Abstract
Background
There are conflicting opinions regarding the optimal waiting time to perform surgery after rupture of supratentorial arteriovenous malformations (AVMs) to achieve the best possible outcome.
Objective
To analyze factors influencing outcomes for ruptured supratentorial AVMs after surgery, paying particular attention to the timing of the surgery.
Methods
We retrospectively investigated 59 patients admitted to our center between 2000 and 2014 for surgical treatment of ruptured supratentorial AVMs. We evaluated the effect of timing of surgery and other variables on the outcome at 2–4 months (early outcome), at 12 months (intermediate outcome) after surgery, and at final follow-up at the end of 2016 (late outcome).
Results
Age over 40 years (OR 18.4; 95% CI 1.9–172.1; p = 0.011), high Hunt and Hess grade (4 or 5) before surgery (OR 13.5; 95% CI 2.1–89.2; p = 0.007), hydrocephalus on admission (OR 12.9; 95% CI 1.8–94.4; p = 0.011), and over 400 cm3 bleeding during surgery (OR 11.5; 95% CI 1.5–86.6; p = 0.017) were associated with an unfavorable early outcome. Age over 40 years (OR 62.8; 95% CI 2.6–1524.9; p = 0.011), associated aneurysms (OR 34.7; 95% CI 1.4–829.9; p = 0.029), high Hunt and Hess grade before surgery (OR 29.2; 95% CI 2.6–332.6; p = 0.007), and over 400 cm3 bleeding during surgery (OR 35.3; 95% CI 1.7–748.7; p = 0.022) were associated with an unfavorable intermediate outcome. Associated aneurysms (OR 8.2; 95% CI 1.2–55.7; p = 0.031), high Hunt and Hess grade before surgery (OR 5.7; 95% CI 1.3–24.3; p = 0.019), and over 400 cm3 bleeding during surgery (OR 5.8; 95% CI 1.2–27.3; p = 0.027) were associated with an unfavorable outcome at last follow-up. Elapsed time between rupture and surgery did not affect early or final outcome.
Conclusions
Early surgery in patients with ruptured supratentorial arteriovenous malformation is feasible strategy, with late results comparable to those achieved with delayed surgery. Many other factors than timing of surgery play significant roles in long-term outcomes for surgically treated ruptured supratentorial AVMs.
Similar content being viewed by others
References
Abla AA, Rutledge WC, Seymour ZA, Guo D, Kim H, Gupta N, Sneed PK, Barani IJ, Larson D, McDermott MW, Lawton MT (2015) A treatment paradigm for high-grade brain arteriovenous malformations: volume-staged radiosurgical downgrading followed by microsurgical resection. J Neurosurg 122:419–432
Ajiboye N, Chalouhi N, Starke RM, Zanaty M, Bell R (2014) Cerebral arteriovenous malformations: evaluation and management. Sci World J 2014:649036
AlKhalili K, Chalouhi N, Tjoumakaris S, Rosenwasser R, Jabbour P (2014) Staged-volume radiosurgery for large arteriovenous malformations: a review. Neurosurg Focus 37:E20
Altay T (2012) Management of arteriovenous malformations related to Spetzler–Martin grading system. J Neurol Surg A Cent Eur Neurosurg 73:307–319
Andrews BT, Wilson CB (1987) Staged treatment of arteriovenous malformations of the brain. Neurosurgery 21:314–323
Beecher JS, Vance A, Lyon KA, Ban VS, McDougall CM, Whitworth LA, White JA, Samson DS, Batjer HH, Welch BG (2016) 359 delayed treatment of ruptured arteriovenous malformations: is it ok to wait? Neurosurgery 63(Suppl 1):206
Benifla M, Shelef I, Melamed I, Merkin V, Barrelly R, Cohen A (2010) Urgent removal of ruptured cerebral arteriovenous malformations in children. Harefuah 149:148–152 195
Bir SC, Maiti TK, Konar S, Nanda A (2016) Overall outcomes following early interventions for intracranial arteriovenous malformations with hematomas. J Clin Neurosci 23:95–100
