Abstract
Background
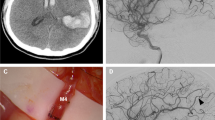
High-flow extracranial-intracranial bypass is associated with a significant risk of ischemic stroke. The goal of this study is to evaluate the effectiveness of STA-MCA bypass preceding a high-flow bypass as a means of protecting the brain from ischemia during the high-flow bypass anastomosis in patients with otherwise untreatable aneurysms.
Materials and method
This prospective study included 10 consecutive patients treated for complex/giant aneurysm using a previous combined STA-MCA bypass and high-flow EC-IC bypass between June 2016 and January 2018 when classical endovascular or microsurgical exclusion was estimated too risky. Early cranial Doppler, MRI, CT scan, and conventional angiography were performed in each patient to confirm patency of bypasses, measure flow in the anastomoses, detect any ischemic lesions, and evaluate exclusion of the aneurysm.
Results
The mean age at treatment was 55 years (range 34 to 67). The mean time of microsurgical procedure was 11 h (range 9 to 12). In all patients, the high-flow bypass was patent intraoperatively and complete occlusion of aneurysm was obtained. No ischemic lesions were noted on early MRI. One patient died from a large hemispheric infarction related to a common carotid artery dissection 10 days after the microsurgical procedure and immediate postoperative epidural hematoma was noted in one other patient.
Conclusion
In this study, we described the use of a protective STA-MCA bypass, performed prior to the high-flow bypass, in order to reduce the risk of perioperative ischemic lesions without increasing the morbidity of the surgical procedure. This treatment paradigm was feasible in all ten patients without complications related to the STA-MCA anastomosis.


Similar content being viewed by others
References
Bulsara KR, Patel T, Fukushima T (2008) Cerebral bypass surgery for skull base lesions: technical notes incorporating lessons learned over two decades. Neurosurg Focus 24:E11
Cantore G, Santoro A, Guidetti G, Delfinis CP, Colonnese C, Passacantilli E (2008) Surgical treatment of giant intracranial aneurysms: current viewpoint. Neurosurgery 63:279–289 discussion 289-290
Charbel FT, Meglio G, Amin-Hanjani S (2005) Superficial temporal artery-to-middle cerebral artery bypass. Neurosurgery 56:186–190 discussion 186-190
Cherian J, Srinivasan V, Kan P, Duckworth EAM (2018) Double-barrel superficial temporal artery-middle cerebral artery bypass: can it be considered “high-flow?”. Oper Neurosurg (Hagerstown) 14:288–294
Garrett MC, Komotar RJ, Starke RM, Merkow MB, Otten ML, Sciacca RR, Connolly ES (2009) The efficacy of direct extracranial-intracranial bypass in the treatment of symptomatic hemodynamic failure secondary to athero-occlusive disease: a systematic review. Clin Neurol Neurosurg 111:319–326
Gross BA, Du R (2012) STA-MCA bypass. Acta Neurochir 154:1463–1467
Guzman R, Lee M, Achrol A, Bell-Stephens T, Kelly M, Do HM, Marks MP, Steinberg GK (2009) Clinical outcome after 450 revascularization procedures for moyamoya disease. Clinical article. J Neurosurg 111:927–935
Ishikawa T, Montello DR (2006) Spatial knowledge acquisition from direct experience in the environment: individual differences in the development of metric knowledge and the integration of separately learned places. Cogn Psychol 52:93–129
Jafar JJ, Russell SM, Woo HH (2002) Treatment of giant intracranial aneurysms with saphenous vein extracranial-to-intracranial bypass grafting: indications, operative technique, and results in 29 patients. Neurosurgery 51:138–144 discussion 144-136
Kim BD, Ver Halen JP, Grant DW, Kim JY (2014) Anesthesia duration as an independent risk factor for postoperative complications in free flap surgery: a review of 1,305 surgical cases. J Reconstr Microsurg 30:217–226
Lagares A, Alen JF, Gomez PA, Lobato RD (2005) Grading of subarachnoid hemorrhage: modification of the World Federation of Neurosurgical Societies scale on the basis of data for a large series of patients. Neurosurgery 56:E873 author replyy E873
