Abstract
Background
A growing number of patients on anticoagulation or antiplatelet therapy (APT) are planned for elective surgery. The management of perioperative anticoagulation and APT is challenging because it must balance the risk of thromboembolism and bleeding, and specific recommendations for the management of bridging in neurosurgical patients are lacking. We surveyed German neurosurgical centers about their management of perioperative bridging of anticoagulation and APT to provide an overview of the current bridging policy.
Method
From April to August 2016, all German neurosurgical departments were invited to participate in the survey. We used SurveyMonkey to compose ten questions and to conduct the survey, and we defined three different approaches for the perioperative management of patients on a preexisting medication: medication will be discontinued (A) with perioperative “bridging” and (B) without perioperative bridging, or (C) medication will be continued perioperatively.
Results
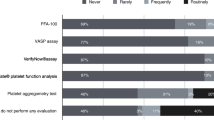
Out of 141 respondents, 84 (60%) partially and 77 (55%) fully completed the questionnaire. No defined policy for the perioperative management of anticoagulation and APT was established in 60.7% (51/84) of participating centers. The perioperative management of anticoagulation and APT varied widely among different centers in all items of the questionnaire; for example, in the group of patients at high risk for thromboembolism, acetylsalicylic acid was discontinued in 22%, bridged in 35%, and continued in 35% of centers.
Conclusions
There is significant uncertainty regarding the management of perioperative bridging of anticoagulation and APT in neurosurgery because of a lack of prospective and limited retrospective data.





Similar content being viewed by others
References
Baron TH, Kamath PS, McBane RD (2013) Management of antithrombotic therapy in patients undergoing invasive procedures. N Engl J Med 368(22):2113–2124
Cannegieter SC, Rosendaal FR, Briët E (1994) Thromboembolic and bleeding complications in patients with mechanical heart valve prostheses. Circulation 89(2):635–641
Capodanno D, Musumeci G, Lettieri C, Limbruno U, Senni M, Guagliumi G, Valsecchi O, Angiolillo DJ, Rossini R (2015) Impact of bridging with perioperative low-molecular-weight heparin on cardiac and bleeding outcomes of stented patients undergoing non-cardiac surgery. Thromb Haemost 114(2):423–431
Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, Gillum RF, Kim YH, McAnulty JH, Zheng ZJ, Forouzanfar MH, Naghavi M, Mensah GA, Ezzati M, Murray CJL (2014) Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation 129(8):837–847
Devereaux PJ, Mrkobrada M, Sessler DI, Leslie K, Alonso-Coello P, Kurz A, Villar JC, Sigamani A, Biccard BM, Meyhoff CS, Parlow JL, Guyatt G, Robinson A, Garg AX, Rodseth RN, Botto F, Lurati Buse G, Xavier D, Chan MTV, Tiboni M, Cook D, Kumar PA, Forget P, Malaga G, Fleischmann E, Amir M, Eikelboom J, Mizera R, Torres D, Wang CY, VanHelder T, Paniagua P, Berwanger O, Srinathan S, Graham M, Pasin L, Le Manach Y, Gao P, Pogue J, Whitlock R, Lamy A, Kearon C, Baigent C, Chow C, Pettit S, Chrolavicius S, Yusuf S (2014) Aspirin in patients undergoing noncardiac surgery. N Engl J Med 370(16):1494–1503
Douketis JD, Healey JS, Brueckmann M, Eikelboom JW, Ezekowitz MD, Fraessdorf M, Noack H, Oldgren J, Reilly P, Spyropoulos AC, Wallentin L, Connolly SJ (2015) Perioperative bridging anticoagulation during dabigatran or warfarin interruption among patients who had an elective surgery or procedure. Substudy of the RE-LY trial. Thromb Haemost 113(3):625–632
Douketis JD, Spyropoulos AC, Kaatz S, Becker RC, Caprini JC, Dunn AS, Garcia DA, Jacobson A, Jaffer AK, Kong DF, Schulman S, Turpie AGG, Hasselblad V, Ortel TL (2015) Perioperative bridging anticoagulation in patients with atrial fibrillation. N Engl J Med 373(9):823–833
Douketis JD, Spyropoulos AC, Spencer FA, Mayr M, Jaffer AK, Eckman MH, Dunn AS, Kunz R (2012) Perioperative management of antithrombotic therapy. Chest 141((2):e326S–e350S
Dunn AS, Spyropoulos AC, Turpie AGG (2007) Bridging therapy in patients on long-term oral anticoagulants who require surgery: the Prospective Peri-operative Enoxaparin Cohort Trial (PROSPECT). J Thromb Haemost 5(11):2211–2218
Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ (2001) Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA 285(22):2864–2870
Garcia D, Alexander JH, Wallentin L, Wojdyla DM, Thomas L, Hanna M, Al-Khatib SM, Dorian P, Ansell J, Commerford P, Flaker G, Lanas F, Vinereanu D, Xavier D, Hylek EM, Held C, Verheugt FWA, Granger CB, Lopes RD (2014) Management and clinical outcomes in patients treated with apixaban vs warfarin undergoing procedures. Blood 124(25):3692–3698
Hamilton MG, Yee WH, Hull RD, Ghali WA (2011) Venous thromboembolism prophylaxis in patients undergoing cranial neurosurgery: a systematic review and meta-analysis. Neurosurgery 68(3):571–581
Iorio A, Agnelli G (2000) Low-molecular-weight and unfractionated heparin for prevention of venous thromboembolism in neurosurgery: a meta-analysis. Arch Intern Med 160(15):2327–2332
Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ, Nelson ME, Wells PS, Gould MK, Dentali F, Crowther M, Kahn SR (2012) Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl):e419S–e496S
Lazio BE, Simard JM (1999) Anticoagulation in neurosurgical patients. Neurosurgery 45(4):838–47– discussion 847–8
Mittal R, Huggins NJ, Varma MK (2012) A59 A U.K. survey of neurosurgical practice for the pre-operative discontinuation of aspirin/clopidogrel. Eur J Anaesthesiol 29:S18
Palmer JD, Sparrow OC, Iannotti F (1994) Postoperative hematoma: a 5-year survey and identification of avoidable risk factors. Neurosurgery 35(6):1061–4– discussion 1064–5
Rachinger JC, Koman G, Scheller C, Prell J, Rampp S, Strauss C (2011) Practice in the perioperative prevention of deep vein thrombosis in German neurosurgical departments—is there a trend towards homogenization? Cen Eur Neurosurg 72(03):115–119
Rahman M, Donnangelo LL, Neal D, Mogali K, Decker M, Ahmed MM (2015) Effects of perioperative acetyl salicylic acid on clinical outcomes in patients undergoing craniotomy for brain tumor. World Neurosurgery 84(1):41–47
Sherwood MW, Douketis JD, Patel MR, Piccini JP, Hellkamp AS, Lokhnygina Y, Spyropoulos AC, Hankey GJ, Singer DE, Nessel CC, Mahaffey KW, Fox KAA, Califf RM, Becker RC (2014) Outcomes of temporary interruption of rivaroxaban compared with warfarin in patients with nonvalvular atrial fibrillation: results from the rivaroxaban once daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation (ROCKET AF). Circulation 129(18):1850–1859
Siegal D, Yudin J, Kaatz S, Douketis JD, Lim W, Spyropoulos AC (2012) Periprocedural heparin bridging in patients receiving vitamin K antagonists: systematic review and meta-analysis of bleeding and thromboembolic rates. Circulation 126(13):1630–1639
Skeith L, Lazo-Langner A, Kovacs MJ (2013) The equipoise of perioperative anticoagulation management: a Canadian cross-sectional survey. J Thromb Thrombolysis 37(4):411–413
Spyropoulos AC, Douketis JD (2012) How I treat anticoagulated patients undergoing an elective procedure or surgery. Blood 120(15):2954–2962
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The institutional ethics committee of the medical faculty of our university decided that approval was not necessary, because the survey questioned the current practice of anticoagulation and APT in neurosurgical centers but did not investigate patient-related data (327/2016A).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Comments
In my opinion, Skardelly and co-workers provide an interesting and important "survey of the management of perioperative bridging of anticoagulation and antiplatelet therapy" in German neurosurgical centers. The limitations of the study have been seen and adequately discussed by the authors, especially the fact that the study did not differentiate between therapeutic and low-dose bridging.
Marcus Reinges
Bremen, Germany
This article is part of the Topical Collection on Neurosurgery General
Electronic supplementary material
ESM 1
(PDF 162 kb)
Rights and permissions
About this article
Cite this article
Skardelly, M., Mönch, L., Roder, C. et al. Survey of the management of perioperative bridging of anticoagulation and antiplatelet therapy in neurosurgery. Acta Neurochir 160, 2077–2085 (2018). https://doi.org/10.1007/s00701-018-3679-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-018-3679-5