Abstract
Background
Giant cavernous carotid aneurysms (GCCAs) usually exert substantial mass effect on adjacent intracavernous cranial nerves. Since predictors of cranial nerve deficits (CNDs) in patients with GCCA are unknown, we designed a study to identify associations between CND and GCCA morphology and the location of mass effect.
Methods
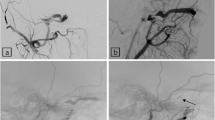
This study was based on data from the prospective clinical and imaging databases of the Giant Intracranial Aneurysm Registry. We used magnetic resonance imaging and digital subtraction angiography to examine GCCA volume, presence of partial thrombosis (PT), GCCA origins, and the location of mass effect. We also documented whether CND was present.
Results
We included 36 GCCA in 34 patients, which had been entered into the registry by eight participating centers between January 2009 and March 2016. The prevalence of CND was 69.4%, with one CND in 41.7% and more than one in 27.5%. The prevalence of PT was 33.3%. The aneurysm origin was most frequently located at the anterior genu (52.8%). The prevalence of CND did not differ between aneurysm origins (p = 0.29). Intracavernous mass effect was lateral in 58.3%, mixed medial/lateral in 27.8%, and purely medial in 13.9%. CND occurred significantly more often in GCCA with lateral (81.0%) or mixed medial/lateral (70.0%) mass effect than in GCCA with medial mass effect (20.0%; p = 0.03). After adjusting our data for the effects of the location of mass effect, we found no association between the prevalence of CND and aneurysm volume (odds ratio (OR) 1.30 (0.98–1.71); p = 0.07), the occurrence of PT (OR 0.64 (0.07–5.73); p = 0.69), or patient age (OR 1.02 (95% CI 0.95–1.09); p = 0.59).
Conclusions
Distinguishing between medial versus lateral location of mass effect may be more helpful than measuring aneurysm volumes or examining aneurysm thrombosis in understanding why some patients with GCCA present with CND while others do not.
Clinical trial registration no.
NCT02066493 (clinicaltrials.gov)

Similar content being viewed by others
References
Dengler J, Maldaner N, Bijlenga P, Burkhardt JK, Graewe A, Guhl S, Hong B, Hohaus C, Kursumovic A, Mielke D, Schebesch KM, Wostrack M, Rufenacht D, Vajkoczy P, Schmidt NO (1990) Perianeurysmal edema in giant intracranial aneurysms in relation to aneurysm location, size, and partial thrombosis. J Neurosurg 123:446–452
Dengler J, Maldaner N, Bijlenga P, Burkhardt JK, Graewe A, Guhl S, Nakamura M, Hohaus C, Kursumovic A, Schmidt NO, Schebesch KM, Wostrack M, Vajkoczy P, Mielke D (2015) Quantifying unruptured giant intracranial aneurysms by measuring diameter and volume—a comparative analysis of 69 cases. Acta Neurochir 157:361–368
Dolenc VV (1990) Surgery of vascular lesions of the cavernous sinus. Clin Neurosurg 36:240–255
Eddleman CS, Hurley MC, Bendok BR, Batjer HH (2009) Cavernous carotid aneurysms: to treat or not to treat? Neurosurg Focus 26:E4
Frosen J, Piippo A, Paetau A, Kangasniemi M, Niemelä M, Hernesniemi J, Jääskeläinen J (2004) Remodeling of saccular cerebral artery aneurysm wall is associated with rupture: histological analysis of 24 unruptured and 42 ruptured cases. Stroke 35:2287–2293
Hahn CD, Nicolle DA, Lownie SP, Drake CG (2000) Giant cavernous carotid aneurysms: clinical presentation in fifty-seven cases. J Neuroophthalmol 20:253–258
Harris FS, Rhoton AL (1976) Anatomy of the cavernous sinus. A microsurgical study. J Neurosurg 45:169–180
Heros RC (1984) Thromboembolic complications after combined internal carotid ligation and extra- to-intracranial bypass. Surg Neurol 21:75–79
Krings T, Alvarez H, Reinacher P, Ozanne A, Baccin CE, Gandolfo C, Zhao WY, Reinges MH, Lasjaunias P (2007) Growth and rupture mechanism of partially thrombosed aneurysms. Interv Neuroradiol 13:117–126
Kupersmith MJ, Hurst R, Berenstein A, Choi IS, Jafar J, Ransohoff J (1992) The benign course of cavernous carotid artery aneurysms. J Neurosurg 77:690–693
