Abstract
Background
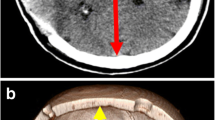
Decompressive craniectomy is a surgical way to treat intracranial hypertension, by removing a large flap of skull bone.
Method
We report the case of a 48 years old right-handed man presenting an acute ischaemic stroke of all the right sylvian artery area, with rapid clinic deterioration then coma. Severe intracranial hypertension was confirmed by transcranial Doppler. In emergency, we decided to perform a right-side decompressive craniectomy.
Conclusion
Six months later, he is in rehabilitation with “only” a left hemiplegia and a very good relational life. His modified Rankin score is 3. Decompressive craniectomy saved this patient’s life, that is why we think this surgical technique must be explained and mastered.




Similar content being viewed by others
References
Flint AC, Manley GT, Gean AD, Hemphill JC, Rosenthal G (2008) Post-operative expansion of hemorrhagic contusions after unilateral decompressive hemicraniectomy in severe traumatic brain injury. J Neurotrauma 25(5):503–512
Hutchinson PJ, Kolias AG, Timofeev IS, Corteen EA, Czosnyka M, Timothy J et al (2016) Trial of decompressive craniectomy for traumatic intracranial hypertension. N Engl J Med 375(12):1119–1130
Kakar V, Nagaria J, John Kirkpatrick P (2009) The current status of decompressive craniectomy. Br J Neurosurg 23(2):147–157
Kemmling A, Duning T, Lemcke L, Niederstadt T, Minnerup J, Wersching H et al (2010) Case report of MR perfusion imaging in sinking skin flap syndrome: growing evidence for hemodynamic impairment. BMC Neurol 10(1):80
Polin RS, Shaffrey ME, Bogaev CA, Tisdale N, Germanson T, Bocchicchio B et al (1997) Decompressive bifrontal craniectomy in the treatment of severe refractory posttraumatic cerebral edema. Neurosurgery. 41(1):84 92–discussion 92–4
Sedney CL, Julien T, Manon J, Wilson A (2014) The effect of craniectomy size on mortality, outcome, and complications after decompressive craniectomy at a rural trauma center. J Neurosci Rural Pract 5(3):212–217
Stiver SI (2009) Complications of decompressive craniectomy for traumatic brain injury. Neurosurg Focus 26(6):E7
Tagliaferri F, Zani G, Iaccarino C, Ferro S, Ridolfi L, Basaglia N et al (2012) Decompressive craniectomies, facts and fiction: a retrospective analysis of 526 cases. Acta Neurochir 154(5):919–926
Timofeev I, Santarius T, Kolias AG, Hutchinson PJA (2012) Decompressive craniectomy - operative technique and perioperative care. Adv Tech Stand Neurosurg 38:115–136
Vahedi K, Hofmeijer J, Juettler E, Vicaut E, George B, Algra A et al (2007) Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials. Lancet Neurol 6(3):215–222
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Key points:
- A multidisciplinary decision is needed, including the patient and/or family.
- Even if it seems not so complicated, anticipate anatomical pitfalls.
- Realise a large hair shearing, a large skin incision and a large bone flap.
- The dura mater must be widely opened.
- Haemostasis must be controlled.
- Do not forget to check the frontal sinus or petrosal bone.
- Protect the brain and facilitate cranioplasty by using an interlayer.
- Keep the hood loose, to avoid brain pressure through craniectomy.
- Time is brain, so try not to waste it.
- An early cranioplasty, within 3 months, is recommended to avoid CSF complications and to improve patient recovery.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurosurgery general
Electronic supplementary material
The case report patient and the video patient next of kin have consented to the submission of this case for submission to the journal.
Video 1
Decompressive craniectomy of a 48 years old man presenting a right malignant ischaemic stroke. (PPSX 263718 kb)
Rights and permissions
About this article
Cite this article
Desse, N., Beucler, N. & Dagain, A. How I do it: supra-tentorial unilateral decompressive craniectomy. Acta Neurochir 161, 895–898 (2019). https://doi.org/10.1007/s00701-019-03880-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-03880-x