Abstract
Background
Giant intracranial aneurysms of the posterior circulation (GPCirA) are rare entities compressing the brainstem and adjacent structures. Previous evidence has shown that the amount of brainstem shift away from the cranial base is not associated with neurological deficits. This raises the question whether other factors may be associated with neurological deficits.
Methods
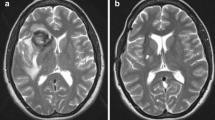
All data were extracted from the Giant Intracranial Aneurysm Registry, an international multicenter prospective study on giant intracranial aneurysms. We grouped GPCirA according to the mass effect on the brainstem (lateral versus medial). Brainstem compression was evaluated with two indices: (a) brainstem compression ratio (BCR) or diameter of the compressed brainstem to the assumed normal diameter of the brainstem and (b) aneurysm to brainstem ratio (ABR) or diameter of the aneurysm to the diameter of the compressed brainstem. We examined associations between neurological deficits and GPCirA characteristics using binary regression analysis.
Results
Twenty-eight GPCirA were included. Twenty GPCirA showed medial (71.4%) and 8 lateral compression of the brainstem (28.6%). Baseline characteristics did not differ between the groups for patient age, aneurysm diameter, aneurysm volume, modified Rankin Scale (mRS), motor deficit (MD), or cranial nerve deficits (CND). Mean BCR was 53.0 in the medial and 54.0 in the lateral group (p = 0.92). The mean ABR was 2.9 in the medial and 2.3 in the lateral group (p = 0.96).
In the entire cohort, neither BCR nor ABR nor GPCirA volumes were associated with the occurrence of CND or MD. In contrast, disability (mRS) was significantly associated with ABR (OR 1.94 (95% CI 1.01–3.70; p = 0.045) and GPCirA volumes (OR 1.21 (95% CI 1.01–1.44); p = 0.035), but not with BCR.
Conclusion
In this cohort of patients with GPCirA, neither the degree of lateral projection nor the amount of brainstem compression predicted neurological deficits. Disability was associated only with aneurysm volume. When designing treatment strategies for GPCirA, aneurysm laterality or the amount of brainstem compression should be viewed as less relevant while the high risk of rupture of such giant lesions should be emphasized.
Trial registration
The registry is listed at clinicaltrials.gov under the registration no. NCT02066493.





Similar content being viewed by others
References
Dengler J, Heuschmann PU, Endres M, Meyer B, Rohde V, Rufenacht DA, Vajkoczy P, Giant Intracranial Aneurysm Study Group (2011) The rationale and design of the Giant Intracranial Aneurysm Registry: a retrospective and prospective study. Int J Stroke Off J Int Stroke Soc 6(3):266–270
Dengler J, Maldaner N, Bijlenga P et al (2015) Perianeurysmal edema in giant intracranial aneurysms in relation to aneurysm location, size, and partial thrombosis. J Neurosurg 123(2):446–452
Dengler J, Maldaner N, Gläsker S, Endres M, Wagner M, Malzahn U, Heuschmann PU, Vajkoczy P, Giant Intracranial Aneurysm Study Group (2016) Outcome of surgical or endovascular treatment of giant intracranial aneurysms, with emphasis on age, aneurysm location, and unruptured aneuryms--a systematic review and meta-analysis. Cerebrovasc Dis Basel Switz 41(3–4):187–198
Durner G, Piano M, Lenga P et al (2018) Cranial nerve deficits in giant cavernous carotid aneurysms and their relation to aneurysm morphology and location. Acta Neurochir 160(8):1653–1660
Lenga P, Hohaus C, Hong B, et al (2018) Giant intracranial aneurysms of the posterior circulation and their relation to the brainstem: analysis of risk factors for neurological deficits. J Neurosurg 1–7
Simonet C, Arrese I, Sarabia R (2016) Giant posterior communicating artery aneurysm presenting as trigeminal neuralgia. J Stroke Cerebrovasc Dis Off J Natl Stroke Assoc 25(9):2243–2246