Braksick SA, Fugate JE (2015) Management of brain arteriovenous malformations. Curr Treat Options Neurol 17:358
Brown RD Jr, Flemming KD, Meyer FB, Cloft HJ, Pollock BE, Link ML (2005) Natural history, evaluation, and management of intracranial vascular malformations. Mayo Clin Proc 80:269–281
Choi JH, Mast H, Sciacca RR, Hartmann A, Khaw AV, Mohr JP, Sacco RL, Stapf C (2006) Clinical outcome after first and recurrent hemorrhage in patients with untreated brain arteriovenous malformation. Stroke 37:1243–1247
Conger A, Kulwin C, Lawton MT, Cohen-Gadol AA (2015) Diagnosis and evaluation of intracranial arteriovenous malformations. Surg Neurol Int 6:76
Crawford PM, West CR, Chadwick DW, Shaw MD (1986) Arteriovenous malformations of the brain: natural history in unoperated patients. J Neurol Neurosurg Psychiatry 49:1–10
Crowley RW, Ducruet AF, McDougall CG, Albuquerque FC (2014) Endovascular advances for brain arteriovenous malformations. Neurosurgery 74(Suppl 1):S74–S82
Du R, Keyoung HM, Dowd CF, Young WL, Lawton MT (2007) The effects of diffuseness and deep perforating artery supply on outcomes after microsurgical resection of brain arteriovenous malformations. Neurosurgery 60:638–646 discussion 646-638
Graf CJ, Perret GE, Torner JC (1983) Bleeding from cerebral arteriovenous malformations as part of their natural history. J Neurosurg 58:331–337
Gross BA, Du R (2012) Rate of re-bleeding of arteriovenous malformations in the first year after rupture. J Clin Neurosci 19:1087–1088
Gross BA, Du R (2013) Natural history of cerebral arteriovenous malformations: a meta-analysis. J Neurosurg 118:437–443
Gross BA, Du R (2014) Diagnosis and treatment of vascular malformations of the brain. Curr Treat Options Neurol 16:279
Gross BA, Lai PM, Du R (2013) Hydrocephalus after arteriovenous malformation rupture. Neurosurg Focus 34:E11
Gross BA, Storey A, Orbach DB, Scott RM, Smith ER (2015) Microsurgical treatment of arteriovenous malformations in pediatric patients: the Boston Children’s Hospital experience. J Neurosurg Pediatr 15:71–77
Han PP, Ponce FA, Spetzler RF (2003) Intention-to-treat analysis of Spetzler–Martin grades IV and V arteriovenous malformations: natural history and treatment paradigm. J Neurosurg 98:3–7
Hartmann A, Mohr JP (2015) Acute management of brain arteriovenous malformations. Curr Treat Options Neurol 17:346
Hernesniemi J, Romani R, Lehecka M, Isarakul P, Dashti R, Celik O, Navratil O, Niemela M, Laakso A (2010) Present state of microneurosurgery of cerebral arteriovenous malformations. Acta Neurochir Suppl 107:71–76
Hernesniemi JA, Dashti R, Juvela S, Vaart K, Niemela M, Laakso A (2008) Natural history of brain arteriovenous malformations: a long-term follow-up study of risk of hemorrhage in 238 patients. Neurosurgery 63:823–829 discussion 829-831
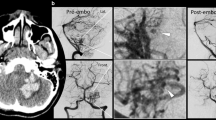
Iwama T, Yoshimura K, Keller E, Imhof HG, Khan N, Leblebicioglu-Konu D, Tanaka M, Valavanis A, Yonekawa Y (2003) Emergency craniotomy for intraparenchymal massive hematoma after embolization of supratentorial arteriovenous malformations. Neurosurgery 53:1251–1258 discussion 1258-1260
Jafar JJ, Rezai AR (1994) Acute surgical management of intracranial arteriovenous malformations. Neurosurgery 34:8–12 discussion 12-13
Kim H, Al-Shahi Salman R, McCulloch CE, Stapf C, Young WL, MARS Coinvestigators (2014) Untreated brain arteriovenous malformation: patient-level meta-analysis of hemorrhage predictors. Neurology 83:590–597
