurochir 138(7):853–861
Krayenbühl N, Krisht AF (2007) Dividing the posterior communicating artery in approaches to the interpeduncular fossa: technical aspects and safety. Oper Neurosurg 61(5 Suppl 2):392–397
Krisht AF, Kadri PAS (2005) Surgical clipping of complex basilar apex aneurysms: a strategy for successful outcome using the pretemporal transzygomatic transcavernous approach. Neurosurgery 56(2 Suppl):261–273 discussion 261-73
Krisht AF, Krayenbühl N, Sercl D, Bikmaz K, Kadri PAS (2007) Results of microsurgical clipping of 50 high complexity basilar apex aneurysms. Neurosurgery 60(2):242–252
Lawton MT (2002) Basilar apex aneurysms: surgical results and perspectives from an initial experience. Neurosurgery 50(1):1–10
Lee J-S, Scerrati A, Zhang J, Ammirati M (2016) Quantitative analysis of surgical exposure and surgical freedom to the anterosuperior pons: comparison of pterional transtentorial, orbitozygomatic, and anterior petrosal approaches. Neurosurg Rev 39(4):599–605
Mardia KV (1972) A multi-sample uniform scores test on a circle and its parametric competitor. J R Stat Soc Ser B 34:102–113
Matsukawa H, Kamiyama H, Miyazaki T et al (2017) Surgical treatment of unruptured distal basilar artery aneurysm: durability and risk factors for neurological worsening. Acta Neurochir 159(9):1633–1642
Matsukawa H, Tanikawa R, Kamiyama H, Tsuboi T, Noda K, Ota N, Miyata S, Tokuda S (2015) Localization in the interpeduncular cistern as risk factors for the thalamoperforators’ ischemia, poor outcome, and oculomotor nerve palsy in patients with complex unruptured basilar apex aneurysm treated with neck clipping. World Neurosurg 84(2):475–482
Molyneux AJ, Kerr RSC, Yu L-M, Clarke M, Sneade M, Yarnold JA, Sandercock P (2005) International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and. Lancet 366(9488):809–817
Motoyama Y, Hironaka Y, Nishimura F et al (2017) Quantitative analysis of the trajectory of simulated basilar apex aneurysms through the internal carotid artery to assess the need for an orbitozygomatic approach. Acta Neurochir 159(1):85–92
Muhammad S, Tanikawa R, Lawton M, Regli L, Niemelä M, Korja M (2019) Microsurgical dissection of Sylvian fissure—short technical videos of third generation cerebrovascular neurosurgeons. Acta Neurochir 161(9):1743–1746
Nanda A, Sonig A, Banerjee AD, Javalkar VK (2014) Microsurgical management of basilar artery apex aneurysms: a single surgeon’s experience from Louisiana State University, Shreveport. World Neurosurg 82(1–2):118–129
Romani R, Elsharkawy A, Laakso A, Kangasniemi M, Hernesniemi J (2012) Complications of anterior clinoidectomy through lateral supraorbital approach. World Neurosurg 77(5–6):698–703
Sekhar LN, Tariq F, Morton RP, Ghodke B, Hallam DK, Barber J, Kim LJ (2013) Basilar tip aneurysms. Neurosurgery 72(2):284–299
Seng LB, Yamada Y, Rajagopal N, Mohammad AA, Teranishi T, Miyatani K, Kawase T, Kato Y (2018) Multimodality techniques in microsurgical clipping as the gold standard treatment in the management of basilar tip aneurysm: a case series. Asian J Neurosurg 13(4):1148–1157
Sharma M, Ahmed O, Ambekar S, Sonig A, Nanda A (2014) Factors predicting the oculomotor nerve palsy following surgical clipping of distal vertebrobasilar aneurysms: a single-institution experience. J Neurol Surg B Skull Base 75(4):261–267
Shi X, Qian H, Singh KCKI, Zhang Y, Zhou Z, Sun Y, Liu F (2013) Surgical management of vertebral and basilar artery aneurysms: a single center experience in 41 patients. Acta Neurochir 155(6):1087–1093
Słoniewski P, Dzierżanowski J, Szmuda T (2008) Modification of the pterional approach to pathologies of the interpeduncular fossa – technical description, morphometry, and results of treatment. Neurol Neurochir Pol 42(supl. 2):160–168
Spiessberger A, Strange F, Fandino J, Marbacher S (2018) Microsurgical clipping of basilar apex aneurysms: a systematic historical review of approaches and their results. World Neurosurg 114:305–316
Szmuda T, Sloniewski P (2011) Early and long-term outcome of surgically treated giant internal carotid artery aneurysms - comparison with smaller aneurysms. Acta Neurochir 153(8):1611–1619 discussion 1619
Tayebi Meybodi A, Benet A, Rodriguez Rubio R, Yousef S, Mokhtari P, Preul MC, Lawton MT (2018) Comparative analysis of orbitozygomatic and subtemporal approaches to the basilar apex: a cadaveric study. World Neurosurg 119:e607–e616
Teramoto S, Bertalanffy H (2016) Predicting the necessity of anterior communicating artery division in the bifrontal basal interhemispheric approach. Acta Neurochir 158(9):1701–1708
Tjahjadi M, Kivelev J, Serrone JC, Maekawa H, Kerro O, Jahromi BR, Lehto H, Niemelä M, Hernesniemi JA (2016) Factors determining surgical approaches to basilar bifurcation aneurysms and its surgical outcomes. Neurosurgery 78(2):181–191
Wiebers DO (2003) Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 362(9378):103–110
Yasargil MG, Antic J, Laciga R, Jain KK, Hodosh RM, Smith RD (1976) Microsurgical pterional approach to aneurysms of the basilar bifurcation. Surg Neurol 6(2):83–91
Yonekawa Y, Khan N, Imhof H-G, Roth P (2005) Basilar bifurcation aneurysms. Lessons learnt from 40 consecutive cases. Acta Neurochir Suppl 94:39–44
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical permission
For preparation of this and previous articles, the ethical approval was obtained in the institution (IRB Committee number: NKEBN/209/2008).
Informed consent
Informed consent for treatment and data processing was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Presentation at a conference: accepted for oral presentation in the upcoming WFNS Congress in Beijing, China, Sep 2019
This article is part of the Topical Collection on Vascular Neurosurgery - Aneurysm
Electronic supplementary material
ESM 1
(PDF 400 kb)
Rights and permissions
About this article
Cite this article
Szmuda, T., Słoniewski, P., Ali, S. et al. Can sectioning the posterior communicating artery be predicted with computed tomography angiography in the microsurgical clipping of basilar apex aneurysms?. Acta Neurochir 162, 567–579 (2020). https://doi.org/10.1007/s00701-019-04138-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-04138-2