Abstract
Background
Reports on outcome after multilobar resection (MLR) are scarce and most are retrospective single-centre studies or case studies with few patients. The aim of this study is to present seizure and complication outcomes 2 years after MLR in a prospective population-based series.
Method
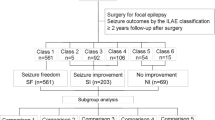
The Swedish National Epilepsy Surgery Registry (SNESUR) provides prospective population-based data on outcome and complications after epilepsy surgery. For this study, we have analysed data on seizure outcome and complications after MLR from the SNESUR between 1990 and 2013.
Results
Fifty-seven patients underwent MLR; 40/57 surgeries were performed between 1990 and 2000. Sixteen operations were classified as partial hemispherotomy. Resections were right-sided in 33 (58 %) patients. Mean age was 17.3 years (range, 0.3-63.4 years) and mean duration of epilepsy before surgery was 11.0 years (range, 0.2-37 years). Preoperative neurological deficits were seen in 19 patients (33.3 %). Learning disability (LD) was seen in 18 patients (31.6 %), six had severe LD (IQ <50). Seizure outcome after 2 years was available for 53 patients. Thirteen (24.5 %) were seizure-free and 12 (22.6 %) had >75 % seizure frequency reduction. Three (5.3 %) patients suffered major complications: infarction of the middle cerebral artery, epidural abscess and hemiparesis. Minor complications were seen in ten patients. There was no mortality.
Conclusions
This prospective, population-based study provides data on seizure outcome and complications after MLR. In selected patients MLR can be considered, but expectations for seizure freedom should not be too high and patients and parents should be counselled appropriately.

Similar content being viewed by others
References
Bjellvi J, Flink R, Rydenhag B, Malmgren K (2015) Complications of epilepsy surgery in Sweden 1996–2010: a prospective, population-based study. J Neurosurg 122:519–525
Bulacio JC, Jehi L, Wong C, Gonzalez-Martinez J, Kotagal P, Nair D, Najm I, Bingaman W (2012) Long-term seizure outcome after resective surgery in patients evaluated with intracranial electrodes. Epilepsia 53:1722–1730
Chugani HT, Asano E, Juhasz C, Kumar A, Kupsky WJ, Sood S (2014) “Subtotal” hemispherectomy in children with intractable focal epilepsy. Epilepsia 55:1926–1933
Cossu M, Lo Russo G, Francione S, Mai R, Nobili L, Sartori I, Tassi L, Citterio A, Colombo N, Bramerio M, Galli C, Castana L, Cardinale F (2008) Epilepsy surgery in children: results and predictors of outcome on seizures. Epilepsia 49:65–72
D'Agostino MD, Bastos A, Piras C, Bernasconi A, Grisar T, Tsur VG, Snipes J, Juhasz C, Chugani H, Guerrini R, Cross H, Andermann E, Dubeau F, Montes J, Olivier A, Andermann F (2004) Posterior quadrantic dysplasia or hemi-hemimegalencephaly: a characteristic brain malformation. Neurology 62:2214–2220
Daniel RT, Meagher-Villemure K, Farmer JP, Andermann F, Villemure JG (2007) Posterior quadrantic epilepsy surgery: technical variants, surgical anatomy, and case series. Epilepsia 48:1429–1437
Delalande O, Bulteau C, Dellatolas G, Fohlen M, Jalin C, Buret V, Viguier D, Dorfmuller G, Jambaque I (2007) Vertical parasagittal hemispherotomy: surgical procedures and clinical long-term outcomes in a population of 83 children. Neurosurgery 60:ONS19-ONS32, discussion ONS32
Elsharkawy AE, Behne F, Oppel F, Pannek H, Schulz R, Hoppe M, Pahs G, Gyimesi C, Nayel M, Issa A, Ebner A (2008) Long-term outcome of extratemporal epilepsy surgery among 154 adult patients. J Neurosurg 108:676–686
Elsharkawy AE, Pannek H, Schulz R, Hoppe M, Pahs G, Gyimesi C, Nayel M, Issa A, Ebner A (2008) Outcome of extratemporal epilepsy surgery experience of a single center. Neurosurgery 63:516–525, discussion 525–516
Eriksson S, Malmgren K, Rydenhag B, Jonsson L, Uvebrant P, Nordborg C (1999) Surgical treatment of epilepsy—clinical, radiological and histopathological findings in 139 children and adults. Acta Neurol Scand 99:8–15
Hemb M, Velasco TR, Parnes MS, Wu JY, Lerner JT, Matsumoto JH, Yudovin S, Shields WD, Sankar R, Salamon N, Vinters HV, Mathern GW (2010) Improved outcomes in pediatric epilepsy surgery: the UCLA experience, 1986–2008. Neurology 74:1768–1775