Kuhmonen J, Piippo A, Vaart K, Karatas A, Ishii K, Winkler P, Niemela M, Porras M, Hernesniemi J (2005) Early surgery for ruptured cerebral arteriovenous malformations. Acta Neurochir Suppl 94:111–114
Laakso A, Dashti R, Juvela S, Isarakul P, Niemela M, Hernesniemi J (2011) Risk of hemorrhage in patients with untreated Spetzler–Martin grade IV and V arteriovenous malformations: a long-term follow-up study in 63 patients. Neurosurgery 68:372–377 discussion 378
Laakso A, Dashti R, Juvela S, Niemela M, Hernesniemi J (2010) Natural history of arteriovenous malformations: presentation, risk of hemorrhage and mortality. Acta Neurochir Suppl 107:65–69
Laakso A, Hernesniemi J (2012) Arteriovenous malformations: epidemiology and clinical presentation. Neurosurg Clin N Am 23:1–6
Lawton MT, Du R, Tran MN, Achrol AS, McCulloch CE, Johnston SC, Quinnine NJ, Young WL (2005) Effect of presenting hemorrhage on outcome after microsurgical resection of brain arteriovenous malformations. Neurosurgery 56:485–493 discussion 485-493
Yasargil MG (1988) Microneurosurgery. In: Yaşargil MG (ed) vol IIIB, 2nd edn. George Thieme Verlag, Stuttgart, p 28
Martinez JL, Macdonald RL (2015) Surgical strategies for acutely ruptured arteriovenous malformations. Front Neurol Neurosci 37:166–181
Mast H, Young WL, Koennecke HC, Sciacca RR, Osipov A, Pile-Spellman J, Hacein-Bey L, Duong H, Stein BM, Mohr JP (1997) Risk of spontaneous haemorrhage after diagnosis of cerebral arteriovenous malformation. Lancet 350:1065–1068
Ondra SL, Troupp H, George ED, Schwab K (1990) The natural history of symptomatic arteriovenous malformations of the brain: a 24-year follow-up assessment. J Neurosurg 73:387–391
Pavesi G, Rustemi O, Berlucchi S, Frigo AC, Gerunda V, Scienza R (2009) Acute surgical removal of low-grade (Spetzler–Martin I-II) bleeding arteriovenous malformations. Surg Neurol 72:662–667
Peschillo S, Caporlingua A, Colonnese C, Guidetti G (2014) Brain AVMs: an endovascular, surgical, and radiosurgical update. ScientificWorldJournal 2014:834931
Pierot L, Cognard C, Spelle L (2004) Cerebral arteriovenous malformations: evaluation of the hemorrhagic risk and its morbidity. J Neuroradiol 31:369–375
Randell T (2010) Principles of neuroanesthesia in stroke surgery. Acta Neurochir Suppl 107:111–113
Ruiz-Sandoval JL, Cantu C, Barinagarrementeria F (1999) Intracerebral hemorrhage in young people: analysis of risk factors, location, causes, and prognosis. Stroke 30:537–541
Rutten-Jacobs LC, Maaijwee NA, Arntz RM, Schoonderwaldt HC, Dorresteijn LD, van Dijk EJ, de Leeuw FE (2014) Clinical characteristics and outcome of intracerebral hemorrhage in young adults. J Neurol 261:2143–2149
Signorelli F, Gory B, Pelissou-Guyotat I, Guyotat J, Riva R, Dailler F, Turjman F (2014) Ruptured brain arteriovenous malformations associated with aneurysms: safety and efficacy of selective embolization in the acute phase of hemorrhage. Neuroradiology 56:763–769
Soderman M, Andersson T, Karlsson B, Wallace MC, Edner G (2003) Management of patients with brain arteriovenous malformations. Eur J Radiol 46:195–205
Stapf C (2006) The neurology of cerebral arteriovenous malformations. Rev Neurol (Paris) 162:1189–1203
van Beijnum J, van der Worp HB, Buis DR, Al-Shahi Salman R, Kappelle LJ, Rinkel GJ, van der Sprenkel JW, Vandertop WP, Algra A, Klijn CJ (2011) Treatment of brain arteriovenous malformations: a systematic review and meta-analysis. JAMA 306:2011–2019
Wilkins RH (1985) Natural history of intracranial vascular malformations: a review. Neurosurgery 16:421–430
Yamada S, Takagi Y, Nozaki K, Kikuta K, Hashimoto N (2007) Risk factors for subsequent hemorrhage in patients with cerebral arteriovenous malformations. J Neurosurg 107:965–972