Lawton MT, Quinones-Hinojosa A, Sanai N, Malek JY, Dowd CF (2003) Combined microsurgical and endovascular management of complex intracranial aneurysms. Neurosurgery 52:263–274 discussion 274-265
Low SW, Teo K, Lwin S, Yeo LL, Paliwal PR, Ahmad A, Sinha AK, Teoh HL, Wong LY, Chong VF, Seet RC, Chan BP, Yeo TT, Chou N, Sharma VK (2015) Improvement in cerebral hemodynamic parameters and outcomes after superficial temporal artery-middle cerebral artery bypass in patients with severe stenoocclusive disease of the intracranial internal carotid or middle cerebral arteries. J Neurosurg 123:662–669
Mracek J, Holeckova I, Lavicka P, Mork J, Stepanek D, Struncova P, Cerveny V (2011) The impact of neuroprotection on brain metabolism during carotid endarterectomy. Cas Lek Cesk 150:489–493
Ono H, Inoue T, Tanishima T, Tamura A, Saito I, Saito N (2018) High-flow bypass with radial artery graft followed by internal carotid artery ligation for large or giant aneurysms of cavernous or cervical portion: clinical results and cognitive performance. Neurosurg Rev 41:655–665
Rankin J (1957) Cerebral vascular accidents in patients over the age of 60. II. Prognosis. Scott Med J 2:200–215
Sanai N, Zador Z, Lawton MT (2009) Bypass surgery for complex brain aneurysms: an assessment of intracranial-intracranial bypass. Neurosurgery 65:670–683 discussion 683
Sekhar LN, Natarajan SK, Ellenbogen RG, Ghodke B (2008) Cerebral revascularization for ischemia, aneurysms, and cranial base tumors. Neurosurgery 62:1373–1408 discussion 1408-1310
Sia SF, Lai L, Morgan MK (2013) Measuring competence development for performing high flow extracranial-to-intracranial bypass. J Clin Neurosci 20:1083–1088
Sidi A, Lobato EB, Cohen JA (2000) The American Society of Anesthesiologists' physical status: category V revisited. J Clin Anesth 12:328–334
Sun SJ, Zhang JJ, Li ZW, Xiong ZW, Wu XL, Wang S, Shu K, Chen JC (2016) Histopathological features of middle cerebral artery and superficial temporal artery from patients with moyamoya disease and enlightenments on clinical treatment. J Huazhong Univ Sci Technolog Med Sci 36:871–875
Takahashi A, Suzuki J, Sugawara T, Yoshimoto T (1986) Surgical treatment of AVMs occluding these feeders during removal--utilizing the intraoperative balloon catheter and brain protective substances (“Sendai cocktail”). No shinkei geka Neurol Surg 14:179–187
Tayebi Meybodi A, Huang W, Benet A, Kola O, Lawton MT (2017) Bypass surgery for complex middle cerebral artery aneurysms: an algorithmic approach to revascularization. J Neurosurg 127:463–479
Vajkoczy P, Korja M, Czabanka M, Schneider UC, Reinert M, Lehecka M, Schmiedek P, Hernesniemi J, Kivipelto L (2012) Experience in using the excimer laser-assisted nonocclusive anastomosis nonocclusive bypass technique for high-flow revascularization: Mannheim-Helsinki series of 64 patients. Neurosurgery 70:49–54 discussion 54-45
van Doormaal TP, van der Zwan A, Verweij BH, Langer DJ, Tulleken CA (2006) Treatment of giant and large internal carotid artery aneurysms with a high-flow replacement bypass using the excimer laser-assisted nonocclusive anastomosis technique. Neurosurgery 59:ONS328–ONS334 discussion ONS334-325
van Doormaal TP, van der Zwan A, Verweij BH, Regli L, Tulleken CA (2010) Giant aneurysm clipping under protection of an excimer laser-assisted non-occlusive anastomosis bypass. Neurosurgery 66:439–447 discussion 447
Wong AK, Joanna Nguyen T, Peric M, Shahabi A, Vidar EN, Hwang BH, Niknam Leilabadi S, Chan LS, Urata MM (2015) Analysis of risk factors associated with microvascular free flap failure using a multi-institutional database. Microsurgery 35:6–12
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Lille University Hospital/ Ethic committee) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Vascular Neurosurgery - Aneurysm
Rights and permissions
About this article
Cite this article
Aboukais, R., Verbraeken, B., Leclerc, X. et al. Protective STA-MCA bypass to prevent brain ischemia during high-flow bypass surgery: case series of 10 patients. Acta Neurochir 161, 1207–1214 (2019). https://doi.org/10.1007/s00701-019-03906-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-03906-4