Jayakar P, Dunoyer C, Dean P, Ragheb J, Resnick T, Morrison G, Bhatia S, Duchowny M (2008) Epilepsy surgery in patients with normal or nonfocal MRI scans: integrative strategies offer long-term seizure relief. Epilepsia 49:758–764
Korkman M, Granstrom ML, Kantola-Sorsa E, Gaily E, Paetau R, Liukkonen E, Boman PA, Blomstedt G (2005) Two-year follow-up of intelligence after pediatric epilepsy surgery. Pediatr Neurol 33:173–178
Malmgren K, Olsson I, Engman E, Flink R, Rydenhag B (2008) Seizure outcome after resective epilepsy surgery in patients with low IQ. Brain 131:535–542
Paolicchi JM, Jayakar P, Dean P, Yaylali I, Morrison G, Prats A, Resnik T, Alvarez L, Duchowny M (2000) Predictors of outcome in pediatric epilepsy surgery. Neurology 54:642–647
Rydenhag B, Silander HC (2001) Complications of epilepsy surgery after 654 procedures in Sweden, September 1990–1995: a multicenter study based on the Swedish National Epilepsy Surgery Register. Neurosurgery 49:51–56, discussion 56–57
Sarkis RA, Jehi L, Najm IM, Kotagal P, Bingaman WE (2012) Seizure outcomes following multilobar epilepsy surgery. Epilepsia 53:44–50
Tellez-Zenteno JF, Dhar R, Wiebe S (2005) Long-term seizure outcomes following epilepsy surgery: a systematic review and meta-analysis. Brain 128:1188–1198
Wiebe S, Blume WT, Girvin JP, Eliasziw M (2001) A randomized, controlled trial of surgery for temporal-lobe epilepsy. N Engl J Med 345:311–318
Wieser HG, Blume WT, Fish D, Goldensohn E, Hufnagel A, King D, Sperling MR, Luders H, Pedley TA, Commission on Neurosurgery of the International League Against Epilepsy (ILAE) (2001) ILAE Commission Report. Proposal for a new classification of outcome with respect to epileptic seizures following epilepsy surgery. Epilepsia 42:282–286
Wyllie E, Comair YG, Kotagal P, Bulacio J, Bingaman W, Ruggieri P (1998) Seizure outcome after epilepsy surgery in children and adolescents. Ann Neurol 44:740–748
Wyllie E, Lachhwani DK, Gupta A, Chirla A, Cosmo G, Worley S, Kotagal P, Ruggieri P, Bingaman WE (2007) Successful surgery for epilepsy due to early brain lesions despite generalized EEG findings. Neurology 69:389–397
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Sahlgrenska Academy, University of Gothenburg through the LUA/ALF agreement. Grant, ALFGBG137431; recipient, Prof. Kristina Malmgren. The sponsor had no role in the design or conduct of this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organisation or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Additional information
Comment
The authors present with their manuscript an analysis of patient outcome after multilobar resection for epilepsy in Sweden. Only surgeries in the years 1990–2013 were included. This manuscript is based on data of the Swedish National Epilepsy Registry. A total of 57 procedures was included with most procedures been done in the first decade. Twenty-four-point-five-percent of the patient became seizure-free, 22.6 % experienced a significant reduction of seizure frequency. Complication rate reached 20 % with three major complications with permanent deficits. The authors conclude that MLR can be considered in selected patients, but expectations for seizure freedom should not be too high and patients and parents should be counselled appropriately. Although the case number is small, this is a rather large case series for multilobar resection in epilepsy. Since this is a very rare indication, all experiences should be published. Particularly since it is a registry based analysis, significant bias with interpretation of the results can be excluded. Overall the data are further discouraging and support the trend that the number of multilobar resections are declining. So in all, the indication for these procedures has to be highly selective.
Joachim Oertel
Homburg-Saar, Germany
Rights and permissions
About this article
Cite this article
Nilsson, D.T., Malmgren, K., Flink, R. et al. Outcomes of multilobar resections for epilepsy in Sweden 1990–2013: a national population-based study. Acta Neurochir 158, 1151–1157 (2016). https://doi.org/10.1007/s00701-016-2807-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-2807-3