Linskey ME, Sekhar LN, Hirsch W Jr, Yonas H, Horton JA (1990) Aneurysms of the intracavernous carotid artery: clinical presentation, radiographic features, and pathogenesis. Neurosurgery 26:71–79
Nasr DM, Brinjikji W, Rouchaud A, Kadirvel R, Flemming KD, Kallmes DF (2016) Imaging characteristics of growing and ruptured vertebrobasilar non-saccular and dolichoectatic aneurysms. Stroke 47:106–112
Peschillo S, Caporlingua A, Resta MC, Peluso JPP, Burdi N, Sourour N, Diana F, Guidetti G, Clarençon F, Bloemsma GC, Di Maria F, Donatelli M, Resta M (2017) Endovascular treatment of large and giant carotid aneurysms with flow-diverter stents alone or in combination with coils: a multicenter experience and long-term follow-up. Oper Neurosurg (Hagerstown) 13:492–502
Puffer RC, Piano M, Lanzino G, Valvassori L, Kallmes DF, Quilici L, Cloft HJ, Boccardi E (2014) Treatment of cavernous sinus aneurysms with flow diversion: results in 44 patients. AJNR Am J Neuroradiol 35:948–951
Rosi Junior J, Welling LC, Yeng LT, Caldas JG, Schafranski M, Teixeira MJ, Figueiredo EG (2014) Cavernous carotid artery aneurysms: epidemiology, natural history, diagnostic and treatment. An experience of a single institution. Clin Neurol Neurosurg 125:32–35
Shimizu H, Matsumoto Y, Tominaga T (2010) Parent artery occlusion with bypass surgery for the treatment of internal carotid artery aneurysms: clinical and hemodynamic results. Clin Neurol Neurosurg 112:32–39
Stiebel-Kalish H, Kalish Y, Bar-On RH, Setton A, Niimi Y, Berenstein A, Kupersmith MJ (2005) Presentation, natural history, and management of carotid cavernous aneurysms. Neurosurgery 57:850–857
Tang X, Wu H, Wang B, Zhang N, Dong Y, Ding J, Dai J, Yu T, Pan L (2015) A new classification and clinical results of Gamma Knife radiosurgery for cavernous sinus hemangiomas: a report of 53 cases. Acta Neurochir 157:961–969
Tu YK, Tseng MY, Liu HM (2000) Experience in surgical management of tumours involving the cavernous sinus. J Clin Neurosci 7:419–424
Vasconcellos LP, Flores JA, Conti ML, Veiga JC, Lancellotti CL (2009) Spontaneous thrombosis of internal carotid artery: a natural history of giant carotid cavernous aneurysms. Arq Neuropsiquiatr 67:278–283
Wiebers DO, Whisnant JP, Huston J 3rd, Meissner I, Brown RD Jr, Piepgras DG, Forbes GS, Thielen K, Nichols D, O'Fallon WM, Peacock J, Jaeger L, Kassell NF, Kongable-Beckman GL, Torner JC (2003) Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 362:103–110
Acknowledgements
The authors would like to thank all members of the Giant Intracranial Aneurysm Group.
Funding
The Giant Intracranial Aneurysm Registry is funded by the Center for Stroke Research-Berlin (Grant No. CS-2009-12) to JD, the coordinating officer of the registry. The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript. Dr. Nima Etminan is a member of Medical monitor and steering committee NEWTON 2 and received Research grant PROTECT-U, which are unrelated to the present study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
AppendixMembers of the Giant Intracranial Aneurysm Study Group:
AppendixMembers of the Giant Intracranial Aneurysm Study Group:
P. Vajkoczy, P. Lenga, J. Dengler: Department of Neurosurgery, Charité – Universitaetsmedizin Berlin, Germany; M. Endres: Department of Neurology, Charité – Universitaetsmedizin Berlin, Germany; T. Liebig, G. Bohner, E. Wiener, H.C. Bauknecht: Department of Neuroradiology, Charité – Universitaetsmedizin Berlin, Germany; P.U. Heuschmann, K. Uttinger, U. Malzahn: Institute of Clinical Epidemiology and Biometry, University of Würzburg, Germany; J.