Wiebers DO, Whisnant JP, Huston J et al (2003) Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet Lond Engl 362(9378):103–110
Wostrack M, Mielke D, Kato N, Guhl S, Schmidt NO, Maldaner N, Vajkoczy P, Dengler J, Giant Intracranial Aneurysm Study Group (2015) Interobserver variability in the characterization of giant intracranial aneurysms with special emphasis on aneurysm diameter and shape. Acta Neurochir 157(11):1859–1865
Inamasu J, Suga S, Sato S, Onozuka S, Kawase T (2000) Long-term outcome of 17 cases of large-giant posterior fossa aneurysm. Clin Neurol Neurosurg 102(2):65–71
Kiyofuji S, Graffeo CS, Perry A, Murad MH, Flemming KD, Lanzino G, Rangel-Castilla L, Brinjikji W (2018) Meta-analysis of treatment outcomes of posterior circulation non-saccular aneurysms by flow diverters. J Neurointerventional Surg 10(5):493–499
Takahashi T (2002) The treatment of symptomatic unruptured aneurysms. Acta Neurochir Suppl 82:17–19
Saito H, Kuroda S, Terasaka S, Asano T, Nakayama N, Houkin K (2013) Reversible isolated accessory nerve palsy due to a large thrombosed vertebral aneurysm. Case Rep Neurol 5(2):135–139
Haley MD, Henderson DBH, Nowell M, Adams WM, Whitfield PC (2017) Giant vertebrobasilar aneurysm: a rare cause of central sleep apnoea. Br J Neurosurg 1–3
Yanagisawa T, Kinouchi H, Sasajima T, Shimizu H (2016) Long-term follow-up for a giant basilar trunk aneurysm surgically treated by proximal occlusion and external carotid artery to posterior cerebral artery bypass using a saphenous vein graft. J Stroke Cerebrovasc Dis 25(11):e212–e213
Bruneau M, George B (2010) Classification system of foramen magnum meningiomas. J Craniovertebral Junction Spine 1(1):10–17
Weisscher N, Vermeulen M, Roos YB, de Haan RJ (2008) What should be defined as good outcome in stroke trials; a modified Rankin score of 0-1 or 0-2? J Neurol 255(6):867–874
Peraio S, Ebner F, Tatagiba M (2018) Posterior fossa meningioma with invasion of the internal acoustic canal. Acta Neurochir 160(9):1823–1831
Funding
The Center for Stroke Research Berlin (no. CS-2009-12) provided financial support to the senior author (J.D.). This grant is exclusively dedicated to the maintenance of the Internet-based database.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee (Charité-Universitaetsmedizin Berlin) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Disclaimer
The sponsor had no role in the design or conduct of this research.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Comments
The major risk of giant aneurysms in the posterior circulation is the risk of rupture (50% in 5 years, cumulative). Unless the patient is in a medical condition which makes a treatment contraindicated, I believe all basilar tip giant aneurysms should be given the same level of attention and be treated if a reasonable clinical setting is present. The fact that a laterally projecting aneurysm or a degree of compression is not impacting C/N or motor function is not a legit criteria to delay or not to treat an unruptured giant aneurysm. This is a well-designed study on a small population and lacks treatment data. I encourage the authors to provide us with their updated information on what treatment modality is used in this population and whether the projection and compressive factors of the aneurysm could/should impact the treatment modality.
Amir Dehdashti
NY, USA
This research was carried out at the Department of Neurosurgery, Charité-Universitaetsmedizin Berlin, Germany.
This article is part of the Topical Collection on Vascular Neurosurgery - Aneurysm
Rights and permissions
About this article
Cite this article
Haemmerli, J., Lenga, P., Hong, B. et al. Clinical implications and radiographic characteristics of the relation between giant intracranial aneurysms of the posterior circulation and the brainstem. Acta Neurochir 161, 1747–1753 (2019). https://doi.org/10.1007/s00701-019-04016-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-04016-x