Yen CP, Varady P, Sheehan J, Steiner M, Steiner L (2007) Subtotal obliteration of cerebral arteriovenous malformations after gamma knife surgery. J Neurosurg 106:361–369
Young AM, Teo M, Martin SC, Phang I, Bhattacharya JJ, St George EJ (2015) The diagnosis and management of brain arteriovenous malformations in a single regional centre. World Neurosurg 84(6):1621–1628
Zhao J, Yu T, Wang S, Zhao Y, Yang WY (2010) Surgical treatment of giant intracranial arteriovenous malformations. Neurosurgery 67:1359–1370 discussion 1370
Funding
The Finnish government provided financial support (Finnish government grant for academic health research #TYH2017235). First author (A.H.) was awarded a scholarship for his PhD program from C. Ehmrooth Fellowship (Fondation de Luxembourg). The sponsors had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Comments
We have here a study from a renowned senior surgeon and an experienced group regarding early surgery approach to ruptured intracranial AVMs. The analysis is done on 59 patients culled from a total experience of 805 patients. It is a fractional sample of the overall group, but this is because careful steps were taken to ensure a complete dataset in analyzed patients. The data is instructive even though it is a small subset of the Helsinki AVM experience.
The raw data is impressive, no doubt because of the quality of this highly experienced team and center, and their ability to transfer patients quickly from throughout Finland. Mean time to surgery was 2 days. Complete excision at first surgery was achieved in 96% of patients. Mortality was 15%. Deep perforators, high Hunt-Hess grade before surgery (note that they have used Hunt and Hess grading for AVMs in the absence of a truly dedicated AVM hemorrhage acuity grading system), age over 40, hydrocephalus, amount of bleeding during surgery, and AVM-related aneurysms were associated with an increased likelihood of poor surgical outcomes. Importantly, neither time to surgery nor embolization before surgery were associated with significant differences in outcome.
This study impacts the practice of AVM surgery in several important ways. Unlike aneurysmal subarachnoid hemorrhage, in this series a policy of early AVM surgery is neither better nor worse than a policy of delayed surgery, except of course where life-threatening ICH and mass effect are present, and early surgery is thus mandated. The study also codifies that risk factors which AVM surgeons know intuitively to be negative predictors of outcome, like excessive bleeding, deep feeders, poor patient condition and the others outlined above, are validated by this analysis.
The only reservation about this paper is that of course this is a tiny subset of the extensive Helsinki experience. However, we can understand why they chose to do it this way, to obtain the best possible dataset, and we accept and recommend the article as a quality observation of many things, but especially that early AVM surgery is reasonable and can be associated with similar outcomes to delayed surgery if the team and facility is available and the surgeon elects this practice.
Christopher M. Loftus,
Philadelphia, PA, USA
Rights and permissions
About this article
Cite this article
Hafez, A., Oulasvirta, E., Koroknay-Pál, P. et al. Timing of surgery for ruptured supratentorial arteriovenous malformations. Acta Neurochir 159, 2103–2112 (2017). https://doi.org/10.1007/s00701-017-3315-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3315-9