-H. Klingler, S.Gläsker, J. Zentner, V. Van Velthoven: Department of Neurosurgery, University Hospital Freiburg, Germany; S. Guhl, H.W.S. Schroeder: Department of Neurosurgery, University of Greifswald, Germany; M. Strowitzki: Department of Neurosurgery, Trauma Center Murnau, Murnau, Germany; S. Eicker, B. Turowski: Department of Neurosurgery, University of Düsseldorf, Germany; N. Etminan, D. Haenggi: Department of Neurosurgery, University Hospital Mannheim, Germany; K.M. Schebesch, A. Brawanski: Department of Neurosurgery, University of Regensburg, Germany; K. Wrede, U. Sure: Department of Neurosurgery, University of Essen, Germany; N.O. Schmidt, J. Regelsberger, M. Westphal: Department of Neurosurgery, University Medical Center, Hamburg Eppendorf, Germany; D. Mielke, V. Rohde: Department of Neurosurgery, Georg-August-University Goettingen, Germany; H. Hosch, D. Moskopp: Department of Neurosurgery Vivantes-Klinikum im Friedrichshain, Berlin, Germany; C. Hohaus, H.J. Meisel: Department of Neurosurgery, BG-Clinic Bergmannstrost, Halle, Germany; M. Wostrack, B. Meyer, J. Lehmberg: Department of Neurosurgery, Technical University of Munich, Germany; O. Ganslandt, C. Musahl, N. Hopf: Department of Neurosurgery, Klinikum Stuttgart, Stuttgart, Germany; A. Graewe, U. Meier: Department of Neurosurgery, Unfallkrankenhaus Berlin, Germany; B. Hong, M. Nakamura, J. Krauss: Department of Neurosurgery, Hannover Medical School, Hannover, Germany; A. Grote, M. Simon, J. Schramm, E. Güresir, H. Vatter: Department of Neurosurgery, University Hospital Bonn, Bonn, Germany; A. Kursumovic, S.A. Rath: Department of Neurosurgery and Interventional Neuroradiology, Donau-Isar-Klinikum, Deggendorf, Germany; S. Marbacher, J. Fandino, M. Diepers: Department of Neurosurgery, Kantonsspital Aarau, Aarau, Switzerland; P. Familiari, A. Raco: Department of Neurosurgery, University of Rome ‘Sapienza’, Rome, Italy; P. Bijlenga, K. Schaller: Service de Neurochirurgie, Faculté de Médecine de Genève and Hôpitaux Universitaire de Genève, Switzerland; A. Gruber, W.T. Wang, E. Knosp: Department of Neurosurgery, Medical University Vienna, Vienna, Austria; K.T. Hoffmann, E. Boxhammer: Department of Neuroradiology, University of Leipzig, Leipzig, Germany; D.A. Rüfenacht, I. Wanke: Department of Neuroradiology, Klinik Hirslanden, Zurich, Switzerland; E. Boccardi, M. Piano: Department of Neuroradiology, Ospedale Niguarda Ca′ Granda, Milano, Italy; M. Niemelä, V. Nurminen, M. Lehecka, J. Hernesniemi: Department of Neurosurgery, Helsinki University Central Hospital, Helsinki, Finland; J.K. Burkhardt, O. Bozinov, N. Maldaner, L. Regli: Department of Neurosurgery, University Hospital of Zurich, Switzerland; O.D. Shekhtman, S.S. Eliava: Burdenko Neurosurgical Institute, Russian Academy of Medical Sciences, Moscow, Russia; N. Kato, K. Irie, K. Nishimura, S. Kaku, H. Arakawa, I. Yuki, T. Ishibashi, Y. Murayama: Department of Neurosurgery, Jikei University School of Medicine, Tokyo, Japan; I. Fiss, T. Kombos: Department of Spine Surgery and Neurosurgery, Helios Klinikum Hildesheim, Hildesheim, Germany; M.T. Pedro, R. König, R. Wirtz, G. Durner, V. Hagel: Department of Neurosurgery, University Hospital of Ulm, Germany; J. Helthuis, A. van der Zwan, T. van Doormaal: Department of Neurosurgery, University Medical Center Utrecht, Utrecht, Netherlands; C. Cognard, M. Gawlitza, A. Guenego: Department of Neuroradiology, Toulouse University Hospital, Toulouse, France; J. Walter, R. Kalff: Department of Neurosurgery, University Hospital Jena, Germany; J. Fiedler: Department of Neurosurgery, Budweis Hospital, Czech Republic; I. Linfante, D. Guilherme, KA. Starosciak: Interventional Neuroradiology and Endovascular Neurosurgery at Miami Cardiac and Vascular Institute and Baptist Neuroscience Institute, Miami, USA; MS. Miran, MFK. Suri: Department of Neurology University of Minnesota; Minnesota, USA.
Rights and permissions
About this article
Cite this article
Durner, G., Piano, M., Lenga, P. et al. Cranial nerve deficits in giant cavernous carotid aneurysms and their relation to aneurysm morphology and location. Acta Neurochir 160, 1653–1660 (2018). https://doi.org/10.1007/s00701-018-3580-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-018-3580-2